Health, Social Care and Sport Committee
ADHD and autism pathways and support
Membership changes
The following changes to Committee membership occurred during the course of this inquiry:
On 21 May 2025, Patrick Harvie MSP replaced Gillian Mackay MSP as a member of the Committee.
On 17 December 2025, Gillian Mackay MSP replaced Patrick Harvie MSP as a member of the Committee.
Summary of recommendations
Accessing pathways to support
The Committee notes with concern the evidence it has heard about the lack of pathways to support for adults, and for children without co-occuring mental health conditions in some health board areas, and the confusion inconsistencies in available pathways across Scotland can cause for individuals and their families.
The Committee welcomes the Scottish Government's commitment to accept the recommendations set out in NAIT's Adult Neurodevelopmental Pathways report, including the development and implementation of guidance for adult pathways in all HSCPs across Scotland, and to review the implementation of the National Neurodevelopmental Specification for Children and Young People through its new task force.
At the same time, the Committee calls on the Scottish Government to take urgent action to develop and implement a national plan to give adults and children with autism and ADHD across all health boards in Scotland access to clear and consistent pathways to support. This should include continuing to work with NAIT and health boards to implement the recommendations from the pathfinder pilots and delivering an updated Specification for children's pathways.
Treatment thresholds and gatekeeping
The Committee recognises that the scale of demand for neurodevelopmental assessments has made it necessary to put certain thresholds in place before a referral is made and that this has resulted in gatekeeping access to assessments in some areas.
However, the Committee has been concerned to hear evidence that many people feel those responsible for referrals and gatekeeping do not have an accurate, up to date understanding of neurodevelopmental conditions and how they present, particularly in women, girls and ethnic minority people, meaning that thresholds may not be applied fairly or appropriately in some cases.
The Committee is further concerned that an over-reliance on threshold setting and gatekeeping risks resulting in many individuals being unable to access the support they need at the appropriate time, leading to a situation where these individuals will then present themselves at a later stage having reached a state of crisis, which can be considerably more difficult and costly to treat. The Committee concludes that, although perhaps understandable when trying to deal with consistently high demand, such an approach to managing access to pathways risks being counterproductive in the longer term.
The Committee therefore calls on the Scottish Government, in responding to this report, to set out how it intends to address this challenge and to ensure Health Boards shift their focus to a progressive approach which ensures the provision of treatment and support for autistic people and/or people with ADHD at the earliest opportunity, in line with the principles of its Population Health Framework.
The Committee further recommends that the Scottish Government takes action to ensure improved consistency and timeliness across Scotland of access to treatment and support, including an assessment or diagnosis where appropriate.
To further improve quality and consistency, the Committee calls on the Scottish Government to develop a plan to deliver mandatory training to all those who are involved in making referrals to neurodevelopmental pathways. This training should:
be developed in collaboration with people with neurodevelopmental conditions
draw from existing resources already developed by NES, NAIT and in health board areas where appropriate
be monitored and reported on to determine rates of uptake.
More broadly, the Committee recommends a programme of mandatory training on neurodevelopmental conditions for all health and social care staff in patient-facing roles.
Open referral
The Committee notes concerns from many healthcare practitioners that broader application of an open referrals model for accessing ADHD and autism pathways would create a risk of "opening the floodgates" to even greater demand and a rise in inappropriate referrals that would be liable to overwhelm services.
At the same time, the Committee notes a strong desire from many individuals to have the option of open referral available to them. It further notes evidence from certain areas where an open referral model is already in place which suggests concerns about services being overwhelmed are not borne out by experience on the ground. Instead, there is strong evidence to suggest an open referral model can help pathways and services to operate more efficiently and responsively.
The Committee therefore calls on the Scottish Government, in responding to this report, to set out what further action it is taking or plans to take to gather further data about the practical impact and any specific benefits for pathways and services of allowing open referrals, to learn appropriate lessons from experience of open referrals on the ground and to explore how open referrals can be made more widely available across Scotland in a way that allays workforce fears that this will result in services being overwhelmed.
Beyond this, the Committee would encourage the Scottish Government to explore how, in future, processes for open referral can be better integrated into national standards for ADHD and autism pathways and support.
Waiting times
The Committee has been extremely concerned to hear evidence during this inquiry of many individuals having to wait many years on a waiting list for assessment for ADHD, autism and other neurodevelopmental conditions, as well as evidence from many areas where waiting lists have now been closed. It is firmly of the view that, as well as being detrimental to the individuals affected, such a situation is damaging to wider society to which, for as long as they fail to receive the support and treatment they need, these individuals may be prevented from making an active and positive contribution.
The Committee acknowledges evidence of an unprecedented rise in demand for neurodevelopmental assessments in recent years. It has been persuaded by evidence that this rise is not attributable to a tendency towards over-diagnosis but rather to an historic under-diagnosis of ADHD and autism and an improved understanding of these conditions more recently. The Committee is also sympathetic to the suggestion that promoting a narrative around over-diagnosis is unhelpful and risks further stigmatising those with autism and/or ADHD, with the result that their condition is not believed or understood and they are denied access to the pathways and support they need.
Given the current length of waiting times, the Committee believes it is particularly crucial that the quality of communication with those on waiting lists is consistently high, that available information is accurate, supportive and up-to-date, uses neuro-affirming language and is delivered in a way that is responsive to the specific needs of those with autism and/or ADHD.
For the same reason, the Committee calls on the Scottish Government to give much greater attention, including the commitment of appropriate resources, to the development of "waiting well" initiatives that provide suitably targeted access to good information and local support as a consistent and integral part of the waiting process for those on neurodevelopmental pathways.
The Committee welcomes the Scottish Government's establishment of a task force and its commitment of additional funding to support implementation of the National Neurodevelopmental Specification. As part of this work, the Committee calls on the Scottish Government to produce a roadmap setting out clear timelines for improvement of ADHD and autism pathways and support. This should address improvements to information and communication (including the potential establishment of a 'one stop shop'), improved access to local support while waiting, the roll-out of targeted "waiting well" initiatives and the commitment of funding to develop the multi-disciplinary workforce needed to reduce waiting times in the longer term.
Assessment process
The Committee calls on the Scottish Government, in close collaboration with health boards, to undertake a comprehensive review of the assessment process in all areas with a view to developing a National Standard for assessments that guarantees consistency of access, responsiveness and support throughout Scotland. In particular, this review and the resulting National Standard should address:
ensuring diagnostic criteria used in assessments are appropriate and up-to-date;
a presumption against the use of single condition assessments, given the high rate of co-occurrence of ADHD and autism (as well as other neurodevelopmental conditions and other mental and physical health problems) and the active promotion instead of the use of holistic assessments;
the development of guidelines to establish clear qualification requirements for those carrying out neurodevelopmental assessments;
Promoting the direct involvement of individuals with lived experience of neurodevelopmental conditions in helping and supporting others to navigate the assessment process;
clear guidance for the use of alternative approaches to assessment such as "whole school" approaches, "stepped care" and "consensus diagnosis" - to include details of the circumstances in which such alternative approaches may be more appropriate than traditional approaches to assessment;
promotion of a multi-disciplinary approach to assessment, including requirements for members of multi-disciplinary teams to undergo continuous professional development and training on providing neurodevelopmental assessments, to include regular updates in neuro-affirming practice.
To ensure the review and resulting National Standard are as responsive as possible to the needs of those seeking an assessment, the Committee calls on the Scottish Government to ensure individuals with lived experience of neurodevelopmental conditions and the community groups that support them, are actively involved in the review process.
The Committee also believes there should be a requirement on health boards to work with the National Autism Implementation Team to ensure updated service specifications for provision of services are successfully implemented, both for children and young people and for adults.
Diagnosis
The Committee acknowledges there are a number of valid reasons for seeking a diagnosis for autism and/or ADHD, including:
Giving individuals a sense of validation and understanding about themselves as people, including understanding current and past life experiences
Determining what forms of support, adjustments or treatment would be most helpful and giving individuals and/or parents and carers the ability to advocate for these.
At the same time, the Committee also acknowledges fundamental differences between these conditions which mean the reasons for seeking a diagnosis will vary between autism and ADHD. In particular, the Committee notes that, as a medically treatable condition, there are especially important reasons for receiving a positive diagnosis for ADHD since this will ensure the individuals affected are able to access the correct medication to treat their condition.
While welcoming the Scottish Government's recognition of the importance of diagnosis while committing itself to ensuring receiving a diagnosis is not a prerequisite for accessing support, the Committee remains concerned that, in reality, the lack of a formal diagnosis has become a barrier to accessing support for too many individuals.
The Committee therefore calls on the Scottish Government, in responding to this report, to set out what action it is taking or plans to take to ensure the lack of a formal diagnosis is not used as an artificial barrier to accessing support and to encourage practitioners to fully explore what support can be made available while individuals are waiting to receive a formal diagnosis.
The Committee highlights the particularly urgent need for formal diagnosis for those individuals who require it to be able to access the correct medication to treat their condition. It therefore calls on the Scottish Government to set out what strategies it is pursuing to reduce waiting times for assessment and diagnosis of these individuals.
Private diagnosis and 'shared care'
The Committee has been concerned to hear evidence of many individuals being forced to seek a private diagnosis, often at significant financial cost, due to long waiting times for accessing neurodevelopmental assessment and diagnosis via the NHS. The Committee is particularly concerned that this risks creating a two-tier system where timely access to diagnosis is based on an individual's ability to pay.
The Committee has been similarly concerned to hear evidence that the quality of assessments and diagnoses acquired privately can be variable. The Committee therefore urges the Scottish Government, in responding to this report, to set out what action it is taking or plans to take to promote a level playing field in standards of assessment and diagnosis across the public and private sectors.
The Committee further notes the negative experiences of many individuals, having acquired a private diagnosis, of getting their GP to recognise that diagnosis or to agree to provide "shared care". The Committee recognises that greater reliability of standards for assessment and diagnosis, whether provided privately or through the NHS, are needed to give GPs the confidence to accept "shared care" agreements.
The Commitee also recognises that, until NHS capacity is significantly expanded, individuals seeking private assessment and diagnosis is likely to be an ongoing fact of life. In these circumstances, it calls on the Scottish Government to work with Healthcare Improvement Scotland, health boards and GPs to address problems with shared care agreements and to develop a more consistent approach to their use.
Transitions
The Committee recognises the particular importance of well managed transitions for people with neurodevelopmental conditions but regrets that too many report experiences of poorly managed transitions and a lack of appropriate support during transitional periods in their lives.
The Committee highlights evidence of particular challenges for people with neurodevelopmental conditions in making the transition from child to adult services at a particularly vulnerable stage of their lives - and the crucial importance of maintaining consistent relationships during this period to be able to successfully navigate this transition. The Committee has also heard similarly concerning evidence of poor planning and support for children with neurodevelopmental conditions in making the transition from primary to secondary school and from education to post-education settings.
In light of this evidence, the Committee calls on the Scottish Government, in responding to this report, to set out what action it is taking to ensure proper implementation of its Principles of Transition policy, GIRFEC policy and guidance and the relevant provisions of the National Neurodevelopmental Specification, so that people with neurodevelopmental conditions do not experience any further negative effects from poorly planned and supported transitions.
In so doing, the Committee further calls on the Scottish Government to address an apparent gap in the National Neurodevelopmental Specification for Children and Young People by ensuring there is absolute continuity of care throughout these important transitions and into adulthood.
The Committee pays particular tribute to the work of third sector organisations in supporting people with neurodevelopmental conditions during periods of transition and calls on the Scottish Government, in responding to this report, to set out what it is doing to support third sector organisations operating in this space.
Role of third sector
The Committee pays tribute to the crucial work of third sector organisations in providing support to those people with ADHD and autism who have not received or are yet to receive a formal assessment or diagnosis from statutory services. It notes that, without access to such support, many individuals would be left isolated and unsupported.
The Committee further commends the work of the third sector in involving people with lived experience of neurodevelopmental conditions in delivering the support it provides - and notes how much their involvement is welcomed by individuals using these services.
Given how crucial third sector support can be in this area, the Committee welcomes the Scottish Government's ongoing commitment to supporting third sector organisations through vehicles such as the Autistic Adult Support Fund. It calls on the Scottish Government, in responding to this report, to set out what further actions it plans to take to continue to support the third sector and to place funding for third sector organisations on a more sustainable long-term footing.
Whole society approach
The Committee highlights the broad range of evidence it has heard throughout this inquiry in support of a whole society approach as the most effective means, longer term, of supporting people with neurodevelopmental conditions, improving wider public awareness and combatting stigma.
In this context, the Committee welcomes the Scottish Government's commitment that its new task force will take a whole-systems approach, working across the health and education sectors to implement the National Neurodevelopmental Specification.
Beyond this, the Committee calls on the Scottish Government, in responding to this report, to set out what actions it will take to further promote a whole-systems or whole society approach, including:
learning the requisite lessons and developing associated guidance from examples of best practice in whole systems approaches, such as that seen in NHS Ayrshire and Arran;
what, if any, steps it intends to take towards developing a national workforce plan as an important component of a whole-systems approach;
how distribution of funding will be adapted in future to facilitate a more integrated, cross-sectoral approach to support;
promoting educational settings that are more inclusive of people with neurodevelopmental conditions;
addressing the particular needs of families with multiple family members who are living with neurodevelopmental conditions; and
promoting closer collaboration between the various different public services people with neurodevelopmental conditions come into contact with.
The Committee has heard evidence from many contributors to the inquiry who have expressed regret that the Scottish Government has paused plans for a Learning Disabilities, Autism and Neurodivergence Bill, which it was felt would contribute positively towards promoting a whole systems or whole society approach to supporting people with neurodevelopmental conditions. The Committee notes the Minister's commitment, in the absence of further progress on a Bill, to publish draft provisions. It calls on the Scottish Government, in responding to this report, to set out a timetable for publication and to provide further details of what these might cover.
Data
The Committee highlights the importance of consistent, reliable, high quality data on neurodevelopmental referrals and waiting times across Scotland to be able to plan services effectively and to make ongoing improvements.
In this context, the Committee has been concerned to hear evidence of significant gaps and a lack of standardisation in data gathering, including across NHS Boards.
The Committee therefore calls on the Scottish Government to set out what steps it plans to take to enable routine quarterly reporting of data on referrals and waiting times for autism and ADHD, underpinned by national guidance.
While welcoming that this will be an area of longer term focus for the new Scottish Government task force, the Committee further calls on the Scottish Government to address how it intends to overcome potential barriers to more consistent data collection and reporting, such as use of different software systems and location of data across multiple different systems and services.
The Committee considers that future work to improve data gathering and reporting should culminate in the establishment of a comprehensive dashboard, with the aim of improving transparency, enhancing effectiveness, and reinforcing patient trust.
Introduction
In April 2025, the Health, Social Care and Sport Committee agreed to undertake an inquiry into Attention Deficit and Hyperactivity Disorder (ADHD) and autism pathways and support.
The agreed scope of the inquiry was to consider key issues including:
Why waiting times for assessment, diagnosis and support for ADHD and autism are reportedly long, including the drivers of increasing demand;
How these conditions are currently diagnosed and managed;
The impact of high demand and delays on individuals and healthcare staff;
Exploring solutions to improve the capacity of services, referral pathways and support.
It was agreed that the inquiry would consider the following in relation to neurodevelopmental pathways for ADHD and autism:
referral pathways
assessment, criteria and treatment thresholds
waiting times
"waiting well" and support pre-diagnosis
transitions between services
funding
workforce
the impact on individuals of receiving a diagnosis or waiting for a diagnosis.
In March 2025, the Committee wrote to each of the fourteen NHS territorial boards requesting information on neurodevelopmental pathways and waiting times. All boards responded and SPICe used the data received to produce a briefing on Neurodevelopmental Pathways and Waiting Times in Scotland.
This briefing reported that, as of March 2025, over 42,000 children were waiting for a neurodevelopmental assessment in Scotland (see Figure 1) and that, in some areas, this figure had increased by over 500% since 2020. Over 23,000 adults were found to be waiting for a neurodevelopmental assessment in Scotland (see Figure 2), an increase of over 2200% since 2020 in some areas.
.png)
.png)
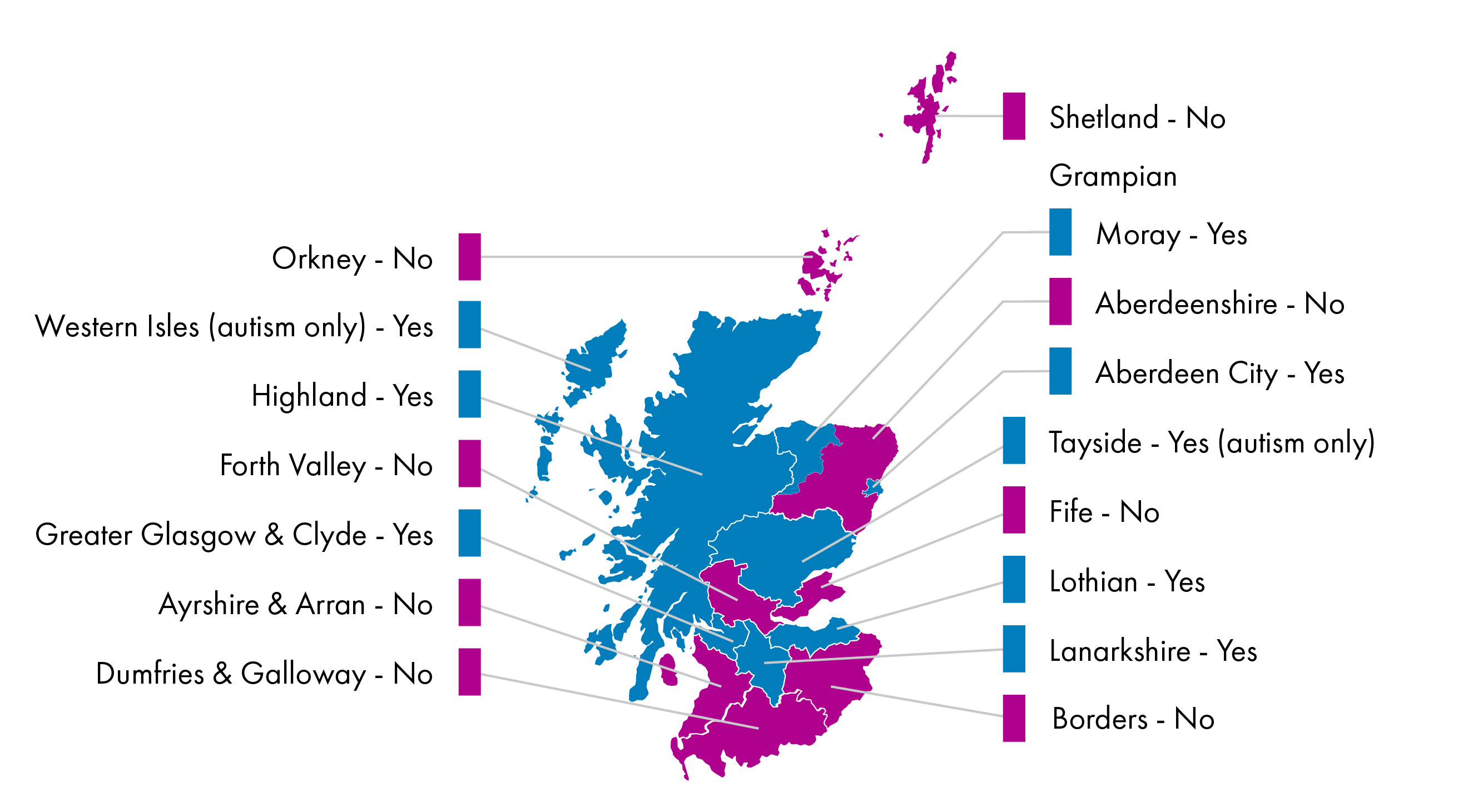
The briefing also reported that pathways for neurodevelopmental assessments vary considerably across Scotland and that, in some areas, no pathway is available through the NHS board for an adult who does not meet the criteria for referral for secondary mental health services (See Figure 3).
At its meeting on 18 June 2025, the Citizen Participation and Public Petitions Committee agreed to refer the following petition to the Health, Social Care and Sport Committee for further consideration as part of the inquiry: Improve access to ADHD diagnosis and treatment across Scotland - Petitions.
In preparation for the inquiry, the Committee wrote to the Minister for Social Care and Mental Wellbeing on 23 June 2025 to request a general update on policy in this area. A response was received from the Minister on 26 August 2025.
As part of the inquiry, the Committee issued a general call for views targeted at organisations on Citizen Space on 23 June 2025.
The call for views asked:
Please tell us your views on the aims of the inquiry, in relation to the people you support, and describe any opportunities for improvement you have identified.
A separate call for views targeted at individuals, families and support workers was issued on the Your Priorities engagement platform on 23 June 2025.
This call for views asked:
Please tell us about your experiences of seeking an Attention Deficit and Hyperactivity Disorder (ADHD) and/or Autism Spectrum Disorder (ASD) diagnosis in Scotland.
Why did you seek a diagnosis?
Is there anything that would have made your experience better?
The call for views on Citizen Space received 86 published responses. SPICe produced a summary analysis of these responses. Your Priorities received 1158 unique submissions and SPICe also produced a summary analysis of these submissions. The Committee is grateful to all those who took the time to respond to the call for views, especially those who shared their lived experiences.
At its meeting on 23 September 2025, prior to commencing taking oral evidence as part of the inquiry, the Committee received a private background briefing from the National Autism Implementation Team (NAIT). NAIT provided a written submission in advance of the private briefing. NAIT also provided the Committee with Neuro-affirming Language Guidance on terminology.
Committee Members held two informal engagement sessions on 25 September 2025 to hear directly from people with ADHD and/or autism. These sessions were supported by the National Autistic Society Scotland and a peer support group for people with ADHD. Anonymised summary notes of the sessions have been published on the Committee webpages. The Committee would like to thank those who volunteered to share their experiences during these sessions.
The Committee also took oral evidence as part of the inquiry over the course of five meetings, from witnesses including:
third sector organisations that support people with ADHD and autistic people
professionals involved in providing support to people with ADHD and autism
NHS Boards
the Minister for Mental Wellbeing and Social Care.
At its meeting on 7 October, the Committee agreed to change the title of the inquiry from "ADHD and ASD pathways and support" to "ADHD and autism pathways and support".
Links to the Minutes and the Official Report of Committee meetings can be found in Annexe A and B.
Background
An increasing number of people in Scotland are seeking neurodevelopmental assessments for conditions such as autism and ADHD. Many specialists in this field argue that this surge in demand is driven mostly by increased awareness of neurodivergence and how it presents, rather than an increase in the number of neurodivergent people. As a result of increased demand, some people have faced long waits to be seen and services have been withdrawn in some areas.
Concerning trends in assessment for autism, Mark McDonald from Scottish Autism told the Committee:
Autism was first diagnosed less than 100 years ago, but that is not to say that autistic people did not exist before then ... We just recognise it now—we understand it, and our understanding has grown. Over the time that our understanding has grown, the thresholds for diagnosis have changed. That has meant that people who historically would not have received a diagnosis are now able to achieve one.
More background information to the inquiry can be found in the SPICe briefing Neurodevelopmental Pathways and Waiting Times in Scotland and in the following SPICe blogs:
The Minister for Social Care and Mental Wellbeing made a statement to Parliament on 26 June 2025 entitled Ensuring the Right Support for Young People’s Neurodivergence, Mental Health and Wellbeing. The statement included an announcement of plans for a cross-sector task force to address the provision of neurodevelopmental services for children and young people in Scotland, supported by £500,000 of additional funding to deliver improvements in these services.
This statement accompanied the publication of a review of the implementation of the National Neurodevelopmental Specification. Among the review’s findings were that:
there was a mixture of views as to whether the Specification met the needs of children, young people and families,
while some praised the increased focus on a neurodevelopmental and multidisciplinary approach, the majority of people surveyed felt that the Specification had had limited impact,
there were major challenges to implementation, including increasing demand, limited funding and poor communication between partners in the Specification’s delivery,
the intended move to a needs-based model had not reduced the demand for diagnostic services, and
there was a lack of clarity over who was responsible for different aspects of implementation, including diagnosis and assessment.
In June 2025, four third sector organisations published a co-produced report entitled Experiences of Autism Assessment and Diagnosis in Scotland.
In October 2025, the Royal College of Psychiatrists in Scotland published a report entitled Multi system solutions for meeting the needs of Autistic and ADHD people in Scotland.
Referral pathways
Accessing pathways to support
As part of the current inquiry, the Committee wrote to each of the fourteen NHS territorial boards requesting information on neurodevelopmental pathways for children and adults. The information received showed variation in the pathways available across Scotland. In several areas, there was no adult neurodevelopmental pathway available. Meanwhile, in some areas, pathways for children were only available to those with a co-occurring mental health condition or who met the criteria for referral to Child and Adolescent Mental Health Services (CAMHS). For a full breakdown of neurodevelopmental pathways in Scotland, see the SPICe briefing Neurodevelopmental Pathways and Waiting Times in Scotland.
During the inquiry, the Committee heard about the importance of early intervention for people with neurodevelopmental conditions. During oral evidence, Anya Kennedy from the Royal College of Occupational Therapists outlined the benefits of early intervention:
By providing support at an early age, when it is needed during their key developmental years, we help children to understand themselves, and how the world around them works, and to manage the various journeys within that ... By helping a child earlier we also support their parents, grandparents and siblings and the local community ... If we are able to support them in the early part of the process, during their childhood, the hope is that they might be able to rely less on services later in their adolescence— for example, within CAMHS or the adult community mental health teams.1
The importance of early intervention was further highlighted by other witnesses. Dani Cosgrove from Stronger Together for Autism and Neurodivergence (STAND) argued :
When support comes at the right time, the benefits extend far beyond the child. It creates stronger families, calmer classrooms and reduced pressure on services, rather than left to escalate ... For us, the right time for support and assessment is as soon as the first concern is raised, whether that is by the child, a family member, a teacher or another professional ... The clearest wider benefit of acting at the right time is simply the prevention of unnecessary harm.2
Dani Cosgrove went on to highlight the confusion that variation in available pathways across Scotland can create for parents and carers:
The variations cause inconsistency, confusion and inequity ... The support in each area is different and that information is unclear. Transparency for children and parents and carers is also lacking ... it is difficult even for us to give correct advice. We could give a family in East Lothian advice and it would be different from the advice that a family in the Highlands would need.2
Variations in available pathways and services between NHS health boards was also identified as a key issue in written submissions to the Committee's call for views.
In its written submission, the Royal College of Paediatrics and Child Health (RCPCH) Scotland identified:
Inconsistencies in neurodevelopmental pathways and staff makeup within services ... [Noting that] these variations contribute to uneven service delivery, exacerbate workforce pressures, and further extend already lengthy waiting lists.4
NHS Grampian Speech and Language Therapy Service noted:
Within NHS Grampian we do not have defined and equitable neurodevelopmental pathways for any age group/client group but as practitioners [we] recognise the need for this.5
The National Autistic Society Scotland called for:
A nationally consistent approach so that families and autistic adults know what to expect and […] an end to the post-code lottery of access.6
Many individuals with lived experience who responded to the Committee's call for views highlighted the personal impact of a lack of available pathways for adults in some areas. For example, one respondent stated:
I am very sure I have ADHD but have no diagnosis. It has a massive impact on my life and I have recently experience yet another burnout and have been unemployed for almost a year as a result (having previously worked in a full time well paid role). I finally approached the GP to find out options for an assessment and was told that unless I am in crisis there is no waiting list that I can join as they have been closed ... I’ve honestly been shocked that there is no support available to even talk about an assessment through the NHS and have no idea what I can do to access support. I want to work, I want to thrive as an individual, a parent, a citizen, an employee but I honestly feel like I get so paralysed and overwhelmed and burnout due to suspected ADHD that I’m not able to ... I feel totally isolated and disillusioned.7
Several witnesses mentioned the work of the National Autism Implementation Team (NAIT), who have carried out pilot projects in four health board areas to develop and implement adult neurodevelopmental pathways. These witnesses argued that the recommendations from these projects should be implemented across Scotland.
For example, Mark McDonald from Scottish Autism told the Committee:
We must take the learning that we got from the neurodevelopmental pathway pilots that were done by NAIT and implement it across Scotland. Best practice is a bad traveller, but there is no reason why we cannot take the learning from those pilots and apply it elsewhere.2
In its Adult Neurodevelopmental Pathways report, the National Autism Implementation Team (NAIT) made ten recommendations resulting from their assessment of the pilot projects, including:
"An adult neurodevelopmental pathway strategy and planning group to be hosted in all HSCPs"
"Development of Adult Neurodevelopmental Pathway standards and guidelines for assessment, diagnosis and support"
"Build a shared expectation that support should be available at any stage for people who identify as neurodivergent"
In his letter to the Committee providing an update on Scottish Government policy in this area, the Minister for Social Care and Mental Wellbeing stated:
Following the publication of the Adult Neurodevelopmental Pathways report, the Scottish Government accepted all ten of the report’s recommendations, and we are taking work forward to implement these.9
The letter added:
Earlier this year, my officials wrote to all health boards seeking clarification on the neurodevelopmental assessment and support they currently have in place for adults. This information is currently being collated and considered, along with next steps.9
In relation to support for children with neurodevelopmental conditions, the Scottish Government published the National Neurodevelopmental Specification for Children and Young People in 2021. As outlined above, a recent review of the implementation of the National Neurodevelopmental Specification set out a number of key findings.
In oral evidence, the Minister for Mental Wellbeing and Social Care told the Committee:
The Scottish Government is committed to improving access to timely, needs-based support for neurodivergent people ... The National Autism Implementation Team published the pathways report a couple of years ago. The Government accepted the recommendations from that and has been working with health boards to support implementation of those recommendations, but I recognise that there is currently variation. Recognising the day-to-day operational role that health boards have, we are committed to continuing to work constructively with boards to achieve the level of national consistency that people across Scotland expect ... For children and young people, our work is guided by the national neurodevelopmental specification, which promotes the provision of early, needs-led support through the getting it right for every child principles. However, rising demand has made implementation challenging. We have invested in pilots, digital tools and family support, and in our work to take forward recommendations to improve implementation, we are being supported by a newly established cross-sector task force.11
The Committee notes with concern the evidence it has heard about the lack of pathways to support for adults, and for children without co-occuring mental health conditions in some health board areas, and the confusion inconsistencies in available pathways across Scotland can cause for individuals and their families.
The Committee welcomes the Scottish Government's commitment to accept the recommendations set out in NAIT's Adult Neurodevelopmental Pathways report, including the development and implementation of guidance for adult pathways in all HSCPs across Scotland, and to review the implementation of the National Neurodevelopmental Specification for Children and Young People through its new task force.
At the same time, the Committee calls on the Scottish Government to take urgent action to develop and implement a national plan to give adults and children with autism and ADHD across all health boards in Scotland access to clear and consistent pathways to support. This should include continuing to work with NAIT and health boards to implement the recommendations from the pathfinder pilots and delivering an updated Specification for children's pathways.
Treatment thresholds and 'gatekeeping'
A number of written submissions to the Committee’s inquiry highlighted treatment thresholds as one key barrier to accessing neurodevelopmental pathways and support. Treatment thresholds are the criteria that are in place in some areas which must be met before an individual can be referred for a neurodevelopmental assessment. Certain written submissions to the inquiry explained that, in response to increased demand, such thresholds have been raised in certain areas in recent years, meaning triaging must take place before referral to a waiting list for assessment can be made.
In its written submission, NHS Ayrshire and Arran outlined the current situation in its local area:
There are no options for assessment and treatment for children, young people and adults in Ayrshire who have a suspected neurodevelopmental profile but do not meet criteria to access a mental health service.1
Commenting on the use of eligibility criteria to determine access to assessment, auticon argued:
By restricting access in this way, many families may be forced to wait until a child’s condition deteriorates or meets the tighter criteria before entering the system. This risks delaying early identification and intervention, increasing unmet need, and ultimately exacerbating pressure on services in the long term.2
The National Autistic Society Scotland raised concerns that the Scottish Government's focus on a needs-led approach could result in thresholds for assessments being raised, concluding:
We would advise that any new approach should be thoroughly tested and evaluated, involving autistic people, and we would strongly caution against making the threshold for assessment too high.3
Representing the Royal College of Psychiatrists in Scotland, Dr Pavan Srireddy argued that early intervention is important at whatever stage an individual seeks help:
I add that early intervention is not only about intervening early in an individuals' life; it is just as applicable to an adult who is in their 30s or 40s. It is as much about recognising a need and putting modifications in place to prevent someone from developing other mental health disorders, or from presenting in crisis to mental health services with far more significant mental disorders that might require greater intervention ... Putting support in place and having access to such support early on still constitutes early intervention while people are waiting for a diagnosis.4
Dr Chris Williams from the Royal College of General Practitioners in Scotland argued "it is neither appropriate nor feasible for all individuals with mild traits to receive specialist assessment and diagnosis".4 He suggested that the Scottish Government should run a public awareness campaign including guidance on when specialist assessments are necessary, support for self-management and signposting to community based third-sector resources. He went on to say that the burden of managing public expectations in the context of long waiting times was falling to GPs and argued that this "risks undermining the doctor-patient relationship".4
Bill Colley from the Scottish ADHD Coalition argued for a more nuanced approach to determining pathways to treatment:
Quality of life ought to be a major consideration, rather than there being the hard criteria of severity and complexity that are set down at the moment. In the criteria, quality of life ought to be a major consideration, rather than there being the hard criteria on severity and complexity that are set down at the moment. The question, particularly with a condition such as ADHD, which is treatable, is whether treatment could improve the person’s quality of life.7
Several respondents to the Committee's call for views described the experience of being told they did not meet the threshold for assessment as distressing. When asked what could have made their experience better, one respondent said: "Not being dismissed as 'not being bad enough' when I was at the point of life being truly unbearable". Another questioned: "Why must Autistic/ADHD people reach crisis before [being] assessed?"8
Many written submissions to the inquiry described the use of treatment thresholds as a form of 'gatekeeping'. They also argued that some people within the workforce who act as 'gatekeepers' lack appropriate training. In particular, many people with lived experience raised concerns that outdated ideas about how autistic people or people with ADHD present remain prevalent amongst GPs, other healthcare professionals, teachers and other educational staff who are involved in referrals for neurodevelopmental assessments.
During oral evidence, Mark McDonald from Scottish Autism described the challenges autistic people and/or people with ADHD can face:
A gatekeeping process, which often results in them coming up against lack of knowledge, a lack of understanding or outdated understanding. For example, a lot of traits that people might look for in an assessment can be based on outdated thinking. We have heard testimony from people who have said that they were told that they were not getting a referral for an assessment because they were able to maintain eye contact. That is extremely outdated thinking, but it exists out there and it results in people having doors closed to them.7
Many contributors to the inquiry pointed out that certain groups of people such as women, girls and people from ethnic minority backgrounds were less likely to be identified as being autistic or having ADHD and argued this may be because they often do not present in the 'stereotypical' way. As Lyndsay Macadam from SWAN Scotland explained during oral evidence: "Autism can present very differently across genders for a number of reasons".7
One individual who responded to the Committee's call for views, described their own negative experience of gatekeeping:
When I approached my GP about ADHD symptoms, having recognised that what I'd attributed to depression was actually ADHD-related difficulties, her response was sympathetic but ultimately dismissive. She refused NHS referral, stating that because I'm a professional with a degree who holds employment, I wouldn't be seen. This discriminatory gatekeeping ignores how adults, particularly women, develop masking strategies whilst struggling significantly.8
A number of older women who responded to the call for views highlighted the particular struggles they had experienced with accessing support. For instance, one individual commented:
I was told that at 56, I should be able to cope by now—and was even asked if I was just seeking medication. That left me feeling like I was wasting her time ... ADHD doesn’t go away just because we’ve reached a certain age. Everyone deserves to be listened to and supported—especially when they finally find the courage to ask for help.8
During oral evidence, Sofia Farzana, representing Scottish Ethnic Minority Autistics (SEMA), described the particular experiences some ethnic minority women can have when seeking support:
Masking is extremely high if you are black or brown and female, because of the way that, in our communities, the gender roles are so defined. A lot of the autistic women that I speak to say that they have been told since childhood that they are too masculine to be girls ... When we ask for support, the difference in our culture as autistic people is put down to racial culture ... Given how I am dressed, no one can assume when I last brushed my hair. I have it tied up, so who knows? The way I dress is all masked up [Sofia wears a hijab] and that is my culture and I have been brought up in a way to mask everything anyway. It is a complete lack of understanding when a clinician says, “She does not have high support needs” and does not even acknowledge that support needs can fluctuate. They presume things and they do not understand ... We have got to this point for survival’s sake because, as racialised autistics or as racialised people, we have just been told to get on with it.7
In their written submission, SEMA described negative experiences of interacting with health professionals, particularly GPs:
GP’s are gatekeepers. GP’s need more equality, diversity and inclusion training. They need to have more cultural competent training. This training needs to be from professionals with lived experience. For young people, teachers’ lack of understanding can be barrier to assessment referrals and delays diagnosis to even go beyond child to adult transitions. Improvement in teacher training from lived experienced professionals is needed ... experiences with GP’s and psychiatrists have been negative with dismissive remarks, and not progressing referrals. Lack of overall understanding of autism and ADHD in women in is poor […] Lack of believing patients has been a problem for many people.14
Some who responded to the Committee's call for views raised concerns that, due to a lack of suitable training for teachers and other educational professionals, the requirement for a child to be referred by their school to be able to access a neurodevelopmental assessment could be an issue:
Schools have been placed in a position where they are the gatekeepers to assessment. We approached our GP at one point and were advised referral to CAMHS from them would most likely be declined and that indicators from school are essential to acceptance. However, I am unsure if teachers have access to sufficient training to recognise more subtle features of autism. I also think there is a lack of understanding of Autistic Masking. I fear that schools are over-stretched and that there may be a bias against assessment as this places an onus on schools to meet those additional needs.8
Many witnesses also recommended that further training for the workforce involved in providing assessments should be implemented consistently across the country. Recommendations included that the training should be developed in close collaboration with autistic people and people with ADHD and should be mandatory.
Gill Kidd from Child Heads of Psychology Services suggested that an overall competency framework should be developed with different levels of training prescribed depending on the skills needed for particular roles. She argued that this should include training suitable for all roles, from receptionists to GPs to teachers, "right through to what you need if you are diagnosing and doing specialist assessment".4 She suggested that the National Trauma Training Programme, which was developed by NHS Education for Scotland (NES) could be drawn on as an example framework for this purpose.
During an oral evidence session, the Minister for Social Care and Mental Wellbeing highlighted existing training such as the NES Foundations of Neurodiversity Affirming Practice webinar that he argued should be routinely utilised by professionals working with neurodivergent people.
At a separate point, the Minister highlighted the importance of ensuring that gate keeping does not become a barrier to access to support:
Education and local authorities should not be using the need for a diagnosis as a way to gate keep access to services.17
The Committee recognises that the scale of demand for neurodevelopmental assessments has made it necessary to put certain thresholds in place before a referral is made and that this has resulted in gatekeeping access to assessments in some areas.
However, the Committee has been concerned to hear evidence that many people feel those responsible for referrals and gatekeeping do not have an accurate, up to date understanding of neurodevelopmental conditions and how they present, particularly in women, girls and ethnic minority people, meaning that thresholds may not be applied fairly or appropriately in some cases.
The Committee is further concerned that an over-reliance on threshold setting and gatekeeping risks resulting in many individuals being unable to access the support they need at the appropriate time, leading to a situation where these individuals will then present themselves at a later stage having reached a state of crisis, which can be considerably more difficult and costly to treat. The Committee concludes that, although perhaps understandable when trying to deal with consistently high demand, such an approach to managing access to pathways risks being counterproductive in the longer term.
The Committee therefore calls on the Scottish Government, in responding to this report, to set out how it intends to address this challenge and to ensure Health Boards shift their focus to a progressive approach which ensures the provision of treatment and support for autistic people and/or people with ADHD at the earliest opportunity, in line with the principles of its Population Health Framework.
The Committee further recommends that the Scottish Government takes action to ensure improved consistency and timeliness across Scotland of access to treatment and support, including an assessment or diagnosis where appropriate.
To further improve quality and consistency, the Committee calls on the Scottish Government to develop a plan to deliver mandatory training to all those who are involved in making referrals to neurodevelopmental pathways. This training should:
be developed in collaboration with people with neurodevelopmental conditions
draw from existing resources already developed by NES, NAIT and in health board areas where appropriate
be monitored and reported on to determine rates of uptake.
More broadly, the Committee recommends a programme of mandatory training on neurodevelopmental conditions for all health and social care staff in patient-facing roles.
Open referral
Self-referral, open referral or 'requests for assistance' were all suggested in written and oral evidence as alternative ways for people to access specialist support or assessment without the need to obtain a formal referral from their GP or school. In reference to these alternative pathways, Mark McDonald from Scottish Austism told the Committee: "It is helpful to have a pathway that people can refer themselves into without having to go through a gatekeeping process".
In their written submission to the Committee, NAIT highlighted the benefits of open referrals, when provided for in accordance with best practice:
Open referrals or requests for assistance allow families or individuals to self-refer, or schools as well as health professionals to make the request for neurodevelopmental assessment. Where this works well, there is clear guidance and information for those making requests about the information needed to proceed. NHS Dumfries and Galloway is a good example of this practice. Local areas have been concerned that having an open-referral process will ‘open the floodgates’ but the evidence from Dumfries and Galloway and in Grampian adult autism team is that this does not happen. The demand or need is similar to other areas, but the outcome is better conversations earlier, with the right people and a better ‘patient flow’.1
Louise Bussell from NHS Highland cautioned against setting an expectation that self-referral would necessarily enable patients to access support or treatment more quickly, pointing out that resources to deliver such support and treatment would remain finite. Dr Cath Malone from NHS Tayside told the Committee she was concerned that, if an open referral process were adopted in her health board area, the resulting volume of open referrals would be unmanageable. She suggested that improved data and evidence was needed to be able to assess the extent to which open referrals should be encouraged by health boards across Scotland. She went on to argue that, in the absence of an open referral model, "appropriate triage means that the right people are getting assessments in a timelier way".2
Dr Gill Kidd from Child Heads of Psychology Services argued that triage could still take place as part of an open referral approach:
Open referral is a request for assistance for support and understanding of the strategies. In some areas, that is a new way of working that we can build on, spread and expand. To go back to the point about stepped and matched care, that is needed at the point where parents and education are requesting that support. Easy access to that would reduce the need for referrals for a diagnosis when that is not the requirement, but we also need a way of stepping up requests where a diagnosis and a formal assessment are required. NHS Fife is working that kind of model, where there is open access for support but there is also the mechanism to refer in when further assessment is required.2
The Royal College of Speech and Language Therapists were supportive of an open referral model in their written submission:
'Request for assistance’ models, which replace traditional referrals with an open referral system with timely triage, have long been implemented by SLT services across Scotland and are showing great results when used in neurodevelopmental services. Neurodevelopmental assessment pathways in Fife and Dumfries & Galloway, which both have strong SLT representation in the pathway leadership teams, are excellent examples of good multi-disciplinary collaboration and working relationships. They have challenged professional assumptions that an open referral system will open the flood gates to inappropriate referrals, when in fact it means effective conversations happen earlier and individuals get the support they need sooner, including while waiting for an official diagnosis.4
The Committee notes concerns from many healthcare practitioners that broader application of an open referrals model for accessing ADHD and autism pathways would create a risk of "opening the floodgates" to even greater demand and a rise in inappropriate referrals that would be liable to overwhelm services.
At the same time, the Committee notes a strong desire from many individuals to have the option of open referral available to them. It further notes evidence from certain areas where an open referral model is already in place which suggests concerns about services being overwhelmed are not borne out by experience on the ground. Instead, there is strong evidence to suggest an open referral model can help pathways and services to operate more efficiently and responsively.
The Committee therefore calls on the Scottish Government, in responding to this report, to set out what further action it is taking or plans to take to gather further data about the practical impact and any specific benefits for pathways and services of allowing open referrals, to learn appropriate lessons from experience of open referrals on the ground and to explore how open referrals can be made more widely available across Scotland in a way that allays workforce fears that this will result in services being overwhelmed.
Beyond this, the Committee would encourage the Scottish Government to explore how, in future, processes for open referral can be better integrated into national standards for ADHD and autism pathways and support.
Waiting
Waiting lists
In March 2025, the Committee wrote to each of the fourteen NHS territorial boards requesting information on neurodevelopmental pathways and waiting times and received a response from every board. National waiting list data for neurodevelopmental assessments are not routinely published in Scotland. It should be noted that the data provided below only includes those waiting for assessment, not those who may have requested support but did not meet the criteria for referral for an assessment.
As of 31 March 2025, all health boards (with the exception of NHS Tayside, who were not accepting new referrals) had established neurodevelopmental pathways for children who didn't meet the criteria for referral to CAMHS. Thirteen of the fourteen health boards reported the number of patients waiting for this service (except for NHS Grampian, who could not provide this figure as they did not have the ability to separate out the requested data on their patient management system). In general, the data received from NHS boards was not in a uniform or easily comparable format (please see para 216 for the Committee's recommendation in relation to this). The data show that there were 42,530 children waiting for a neurodevelopmental assessment as of that date (see Figure 1).
Eight health boards (Ayrshire and Arran, Fife, Lothian, Tayside, Borders, Forth Valley, Greater Glasgow and Clyde and Highland) were able to provide data on the length of waiting lists in previous years, although only the first four provided data going as far back as 2020. The number of children waiting for a neurodevelopmental assessment in Ayrshire and Arran, Fife, Lothian and Tayside increased from 2,475 to 14,943 between 2020 and 2025 - an increase of over 500%.
Six health boards reported having a neurodevelopmental pathway that is available to adults who do not meet the criteria for referral to secondary mental health services (Greater Glasgow and Clyde, Lanarkshire, Lothian, Tayside, Highland and Western Isles). However, it should be noted that, in the case of Tayside and Western Isles, this pathway was only available for support with or assessment for autism. Provision across the three Health and Social Care Partnerships (HSCPs) covered by NHS Grampian was variable since Aberdeenshire HSCP ceased its adult neurodevelopmental pathway in February 2025.
Nine health boards disclosed the number of adults waiting for a neurodevelopmental assessment in their areas. This included five of the health boards with adult neurodevelopmental pathways in place (Greater Glasgow and Clyde, Highland, Lothian, Tayside and Western Isles but not Lanarkshire) and four of the boards which offered neurodevelopmental assessments only to those who met the criteria for referral to secondary mental health services (Ayrshire and Arran, Fife, Orkney and Shetland).
There were 23,339 adults reported as waiting for a neurodevelopmental assessment as of March 2025 (See Figure 2), and over 97% of these were in areas where adults did not have to meet the criteria for referral to secondary mental health services to access these services. The number of adults waiting for a neurodevelopmental assessment across Forth Valley, Highland, Lothian and the Western Isles increased by more than 2200% in five years, from 543 in 2020 to 12,974 in 2025.
All health boards reported the median and longest current waiting times for children seeking a neurodevelopmental assessment, except for NHS Grampian (which could not provide data specific to neurodevelopmental cases) and NHS Dumfries and Galloway (which provided a longest waiting time only). Median waiting times ranged from 22 weeks (NHS Western Isles) to 141 weeks (NHS Ayrshire and Arran), with an average median waiting time for children across all health boards providing data of 76 weeks. Longest waiting times ranged between 69 weeks (NHS Fife) and 342 weeks (NHS Ayrshire and Arran), with an average longest waiting time for children across all health boards providing data of 196 weeks.
Nine health boards (Lothian, Ayrshire and Arran, Tayside, Forth Valley, Highland, Fife, Shetland, Orkney and Western Isles) reported both the median and longest waiting time for an adult seeking a neurodevelopmental assessment, while Greater Glasgow and Clyde reported the longest waiting time only. Forth Valley, Tayside and Fife reported waiting times for autism assessment only. Ayrshire and Arran and Western Isles reported the combined average from the median waiting times for autism and ADHD individually. Median waiting times ranged from 24 weeks (NHS Orkney) to 146 weeks (NHS Tayside), with an average median waiting time for adults across all health boards providing data of 76 weeks. Longest waiting times for adults ranged between 61 weeks (NHS Fife) and 390 weeks (NHS Greater Glasgow and Clyde), with an average longest waiting time for adults across all health boards providing data of 182 weeks.
Speaking to the Committee during an oral evidence session, Dr Pavan Srireddy from the Royal College of Psychiatrists in Scotland highlighted the significant rise in demand for services:
We must recognise the sheer scale of what we are discussing. The increases in referral rates, in demand and in the numbers of young people and adults awaiting diagnosis are beyond anything that we have seen in the recent history of our healthcare systems apart from during the Covid pandemic ... The reality on the ground is that our healthcare model is designed to meet the needs of 1 per cent of the population, but it is trying to meet the needs of more than 20 per cent of the population. That cannot and will not work.1
Impact of waiting times
Oral and written evidence submitted to the inquiry suggests that long waiting periods can be distressing and harmful for individuals and their families. In its written submission, Children's Health Scotland argued that “children's wellbeing deteriorates during long waits for diagnosis, with increased anxiety, school refusal, and social withdrawal”.1
Other responses to the Committee's call for views supported this view, with one respondent describing their daughter's negative experience of waiting for an assessment and support:
My daughter was referred for neurodevelopmental assessment in Primary 5 by her new head teacher ... That was four and a half years ago. She’s now 13 and has just entered S3 in high school, still without a diagnosis or the support she needs. In that time, she has withdrawn socially, been bullied for thinking differently, and repeatedly placed in isolation because staff don’t know how to manage her needs. She was 9 when referred; now she’s navigating adolescence and hormonal changes without the understanding or tailored help she deserves. This delay has had a profound impact on her mental health, education, and self-esteem. We have been left to cope alone, misunderstood and unsupported, while her potential remains untapped. I am deeply concerned about the long-term consequences of this delay and the emotional toll it continues to take.2
Another respondent described their experience of lengthy waiting times as an adult:
I’ve been waiting 3 years. When I first went on the register for assessment I was told about 18 months, then it’s just kept being pushed back. I phone about every 6 months and record the date I phone and the new time they expect me to be seen. It’s ridiculous ... I feel stuck in this limbo and it is very frustrating.2
During an oral evidence session, Dani Cosgrove from STAND described similar experiences of families her organisation supports:
We hear from our families that the longer they wait for the assessment, the longer it is before their child’s needs are fully met and properly understood. Children are losing years of development, families are being left in limbo and support is being delayed or withheld. A parent spoke to me last week and described the waiting period as "physically and emotionally torturous".4
In further correspondence to the Committee, STAND highlighted that children face exclusion from activities while waiting for support:
During this time, many children are excluded from school activities, parents reduce or leave work and mental health deteriorates. The waiting period is not neutral; it is actively damaging.5
Several respondents to the call for views described experiences of children "ageing out" of the children's waiting list before being seen and then having to join the bottom of an adult waiting list. The transition from childhood to adulthood was recognised as a crucial point in a young person's life where a lack of appropriate support could leave them especially vulnerable.
Many contributors to the inquiry suggested that individuals and families waiting for an assessment or further support were not given necessary information and that communication was generally poor.
One respondent to the call for views commented:
Not knowing roughly how long each stage would take was one of the most difficult and frustrating parts of the process. There was a lot of waiting with very little communication.2
Another argued:
If the wait times cannot be changed more open and honest communication would at least [allow] parents to know where they stand in this regard.2
In its written submission, the Autistic Rights Group Highland (ARGH) reported similarly negative experiences from people on waiting lists for assessment:
They are given no support and receive no or very poor communication whilst waiting for an assessment, they feel abandoned and that they are expected to 'just get on with life' but cannot just get on and often feel that their life is falling apart. Once someone finally receives an assessment, even if they are diagnosed the wait is not over: people can wait months for a further appointment to receive medication (ADHD) or just be given a leaflet and told to get on with it (often the materials handed out are out of date and / or far from neuroaffirming).8
One individual with lived experience who participated in an informal engagement session as part of the Committee’s inquiry said that "what helped them during this period was not access to medication but rather rest and exercise – and it would have been beneficial to have received more advice about that".9
Several respondents with lived experience of being on a waiting list for assessment explained that one of the only pieces of communication they received during this time was a letter asking them to confirm if they still wanted to be on the waiting list and telling them they would be removed from the waiting list if they did not respond within a certain time frame. During an informal engagement session as part of the inquiry, one participant described how difficult it can be for people with ADHD, who struggle with executive function, to deal with such a process. On receiving one such letter, this participant described putting it away and forgetting about it and explained this would be typical behaviour for someone with ADHD.
Witnesses reported pockets of good practice such as "waiting well" initiatives but went on to argue that there are no consistent standards across the country. Thelma Bowers from NHS Ayrshire and Arran informed the Committee that her health board has established a Neurodevelopmental Empowerment & Strategy Team (NEST) which has developed a central hub for online resources and information, and also runs workshops. She went on to describe having "worked with the third and independent sector to create alternative supports and options such as physical activities and programmes of therapy while young people are waiting".10
Anya Kennedy from the Royal College of Occupational Therapists told the Committee she was aware of several projects across the country to develop resources for people with neurodevelopmental conditions, including some that have been developed by NAIT. She suggested:
We need to try to work smarter with the resources that we have. A once for Scotland approach allows us to pool resources and skills from across Scotland, and not just work within individual board areas.10
Dr Pavan Srireddy from the Royal College of Psychiatry argued that "curated, good-quality information gives people the ability to access help and support based on what their needs are at that time".10 He suggested there is currently an over-reliance on social media as a source of information and that this can sometimes be inaccurate or harmful.
Some witnesses also mentioned that lengthy waiting lists have had a negative impact on staff wellbeing and morale. Thelma Bowers from NHS Ayrshire and Arran told the Committee:
There are still waits, which create burnout in our team and a sense of moral injury from not being able to support people in the way that clinicians would want to. Because people either cannot get a diagnosis or they have a long wait—which could be two and a half years—we receive a lot of complaints and inquiries, which our team have to deal with at the same time".10
Similarly, Louise Bussell from NHS Highland said:
It is also important to note the number of complaints that come in from families. It is often the people at the front door—the folk on reception and in admin roles—who absolutely bear the impact of people contacting them, asking “What is happening?” and, understandably, being very unhappy.10
In oral evidence to the Committee, the Minister for Social Care and Mental Wellbeing said:
My clear expectation is that anyone who is waiting for assessment should be sensitively signposted to support that is available.15
Reasons for long waiting times
The Committee heard both oral and written evidence that waiting times for ADHD and autism assessments have increased at an unprecedented rate in recent years due to increased awareness and understanding of neurodevelopmental conditions. Several witnesses told the committee that this is partly due to 'historical underdiagnosis' particularly amongst older generations and women.
Several witnesses mentioned that they were aware of a narrative developing that ADHD and autism is being over-diagnosed and were keen to dispel this idea. In this context, Rob Holland from National Autistic Society Scotland expressed the following concern:
Sometimes the debate in this space is focused on reducing referrals rather than making sure that we tackle the issue here. The issue is not a problem of demand; it is a problem of supply and ensuring that we have the right number of assessments and the right level of support.1
Bill Colley from the Scottish ADHD Coalition argued that statistical data points to an under-diagnosis of ADHD in the population. He pointed to research suggesting prevalence of ADHD in children is estimated to be between 5-7%, meaning that between 73-81% of children who have ADHD are not diagnosed. Furthermore, he said that estimates suggest 2-4% of the adult population have ADHD, meaning that 91-96% of this population are not diagnosed. He concluded: "Given that ADHD is a treatable condition, the vast majority of people who have it have not been assessed and diagnosed and are, therefore, not receiving treatment".1
Written evidence submitted to the Committee suggests that healthcare systems are not prepared for the considerable increase in demand for support and assessments currently being experienced. Contributors to the inquiry argued that a lack of funding and an appropriately skilled workforce are two of the main reasons why waiting times are so lengthy.
Louise Bussell from NHS Highland encapsulated this view:
Workforce challenges have a massive impact on our waiting times; they are the most significant factor in why we have the waiting times that we do. There are multi-faceted reasons for that. They are not all about being able to get people for the roles; they also include having the finance in place ... there is a small market for such positions, because only a small number of people can currently do that work. We need to build a much greater workforce, but first we need the finance to enable us to do so.3
Representing Child Heads of Psychology Services, Dr Gill Kidd agreed that there are gaps in the workforce and went on to describe the impact this is having on CAMHS services:
There are workforce bottlenecks, in particular around prescribing. There are insufficient medical and non-medical prescribers to meet the demand. Even if we diagnose ADHD, for example, there will still be a wait for prescribing and treatment. The diagnostic process generally sits with a small number of people so we have bottlenecks there, too. As I said, some of those services sit within CAMHS. Although the workforce and the skills might be there, some services have not been able to direct capacity to neurodevelopmental services because of the need to also address the waits for mental health services, so we are confounding two workforces.3
Witnesses also highlighted short term availability of funding as a particular issue when trying to plan longer term improvements to services. They also reported particular challenges with recruiting qualified staff because temporary posts are generally less attractive than more secure long term or permanent posts. While short term funding for pilots was welcomed, many felt that longer term funding commitments were needed to be able to embed improvements. Dr Gill Kidd advocated a multi-agency approach where the allocation of funding was integrated across "education, social work, children's services and CAMHS" as well as healthcare.3
Giving oral evidence to the Committee, the Minister for Social Care and Mental Wellbeing emphasised the Scottish Government’s commitment to addressing the issue of long waiting lists through a multi-agency approach:
Neurodevelopmental needs span health, education and social care, and they are shaped by a wide range of factors. A traditional national health service waiting list approach is not sufficient. What is needed is a coordinated multi-agency response that focuses on timely, needs-based support and reflects the evolving nature of neurodevelopmental needs and the diversity of individual experiences. The Scottish Government is committed to improving access to timely, needs-based support for neurodivergent people.6
The Committee has been extremely concerned to hear evidence during this inquiry of many individuals having to wait many years on a waiting list for assessment for ADHD, autism and other neurodevelopmental conditions, as well as evidence from many areas where waiting lists have now been closed. It is firmly of the view that, as well as being detrimental to the individuals affected, such a situation is damaging to wider society to which, for as long as they fail to receive the support and treatment they need, these individuals may be prevented from making an active and positive contribution.
The Committee acknowledges evidence of an unprecedented rise in demand for neurodevelopmental assessments in recent years. It has been persuaded by evidence that this rise is not attributable to a tendency towards over-diagnosis but rather to an historic under-diagnosis of ADHD and autism and an improved understanding of these conditions more recently. The Committee is also sympathetic to the suggestion that promoting a narrative around over-diagnosis is unhelpful and risks further stigmatising those with autism and/or ADHD, with the result that their condition is not believed or understood and they are denied access to the pathways and support they need.
Given the current length of waiting times, the Committee believes it is particularly crucial that the quality of communication with those on waiting lists is consistently high, that available information is accurate, supportive and up-to-date, uses neuro-affirming language and is delivered in a way that is responsive to the specific needs of those with autism and/or ADHD.
For the same reason, the Committee calls on the Scottish Government to give much greater attention, including the commitment of appropriate resources, to the development of "waiting well" initiatives that provide suitably targeted access to good information and local support as a consistent and integral part of the waiting process for those on neurodevelopmental pathways.
The Committee welcomes the Scottish Government's establishment of a task force and its commitment of additional funding to support implementation of the National Neurodevelopmental Specification. As part of this work, the Committee calls on the Scottish Government to produce a roadmap setting out clear timelines for improvement of ADHD and autism pathways and support. This should address improvements to information and communication (including the potential establishment of a 'one stop shop'), improved access to local support while waiting, the roll-out of targeted "waiting well" initiatives and the commitment of funding to develop the multi-disciplinary workforce needed to reduce waiting times in the longer term.
Assessment and diagnosis
Assessment process
As set out in the SPICe briefing Neurodevelopmental Pathways and Waiting Times in Scotland, the assessment process for ADHD and autism varies between different NHS Scotland territorial health boards. However, in general, it tends to require several appointments, depending on the complexity of the case. These appointments have two key purposes. The first is information gathering through interview-style discussions with the patient and their family. The second is direct observation of the patient and their behaviours, sometimes across a range of environments. For example, where a child presents differently at school as opposed to at home, it can be appropriate to arrange in-school and at-home observations. Specialist multi-disciplinary assessment teams carry out these observations and discussions.
Once the multi-disciplinary team has gathered the relevant information, the assessment team will reach a judgement as to the diagnosis of the patient. This is done against a standard set of criteria, such as the DSM-5 or ICD-11. Patients may be diagnosed with one or more neurodevelopmental conditions, or none at all. The team making the assessment may also diagnose co-occurring mental health conditions. Finally, the team shares the diagnosis with the patient, their family and other groups (such as the school, GP, or social care services). The patient may be signposted to further post-diagnostic support, either within the NHS or via the third sector.
Areas for improvement to the assessment process were identified by some respondents in written evidence submitted to the Committee. For instance, Heriot-Watt University argued there was a:
Need to consider an assessment process and tools which better support identification of autism and ADHD which are more accessible and neuroaffirmative (ensuring that neurodivergence is not seen as an abnormality but rather as a normal variation of human experience). We need to consider the impact of diagnosis on the individual and ensure that the process, rather than highlighting deficits with no route to support, offers insights and potential routes to support.” They went on to say that the “current diagnostic criteria are outdated, deficit-based, and fail to capture the diversity of autistic experience, especially when autism co-occurs with ADHD or other conditions. Older adults, women, and people from marginalised ethnic and LGBTQ+ communities are less likely to receive timely or accurate diagnoses.1
In their written submission to the inquiry, SWAN Scotland also called for diagnostic tools to be reviewed and updated, arguing:
Standard diagnostic criteria were originally designed to identify traits prevalent in males and are therefore not fit for purpose for assessing women and other genders. The process itself is deficit-based and can be disempowering and humiliating for individuals.2
Several people with lived experience of the assessment process reported finding it difficult to navigate, particularly for those with ADHD who may struggle with executive function. One respondent commented: "The process of filling in all the required forms for assessment was extremely challenging, and the irony of a person with ADHD trying to navigate this was not lost on me".3
Several witnesses giving oral evidence suggested that recruiting diagnosticians from more varied backgrounds could help to improve the experience of assessment for patients. For example, it was suggested that this could include minority ethnic people or people who are themselves neurodivergent. Witnesses also suggested that, to improve their understanding, diagnosticians should be encouraged to engage more with neurodivergent people through community groups.
For instance, Kabie Brook from Autistic Rights Group Highland argued:
It would help if diagnosticians kept up with research and learned about what it is like to be autistic, from all kinds of community groups, so that they have a relationship with and an understanding of autism from the inside ... a lot of them meet autistic people only in the clinic, which is a scary place.4
The Committee heard evidence during the inquiry that co-occurrence of different neurodevelopmental conditions in a single individual is very common. NAIT's written evidence indicated: "There is 40% co-occurrence across autism and ADHD diagnoses" and concluded that "separate pathways are inefficient and ineffective".5
Many people with lived experience of the assessment process who responded to the Committee's call for views reported having been assessed for one neurodevelopmental condition only to go back to the bottom of the waiting list to access an assessment for another condition. For example, one individual explained: "It took 7 years of being on the waiting list for the autism one and I’ve been told it will be at least another 10 for the ADHD one".3
In this context, there was consensus amongst witnesses that offering single condition assessments was not a good approach. Anya Kennedy from the Royal College of Occupational Therapists told the Committee:
The evidence supports integrated neurodevelopmental assessments, rather than the siloed pathways that we currently have ... Somebody may be on the list for an autism assessment and also on the list for an ADHD assessment ... That is inefficient and causes delays for the individuals, their families and their carers. It is also inefficient in the use of resources and skills.7
In its paper ‘Multi system solutions for meeting the needs of Autistic and ADHD people in Scotland’ the Royal College of Psychiatry Scotland called for:
National standards for NDC [neurodevelopmental condition] assessments, overseen by an appropriate Government inspectorate. Comprehensive, holistic mental health assessments should be the new standard. Single-condition assessments should not be offered.
Several witnesses advocated the development of a national standard for neurodevelopmental assessments across Scotland. For instance, Dr Pavan Srireddy from the Royal College of Psychiatrists Scotland argued:
There is also a lack of consistency in what constitutes a good-quality neurodevelopmental assessment. We have such standards individually within board areas, but there is nothing nationally that determines what a minimum good-quality assessment would look like. We would strongly recommend and advocate for a national standard, which could serve as the gold standard of what you would expect.7
A number of witnesses expressed a view that NICE and SIGN guidelines should be reviewed and updated. In particular, there was a call for clearer guidance to identify those qualified to complete assessments.
In its written submission to the Committee, NAIT recommended the use of wider, multi-disciplinary teams to undertake assessments and diagnosis. They argued that this could involve a "stepped care" approach (a model whereby the most effective yet least resource-intensive treatment is offered to patients in the first instance) and could help to reduce waiting times, concluding:
CMHTs and Psychiatric services cannot and will not be the solution to meeting all of the needs for diagnostic assessment of neurodivergent people. Instead, a stepped care approach is required, with new multi-disciplinary specialist teams undertaking diagnosis and offering support and the right conversations at an earlier stage, before crisis hits. These teams should link with CMHTS and use the expertise of psychiatry and psychology services, to ensure smooth links between steps in the pathway.5
During oral evidence, Scottish Government Official Dr Lynne Taylor argued in favour of a needs-led assessment that takes into account potential co-occurring conditions such as anxiety and Avoidant/Restrictive Food Intake Disorder (ARFID):
The complexity of how an individual presents is often affected by their environment, their physical symptoms and their past experiences … About ARFID, which involves restrictive eating and hyperfocus. Neurodevelopmental conditions can cause people to develop problems with eating and other things such as anxiety … I have quite often in my clinical practice had individuals referred for obsessive compulsive disorder because they have presented in that way, but, through further needs-led assessment and individual formulations that describe individual stories of strengths and weaknesses … we can gather a picture of the whole person and the whole individual.10
In connection with this point, the NHS UK website provides further information about other neurodevelopmental conditions and other mental and physical health problems that can affect people with autism.
In oral evidence, many witnesses also recommended greater use of multi-disciplinary teams in assessment processes. For example, Rob Holland from the National Autistic Society Scotland spoke of "the need to expand the multidisciplinary team that can be involved in the assessment process".4 Some witnesses reported evidence of multi-disciplinary teams already being used in some health board areas but concluded that longer-term funding and a more consistent national approach was needed to guarantee standards across Scotland.
Representing the Royal College of Occupational Therapists, Anya Kennedy argued:
It should not be a uniprofession approach, involving only a doctor or a lone AHP doing that assessment, because the assessment is multidimensional and looks at different areas.7
Correspondence from NHS Lanarkshire’s Neurodevelopmental Service School Team included information about a whole school approach to neurodevelopmental assessments within mainstream primary schools that is being undertaken in that health board area:
NHS Lanarkshire’s Neurodevelopmental Service carried out 2 Tests of Change (ToC) to consider assessment in a different way. The first test was within South Lanarkshire and the second within North Lanarkshire. The focus of the ToC was to consider a Whole School Approach to ND Assessments within mainstream primary schools. We wanted to consider service efficiencies when all children on the current waiting list in a school were assessed at the one time, in their own environment and with the full support of the school. In conjunction with the assessments, we also wanted to provide a range of Parent Workshops to the parents involved in the ToC, but also to the wider school community.13
NHS Lanarskshire reported having found that this whole school approach offered a number of benefits including:
Maintaining diagnostic quality and multidisciplinary input comparable to traditional clinics
Improving access and equity for children and families who may struggle to engage with clinic-based services
Supporting earlier identification and intervention for autistic children and those with ADHD, intellectual disability, and other ND profiles
Supporting schools with the development of strategies for those with an ND profile within their school prior to any formal diagnosis
Engaging with families in a less intimidating / more familiar setting
Improving family satisfaction and diagnostic throughput
Increasing capacity
Some witnesses recommended consensus diagnosis as an alternative approach for less complicated cases. This is a process whereby a team of professionals along with the individual and their families can come to a mutually agreed position that there is sufficient evidence for a diagnosis to be arrived at and for appropriate support to be put in place.
Dr Gill Kidd from Child Heads of Psychology Services explained:
Currently we have long waiting lists that are difficult to stratify to look at individual cases. Therefore, work needs to be done first to identify who is on a waiting list and what their needs are, and then to point them in the right direction towards either a consensus diagnosis or a more formal structured assessment where that is required.7
The Committee calls on the Scottish Government, in close collaboration with health boards, to undertake a comprehensive review of the assessment process in all areas with a view to developing a National Standard for assessments that guarantees consistency of access, responsiveness and support throughout Scotland. In particular, this review and the resulting National Standard should address:
ensuring diagnostic criteria used in assessments are appropriate and up-to-date;
a presumption against the use of single condition assessments, given the high rate of co-occurrence of ADHD and autism (as well as other neurodevelopmental conditions and other mental and physical health problems) and the active promotion instead of the use of holistic assessments;
the development of guidelines to establish clear qualification requirements for those carrying out neurodevelopmental assessments;
Promoting the direct involvement of individuals with lived experience of neurodevelopmental conditions in helping and supporting others to navigate the assessment process;
clear guidance for the use of alternative approaches to assessment such as "whole school" approaches, "stepped care" and "consensus diagnosis" - to include details of the circumstances in which such alternative approaches may be more appropriate than traditional approaches to assessment;
promotion of a multi-disciplinary approach to assessment, including requirements for members of multi-disciplinary teams to undergo continuous professional development and training on providing neurodevelopmental assessments, to include regular updates in neuro-affirming practice.
To ensure the review and resulting National Standard are as responsive as possible to the needs of those seeking an assessment, the Committee calls on the Scottish Government to ensure individuals with lived experience of neurodevelopmental conditions and the community groups that support them, are actively involved in the review process.
The Committee also believes there should be a requirement on health boards to work with the National Autism Implementation Team to ensure updated service specifications for provision of services are successfully implemented, both for children and young people and for adults.
Impact of receiving a diagnosis
The Committee heard from many people with lived experience who highlighted how important receiving a diagnosis had been for them:
Receiving my diagnosis of ADHD has been life-changing for me, predominantly in terms of the way I view myself. Having a diagnosis is extremely validating, and knowing that there is a reason for my struggles has allowed me to be much kinder to myself. I was diagnosed about a year ago, age 44. I am slowly processing and trying to undo a lifetime of negativity towards myself, and understanding the impact that this undiagnosed condition has had on my life.1
In oral evidence, Kabie Brook from Autistic Rights Group Highland, emphasised the impact receiving a diagnosis can have:
The impact is massive. It is about knowing who we are and being able to understand ourselves and understand what is going on for us as a way to get our needs met. Everyone has the right to know who they are ... Before identification, it can feel as if we do not fit in, we are wrong and everything that we try is doomed to failure ... It is like a slow indoctrination in the view that you must be wrong: if everyone else does not feel that way, it has to be a problem with you—it has to be something wrong with you. That can lead to very poor mental health and suicidal ideation and sometimes to people going through with that. In a way, it is like it is for any minority group. It feels as though we are constantly being pointed out by the whole of society and then people say, “It is your fault”. It is not our fault.2
Many people who contributed to the inquiry mentioned that being able to access medication for ADHD as a resut of a diagnosis had been life changing:
My son is thriving on the adhd medication. He is off antidepressants and is able to study and cope with life again.1
I was then lucky enough to unexpectedly get enough money to see a private consultant, who diagnosed me with ADHD ... For me, this choice was 100% worth it as it has transformed my life. I am now thriving at work, completing all my chores, and my physical health has also improved as I am able to make healthier choices.1
Bill Colley from the Scottish ADHD Coalition highlighted the difference between ADHD and autism in terms of the availability or otherwise of effective medication for each of these conditions:
There is a critical difference between the ADHD population and those with ASD—although there is, as you will be aware, a huge overlap in comorbidity. In particular, without diagnosis, you cannot get treatment and although there is no medical treatment for autism, there is for ADHD and it is shown to be effective. If young people or adults are not being given access to assessment and diagnosis, they are not getting treatment for a treatable condition.2
Many contributors to the Committee's inquiry took issue with the assumption that individuals should be able to access needs-led support without the need for a diagnosis. They argued that this did not reflect the reality of many people's lived experience. Indeed, a number of contributors described not being believed and being refused support because they had not received a formal diagnosis.
Several witnesses argued during the oral evidence sessions that autistic people and people with ADHD have a right to seek a diagnosis to understand why they may experience challenges in life and what forms of support may help. Rob Holland from the National Autistic Society Scotland argued that, for many, a diagnosis will continue to be an important component of a needs-led approach to support:
Diagnosis and needs-led support should not be either/or. Providing early interventions and meeting needs should be complementary to, and not instead of, a diagnosis. Both diagnosis and support are valuable. Diagnosis is a need in itself ... It is important to say that needs-led support is context specific. It supports someone at a specific point in time—in school, for example—and people have a variety of experiences, with different transition points and major events throughout their lives, and their needs will often change. Having a diagnosis helps that person to navigate through those transitions and build the strategies that help them in those situations. We should not delay diagnosis until somebody’s situation is acute or they are in crisis, because that is no good for the individual and no good for the system.2
The importance of diagnosis was also emphasised by the National Autistic Society Scotland in their written submission to the Committee's call for views:
Receiving a diagnosis is a validating and life-affirming experience for many and helps autistic people to understand themselves, their identity, as well as their strengths and challenges. The assessment process is much more than a diagnosis; it offers the individual a needs assessment, as well as ruling out or identifying other conditions. Moreover, we know that a diagnosis is, unfortunately, often the gateway to support for individuals. Indeed, the reality is that public services are under pressure and will often prioritise allocation of support based on level of need and/or diagnosis. Autistic people also often struggle to be believed when seeking support due to ongoing stigma and discrimination, which makes a diagnosis important to individual.7
Scottish Autism expressed a similar viewpoint in their written submission:
A diagnosis can be vital in supporting a person to better understand themselves and to be better understood and supported by others. While we have heard the Scottish Government argue that a diagnosis is not necessary to receive support, rather that the needs should determine this, we hear on a daily basis that this is not the reality facing people. Moreover, a holistic assessment process should not simply be about confirming or declining a diagnosis, but establishing an individual profile of needs.8
In oral evidence, Dani Cosgrove from STAND highlighted how important it is for parents and carers of children with neurodevelopmental conditions to be able to access a diagnosis:
It means that I, as the parent, have the confidence to know that I am right, and that I will not be told that my child does not have these needs because I have the diagnostic assessment to prove that he does. It gives me the opportunity not only to fight for rights with the school but, if I do not feel that the school is fulfilling them, to take it to the local authority, which has to fulfil my child’s educational rights.2
Asked what the role of diagnosis would be in a neuroaffirming society, several witnesses were quick to point out that, in their view, society was currently not neuroaffirming, and therefore they felt unable to answer this question. Kabie Brook from Autistic Rights Group Highland told the Committee: "If we lived in a neuroaffirming society, life would be so different. We would know when we got there whether the role of diagnosis was still important, but it definitely is now and we know that now".2
In oral evidence, the Minister for Social Care and Mental Wellbeing recognised the importance of assessment and diagnosis but emphasised that the lack of a diagnosis should not become an artificial barrier to support:
I fully recognise the importance that is placed on assessment and diagnosis for a range of reasons ... I reiterate the point that diagnosis is not, and should not be, a prerequisite for support.11
Impact of not receiving the right support or diagnosis
Studies have shown that the life expectancy of autistic people in the UK is significantly lower than for the general population. One study estimated that, on average, autistic people (with no learning disability) live six years less than the general population. The increased prevalence of epilepsy partly explains this discrepancy, as do cases of suicide - which is the leading cause of early death in autistic adults with no additional learning disability.
A similar picture is seen in the life expectancy of people with ADHD in the UK, which is seven and nine years lower than for the general population for males and females respectively. In people with ADHD, this difference is believed to be attributable to an increased prevalence of smoking, substance use and risk-taking behaviours.
In their written submission to the inquiry, the Scottish ADHD Coalition raised concerns that the withdrawal of pathways for ADHD assessment and support in some areas of Scotland would have a detrimental impact on people with ADHD:
The recent withdrawal of ADHD assessment and treatment across Scotland will lead to a significant rise in mortality, a reduction in life expectancy, and reduced quality of life in the affected cohort, and increased costs to the NHS and other publicly funded services which will outweigh the cost savings that have driven the decision. Changes to patient pathways will also severely undermine policy initiatives designed to address the drugs crisis, reduce youth offending and prison overcrowding, improve pupil behaviour and attainment in schools, eliminate child poverty, improve longevity and the mental health and wellbeing of the Scottish population, and to tackle the obesity epidemic. In some areas of Scotland it is now no longer possible for an adult with ADHD to undergo an assessment or receive treatment despite suffering chronic impairment as a result of the condition.1
Matthew Day from Number 6 expressed similar concerns that late diagnosis or misdiagnosis could have a significant negative impact on people's lives:
For a lot of neurodivergent people I have worked with, the impact of not getting a diagnosis earlier was that they ended up in prison or, in the cases of many women who were seen as seeking a diagnosis too aggressively, were diagnosed with borderline personality disorder.2
Many people with lived experience who responded to the Committee's call for views shared experiences of having been misdiagnosed before realising they had ADHD and/or were autistic. Such experiences were particularly prevalent amongst women who reported having been misdiagnosed with mental health conditions. For example:
After years of being prescribed medications for borderline personality disorder, depression and anxiety and nothing improving my mental health nurse queried ADHD. […] I waited around 4 years, however if I am being honest I actually waited around 20 years as was misdiagnosed the majority of my life.3
I have been wrongly diagnosed with many different things since I was a child. In the 90s, ADHD for girls was practically unheard of.3
I was treated for anorexia for almost 30 years and misdiagnosed with BPD [Borderline Personality Disorder]/ EUPD [Emotionally Unstable Personality Disorder] for all of this time - and treated terribly because of it. What I now know is autism and ADHD (e.g. meltdowns, sensory sensitivities, emotional irregulation issues, monotropism / intense interests, difficulty with change and need for routine) was seen as symptoms of BPD and I was forcibly medicated, sectioned and transferred to hospitals all over the UK. It's been difficult to get appropriate treatment for my anorexia because of it and now I am told (frequently) that after 30 years of anorexia and with co-occuring autism, there's little hope / help for me.3
During an oral evidence session, Sofia Farzana from Scottish Ethnic Minority Autistics addressed the dangers posed to individuals of being prescribed the wrong medication when neurodevelopmental conditions were not taken into account:
An example would be not assessing for ADHD. That is quite a big thing, particularly for women, given the whole interaction of ADHD and female hormones. If that is not seen properly, females cannot access the correct hormonal support. Another example is being prescribed the wrong medicine. For example, I had a case of someone who was refused ADHD assessment after successfully getting an autism diagnosis and who was then prescribed sertraline, which just made the ADHD worse, to the point where the person sustained an injury because of the hyperactivity and the inability to maintain focus ... The person might be prescribed antidepressants for sleep but because of the ADHD they cannot take medication consistently ... Not being able to take antidepressants consistently has consequences and the person I am talking about experienced suicidal ideation.2
She went on to highlight other challenges faced by autistic people and people with ADHD who do not receive the right support, including high rates of domestic abuse and complex post-traumatic stress disorder (PTSD):
Autistic people have the highest rate of suicide and the highest rate of abuse, including domestic abuse. If you put those statistics together, you should not be surprised that it is quite common for somebody who is neurodivergent to also have complex PTSD ... Knowing that you are autistic or ADHD improves relationships because you know yourself better. It will help you understand that, for example, you are in a relationship that is not good for you, and it will empower you—because you have improved mental health, you have a better understanding and you are around people who understand you.2
In oral evidence, the Minister for Social Care and Mental Wellbeing reiterated the importance of diagnosis but went on to emphasise his view that receiving a diagnosis should not be a prerequisite for accessing support:
I stress that I fully recognise the importance of assessment and diagnosis, not only for individuals but for families, in order to understand need and for reasons of identity and validation; in some circumstances, assessment and diagnosis are important with particular reference to medication in relation to ADHD. We want to provide a needs-led approach, recognising that, consistent with our national specification for children and young people, a diagnosis is not a prerequisite for accessing support—and nor should it be.8
The Committee acknowledges there are a number of valid reasons for seeking a diagnosis for autism and/or ADHD, including:
Giving individuals a sense of validation and understanding about themselves as people, including understanding current and past life experiences
Determining what forms of support, adjustments or treatment would be most helpful and giving individuals and/or parents and carers the ability to advocate for these.
At the same time, the Committee also acknowledges fundamental differences between these conditions which mean the reasons for seeking a diagnosis will vary between autism and ADHD. In particular, the Committee notes that, as a medically treatable condition, there are especially important reasons for receiving a positive diagnosis for ADHD since this will ensure the individuals affected are able to access the correct medication to treat their condition.
While welcoming the Scottish Government's recognition of the importance of diagnosis while committing itself to ensuring receiving a diagnosis is not a prerequisite for accessing support, the Committee remains concerned that, in reality, the lack of a formal diagnosis has become a barrier to accessing support for too many individuals.
The Committee therefore calls on the Scottish Government, in responding to this report, to set out what action it is taking or plans to take to ensure the lack of a formal diagnosis is not used as an artificial barrier to accessing support and to encourage practitioners to fully explore what support can be made available while individuals are waiting to receive a formal diagnosis.
The Committee highlights the particularly urgent need for formal diagnosis for those individuals who require it to be able to access the correct medication to treat their condition. It therefore calls on the Scottish Government to set out what strategies it is pursuing to reduce waiting times for assessment and diagnosis of these individuals.
Private diagnosis and shared care
During the inquiry, the Committee heard evidence from many people with lived experience who had obtained an assessment for ADHD and autism, or both, privately. Most described having been forced into this position as a result of experiencing long waiting times for NHS assessments, rather than this being an active choice to use private healthcare. Many described incurring a significant financial burden not only as a result of paying for the initial assessment but also due to the ongoing cost of private prescriptions. For example:
When I called the NHS Lothian switchboard I was informed that they were seeing patients registered in 2018, indicating a 6 years delay and putting my assessment at ~2028, three years away from now. In the meantime I had to go out and seek an assessment privately, which cost me £1,500 for the diagnosis and then £3,500 more for titration [the process of gradually adjusting the dose of a drug to find the optimal amount] over 12 months with monthly appointments. On top of the £5,000 spent I am now expecting to spend further £5,000+ over the course of five years (2023-2028) obtaining medication which costs ~£60pm + £30 for private prescription. TEN THOUSAND pounds to live a normal life.1
Been on the NHS waiting list for over 2 years, decided to go private as daily struggles were too much.1
I paid several thousands of pounds, which I am still paying off four years later.1
Some respondents to the Committee's call for views argued that an unequal system had developed whereby, in many cases, prompt diagnosis was only available to those who could afford to pay for it. At the same time, some of those who had been diagnosed privately with ADHD reported subsequently being unable to access medication on the NHS because their GP refused to offer "shared care".i Whether or not the GP agrees to this arrangement depends on a number of factors including specific health board guidance, quality of diagnosis, the nature of any other medication the patient may be taking, and the GP's own workload.
The Committee heard from many contributors to the inquiry that refusal to accept shared care agreements in the case of ADHD has caused significant distress, particularly when patients had been under the impression, at the point of seeking a private diagnosis, that shared care would be available. Some pointed out that, sometimes, the same clinicians offer both private and NHS assessments. For example:
I have also been told that they absolutely would not take on shared care, even though it would be a NHS consultant psychiatrist that would diagnosis me.1
I first realised that i possibly had ADHD in 2022, after the birth of my second child. The symptoms were becoming debilitating, and I sought help from my GP. They were very dismissive but put me on a waiting list anyway. Eventually in late 2024 I couldn’t cope with the symptoms anymore, and took out a loan for a private diagnosis, after consulting my GP who assured me they would offer shared care. After diagnosis and trying different medications, I am now on the strongest dose of methylphenidate, which is very expensive. When the private doctor sent the shared care agreement to my GP, they were informed that the GP no longer offers shared care, as of the previous month. This has left me in limbo, still having to pay a high price for the medication that has been working for me.1
There is no shared care in place in NHS Lothian. The refusal of CAMHS after GP referral was a severe blow. GP Practice has said currently they will not accept private diagnoses from private providers despite them being NHS accredited and conforming to NICE standards which is accepted in NHS England ... I will have no Shared Care agreement and will have to fund medication and any further care myself. It seems that this is a postcode lottery rather than a blanket acceptance of private diagnoses across Scotland.1
Many contributors to the inquiry contrasted this negative experience of accessing shared care in Scotland with the situation in NHS England where, under the NHS Choice Framework, if an individual is referred by a GP for specialist treatment such as an autism or ADHD assessment or diagnosis, they have a legal right to choose an appropriate provider of that treatment.
In its written submission to the inquiry, NHS Highland addressed the challenge posed to the idea of equitable access to services by people opting for a private assessment:
The current delays and limitations within neurodevelopmental services have created a two-tiered system, where those with financial means are increasingly turning to private assessments to bypass long waiting times. This trend raises serious concerns about equity, fairness, and the principle of universal access to healthcare.7
Variability in the quality of private assessments was also raised as an issue in the written submission from the Royal Pharmaceutical Society Scotland:
It is important that where private providers are used, that there is assurance that same standard of assessment and standards are met as used in the NHS, and that their use is equitable across Health Boards.8
The Royal College of General Practitioners Scotland argued that this variability in the quality of private services was one of the reasons why shared care agreements are often difficult to manage:
Patients who receive a private diagnosis frequently request that their GP initiate or continue prescribing high-risk medications under a shared care agreement. However, there are significant concerns regarding the consistency and quality of private assessments, particularly when compared to NHS secondary care standards ... These responsibilities are time-consuming, clinically complex, and currently unfunded under the General Medical Services (GMS) contract.9
During an oral evidence session, Dr Chris Williams from the Royal College of General Practitioners Scotland suggested that GPs might feel more comfortable accepting shared care agreements in the event that:
... There was a healthy relationship with certain clinics, with an understanding that there was a sufficient level of governance, and we were confident that there was a wide range of mental health conditions being considered as part of the assessment ... there would be circumstances in which GPs could be far more trusting of advice that is coming to them from outside their local NHS resource.10
In its written submission to the inquiry, ADHD Right Now argued that shared care agreements should be standardised, as follows:
A national framework for Shared Care Agreements should be developed to eliminate the postcode lottery for medication access. This should include:
Clear national guidance for GPs and health boards with additional support and training where required
Standard documentation templates and eligibility criteria
Mechanisms for auditing Shared Care practices to ensure safety and consistency.11
Dr Pavan Srireddy from the Royal Society of Psychiatrists Scotland, made a similar case for the quality of private assessments to be systematically improved:
If I am going to get an assessment from the private sector, I deserve to know that I am having a good-quality assessment to the same level as what I would get in the NHS, and I would deserve to know that the person undertaking the assessment has the right qualifications, has the right training ... Our view is that the regulation is not robust enough at present ... The current regulatory mechanism does not cover virtual assessments, where the service can be based outwith Scotland, and they make up a large proportion of assessments that are currently undertaken, especially post Covid. That is a huge gap. That leads to concerns about the quality of the assessment.10
While advocating more robust regulation of private assessment, Dr Srireddy concluded:
Ultimately, the increase in private sector assessments is simply a consequence of the lengthy waits that we have in the NHS. That is the core of the issue ... Ultimately, the longer-term sustainable goal is everything that we discussed previously: increasing capacity in the NHS and having a wider model that provides support first, rather than focusing on diagnosis.10
The Committee has been concerned to hear evidence of many individuals being forced to seek a private diagnosis, often at significant financial cost, due to long waiting times for accessing neurodevelopmental assessment and diagnosis via the NHS. The Committee is particularly concerned that this risks creating a two-tier system where timely access to diagnosis is based on an individual's ability to pay.
The Committee has been similarly concerned to hear evidence that the quality of assessments and diagnoses acquired privately can be variable. The Committee therefore urges the Scottish Government, in responding to this report, to set out what action it is taking or plans to take to promote a level playing field in standards of assessment and diagnosis across the public and private sectors.
The Committee further notes the negative experiences of many individuals, having acquired a private diagnosis, of getting their GP to recognise that diagnosis or to agree to provide "shared care". The Committee recognises that greater reliability of standards for assessment and diagnosis, whether provided privately or through the NHS, are needed to give GPs the confidence to accept "shared care" agreements.
The Commitee also recognises that, until NHS capacity is significantly expanded, individuals seeking private assessment and diagnosis is likely to be an ongoing fact of life. In these circumstances, it calls on the Scottish Government to work with Healthcare Improvement Scotland, health boards and GPs to address problems with shared care agreements and to develop a more consistent approach to their use.
Transitions
During their lifetime, neurodivergent people in Scotland can experience a number of different categories of transition. Transitions are any change from one stage of life to another, and can include:
in healthcare, transitions between Child and Adolescent Mental Health Services (CAMHS) and Adult Mental Health Services (AMHS) or similar.
in education, transitions between primary and secondary schools, college, and university.
in employment, transitions between different jobs or into/out of employment.
in social security, transitions between access to different support mechanisms such as the Child Disability Payment and Adult Disability Payment.
These transitions form a key part of a neurodivergent person's life and can be very challenging to navigate. Current policy governing transitions includes a Principles of Transition document published by the Scottish Government. This sets out guidance for young people moving between CAMHS and Adult Mental Health Services. In addition, the Getting It Right For Every Child (GIRFEC) policy and guidance highlight the importance of well-planned and supported transitions. Despite this, as outlined in the SPICe briefing on Neurodevelopmental Pathways and Waiting Times in Scotland, neurodivergent people still report experiencing difficulties in many aspects of transitions, especially between mental health services and educational institutions. On the other hand, the National Neurodevelopmental Specification addresses transitions as one of its key standards and, as reported through the Scottish Government's previous consultation on proposals for a Learning Disabilities, Autism and Neurodivergence Bill, this has been well-received by the neurodivergent community.
Many written submissions to the inquiry described particular challenges encountered by individuals at certain points of transition, particularly between accessing child and adolescent and adult services, and the risk some people face of transitioning out of services before they are seen. For example, in its written submission, Salvesen Mindroom Centre stated:
The transition from NHS Child and Adolescent Mental Health Services (CAMHS) to NHS Adult Mental Health Services is widely recognised as a critical point where many young people fall through the gaps. Despite having spent years on CAMHS waiting lists, young people often face the frustrating reality of starting over, joining the bottom of an adult services waiting list for assessment or support. This discontinuity not only delays access to care but can also exacerbate existing mental health challenges during a vulnerable life stage.1
Autistic Rights Group Highland (ARGH) Scotland raised a similar point in its written submission
We are also aware that the crisis extends to the children's waiting lists: children who 'age out' of the child system whilst on a waiting list will join the bottom of the adult waiting list increasing their wait time significantly and without appropriate support in the meantime during their formative years / years of education and upon leaving school (as I said support is in theory based on need not diagnosis but in reality this does not happen).2
On the issue of managing transitions between child and adults services, NHS Highland also raised concerns in its written submission:
There is currently no nationally implemented transitional framework for neurodivergent young people moving from child to adult services in Scotland. While the National Neurodevelopmental Specification for Children and Young People (2021) set out clear expectations for early intervention and support, there remains a critical gap in continuity of care into adulthood. Embedding a co-produced, cross-sector transition framework—aligned with the Principles of Good Transitions and supported by dedicated resources—would ensure that neurodivergent individuals experience seamless, person-centred support across the lifespan, reducing the risk of disengagement and unmet need during this pivotal stage.3
Convention of Scottish Local Authorities (COSLA) raised related concerns about the transition from education to post-education settings:
The lack of structured post-education pathways may leave young people vulnerable to disengagement, and wider more serious impact. Currently a significant percentage of children and young people in school settings are identified as having additional needs. Ensuring these needs are met post school places a significant pressure on the system that requires appropriate consideration, planning and investment.4
People with lived experience who responded to the Committee's call for views similarly highlighted the negative impact of poorly managed transitions. Some parents, for instance, felt their children should have received more support during the transition from primary school to secondary school:
Education department has completely failed her. No enhanced transition to secondary. Suffered autistic burnout S1 and hasn't been able to attend for 3 years.5
My child aspired to be a Dr, yet now has no qualifications at the age of 16. She has trauma as well as probable autism so her needs are complex. Had Camhs intervened at a much earlier stage, to give her the help she desperately needed at the start of the high school transition, then her future may have looked brighter.5
Several witnesses suggested that third sector support services can be helpful during points of transition. Matthew Day from Number 6 highlighted the work of Aspire, a transitions team in Edinburgh that previously worked with 16 and 17 year olds. He informed the Committee that, after Aspire was disbanded, it had become difficult to identify individuals in schools who might need support with transitions. Sofia Farzana from Scottish Ethnic Minority Autistics argued that, in her experience, maintaining consistent relationships was key to successfully supporting children and young adults with neurodevelopmental conditions:
There need to be relationships with people between the ages of 16 and 24 and who are in that transition. They are not just transitioning out of school; they are transitioning into work or education, and as soon as you are 18 you are an adult ... When it comes to moving out of home, with all the bills and so on, there is so much to consider. If you have a relationship with somebody, they can provide the help that you got beforehand with, for example, sleep or with moving from child disability payment to adult disability payment, or even with caring issues ... Relationships are not there, but that is what we need. We need someone who we can trust and can talk to. We need consistency.7
The Committee recognises the particular importance of well managed transitions for people with neurodevelopmental conditions but regrets that too many report experiences of poorly managed transitions and a lack of appropriate support during transitional periods in their lives.
The Committee highlights evidence of particular challenges for people with neurodevelopmental conditions in making the transition from child to adult services at a particularly vulnerable stage of their lives - and the crucial importance of maintaining consistent relationships during this period to be able to successfully navigate this transition. The Committee has also heard similarly concerning evidence of poor planning and support for children with neurodevelopmental conditions in making the transition from primary to secondary school and from education to post-education settings.
In light of this evidence, the Committee calls on the Scottish Government, in responding to this report, to set out what action it is taking to ensure proper implementation of its Principles of Transition policy, GIRFEC policy and guidance and the relevant provisions of the National Neurodevelopmental Specification, so that people with neurodevelopmental conditions do not experience any further negative effects from poorly planned and supported transitions.
In so doing, the Committee further calls on the Scottish Government to address an apparent gap in the National Neurodevelopmental Specification for Children and Young People by ensuring there is absolute continuity of care throughout these important transitions and into adulthood.
The Committee pays particular tribute to the work of third sector organisations in supporting people with neurodevelopmental conditions during periods of transition and calls on the Scottish Government, in responding to this report, to set out what it is doing to support third sector organisations operating in this space.
Role of third sector
Throughout the inquiry, the Committee has heard evidence of how much autistic people and people with ADHD value the support they have received from third sector organisations. Mark McDonald from Scottish Autism told the Committee that this applies particularly to those who are unable to access statutory support without a formal diagnosis. He explained:
People can contact our advice line or access our community services at any stage on their diagnostic journey. They do not need to have achieved a diagnosis to access those support services. Broadly speaking, that is the approach that is taken across the third sector, often because support is not available already from statutory services. The third sector meets need that exists that the statutory services are not dealing with.1
In its written submission to the Committee, the Scotland Yard Adventure Centre highlighted the important role it and other third sector organisations play in supporting children and families:
Many families cannot access a support service in their local area prior to diagnosis so they are left isolated. The third sector is able to deliver services to families that are flexible to their needs, greater funding to allow the delivery of services pre-diagnosis (such as The Yard) would be invaluable to families. Families often talk of The Yard as a life-saver during this time, there are so few services that will accept children without a diagnosis. Often children come to The Yard in their early years before a diagnosis and we are able to support them through the diagnosis journey and onto into early adulthood, children literally grow up in The Yard. Their families are able to access support either through informal/semi-formal peer support or through our Family Workers.2
Anya Kennedy from the Royal College of Occupational Therapists highlighted the important work undertaken by the third sector and particularly drew attention to its role in involving people with lived experience in providing support:
A lot of what is currently provided is provided through the third sector. That is particularly the case when it comes to post-diagnostic work. Third sector organisations also involve a lot of people who identify as neurodivergent or have lived experience of neurodivergence. That is essential to working together to progress those services, because those people have knowledge and skills that cannot be learned, which come from their daily experience.3
Throughout the inquiry, the Committee heard extensive evidence to suggest that many individuals particularly welcomed receiving support from other people with neurodevelopmental conditions who have a better understanding of what they are experiencing. The Committee also heard that such support is often delivered by third-sector organisations run by and for autistic people and people with ADHD. During an informal engagement session with a peer support group for people with ADHD , one participant "described the best support they have had throughout their journey as having come from interacting with other people with ADHD".4
Lyndsay Macadam from SWAN Scotland, raised concerns that a tendency towards larger organisations competing successfully for contracts could result in smaller groups run by and for people with neurodevelopmnetal conditions being excluded. She went on to emphasise the positive impact SWAN Scotland have had despite experiencing ongoing challenges with securing long-term funding:
Last year, I had a team of three people. We ran 310 groups in 22 locations across Scotland, from Shetland to the Borders, with just those three people and a team of volunteers. Nobody else can do that apart from us ... From feedback from the reporting that we carry out for our funders, we know that ... In one hour with us, they get more help than they have had elsewhere throughout their lives. However, we are already struggling to access the funding that we need to be able to see them.1
In its written submission, Scottish Ethnic Minority Autistics called for the Scottish Government to "fund community based care / grassroots organisations who support peers, in particular underrepresented communities like racialised autistics".6
Asked whether the voluntary sector should be given an on-going, long-term role to deliver assessments and diagnoses in concert with other forms of support, Kabie Brook from Autistic Rights Group Highland gave a cautious response:
I just get very nervous about the prospect of things that I feel should sit within the NHS not actually doing so. It is good that we have some services doing assessments, in some areas, to try to reduce the awful waiting lists. However, it feels almost as though, by using such a pathway, the NHS would be washing its hands of us.1
While acknowledging that third sector organisations were able to deliver good value for money and added flexibility in their approach to providing support, several other witnesses expressed concern that this was partly due to staff working in the third sector receiving relatively lower pay. They also expressed concern that a willingness in third sector organisations to continue providing support, even at comparatively lower rates of pay, was something that could be exploited. They therefore called for a commitment to more sustainable funding models that would allow third sector organisations to plan more effectively and to improve the longer term reliability of the support they provide.
During oral evidence, the Minister for Social Care and Mental Wellbeing recognised that the third sector "has a profoundly positive impact, particularly when it comes to peer support and helping to tackle isolation and provide opportunities for engagement and socialising". 8Asked for specific examples of how the Scottish Government is supporting third sector organisations in this area, the Minister told the Committee that the Scottish Government continues to support Scottish Autism to run its Autism Advice Line and is currently funding nine organisations working with autistic adults through the Autistic Adult Support Fund.
The Committee pays tribute to the crucial work of third sector organisations in providing support to those people with ADHD and autism who have not received or are yet to receive a formal assessment or diagnosis from statutory services. It notes that, without access to such support, many individuals would be left isolated and unsupported.
The Committee further commends the work of the third sector in involving people with lived experience of neurodevelopmental conditions in delivering the support it provides - and notes how much their involvement is welcomed by individuals using these services.
Given how crucial third sector support can be in this area, the Committee welcomes the Scottish Government's ongoing commitment to supporting third sector organisations through vehicles such as the Autistic Adult Support Fund. It calls on the Scottish Government, in responding to this report, to set out what further actions it plans to take to continue to support the third sector and to place funding for third sector organisations on a more sustainable long-term footing.
Whole society approach
Throughout the inquiry, many contributors argued that, in the longer term, improving the lives and circumstances of autistic people, people with ADHD, and those with other neurodevelopmental conditions, would require a whole society, multi-systems approach.
In their recent paper, Multi system solutions for meeting the needs of Autistic and ADHD people in Scotland, the Royal College of Psychiatrists in Scotland also made the case for the needs of people with neurodevelopmental conditions (NDCs) to be addressed through a whole society approach:
NDCs have a major impact across multiple domains including social care settings, educational institutes and the workplace. Recognition and support for people with NDCs are therefore not the exclusive remit of health services, but requires responses from all areas of society. This challenge is far bigger and more consequential than previously anticipated and planned for. The current approach therefore cannot continue. It is a society wide issue, requiring a multi system, public health-based approach similar to those adopted in other areas (for example climate change, poverty, knife crime & obesity).
Thelma Bowers from NHS Ayrshire and Arran told the Commitee that such an approach was already being successfully undertaken in her health board area:
For three years, all partners have adopted a whole-system, multi-agency approach, and have worked together across education, social care, children’s services and mental health services to address issues within the resources that are available ... Implementation groups were set up in east, south and north Ayrshire, and the group in south Ayrshire implemented a multi-agency panel approach.1
Thelma Bowers went on to argue that implementing such a whole systems approach more widely would also require an integrated, cross-sectoral approach to workforce planning:
We should look at having a national workforce plan. This is a public health issue. How then do we align our existing workforce and expertise across the whole system, so not just in mental health but in education and the third and independent sectors? What can we deliver as a whole society at those different levels to grow that expertise?1
Dr Gill Kidd from Child Heads of Psychology Services expressed similar support for a whole systems approach but went on to argue that, for it to be successful, there would be a corresponding requirement for a more integrated, cross-sectoral approach to the distribution of funding:
We must also consider where funding has been directed to. For example, if it is coming into health only, then it would not support the wider framework that we are talking about. We need to think differently about how the whole system is funded and to use a multi-agency approach. Funding also needs to go into education, social work, children’s services and CAMHS so that we can all provide the bits of that service that we need to and for our services to hang together and be sustainable.1
Anya Kennedy from the Royal College of Occupational Therapists told the Committee that many people with neurodevelopmental conditions interacted with a wide range of different public services and suggested this underlined the need for a whole-system approach:
We have a lot of neurodivergent people in our adult mental health services already with and without a diagnosis. A lot of that is hidden in the population. People can be in, for example, adult mental health services, perinatal health services, integrated drug and alcohol services and in the criminal justice system. I have occupational therapists working in all those areas, and I am very aware of how many of the people who they are working with have neurodevelopmental conditions. It is very important that we take a whole-system approach.1
Mark McDonald from Scottish Autism mentioned that one of the reasons his organisation had been supportive of Scottish Government proposals to bring forward a Learning Disabilities, Autism and Neurodivergence Bill was that it sought to reflect a whole society approach to issues faced by people with neurodevelopmental conditions:
One reason why we were so supportive of the proposed learning disabilities, autism and neurodivergence bill and why we are so disappointed that it will not be passed in this session of Parliament is that it was focused on the whole life journey and the whole life experience. This committee is rightly focusing on assessment and diagnosis, but once the individual has achieved that diagnosis, that is not the end of their story. They then have to go into other areas of their life and access or identify support, or advocate to try to get support to be made available.5
Sofia Farzana from Scottish Ethnic Minority Autistics highlighted cases where multiple members of a family can be autistic or have ADHD and argued for a more holistic approach across services to support families in such a situation:
We need to have proper holistic support services. People in our community groups are now interacting with five or six different professionals to get support because they are in burnout and crisis mode. It gets to the point where, because things have got so bad from many different angles, there are too many professionals involved, with people from the courts, the police, social work, education services, speech and language therapy, occupational therapy and the school all working with one family.1
Many submissions to the Committee's inquiry raised particular concerns about a lack of appropriate support for autistic children and children with ADHD in schools. Mark McDonald from Scottish Autism explained that, when children with neurodevelopmental conditions are not coping at school due to a lack of appropriate support, this can result in them being informally excluded from school and their parents having to leave their place of work to look after them:
That happens almost daily and means that at least one parent is locked out of the workforce because they have to be available for the child coming home from school. It also means that the child does not access and benefit from education. Nobody benefits in that scenario.5
Kabie Brook from Autistic Rights Group Highland argued that excluding autistic children from mainstream schools was counterproductive to creating a properly inclusive society:
It seems to me that if you do not have an integrated school and if you are not teaching children from a very young age about what society is and who the members of our communities are, and if some people end up being segregated because they cannot manage to access school, school will continue to be a hostile environment for many neurodivergent people.5
In written correspondence to the Committee, COSLA have highlighted the importance of funding local authorities to provide wider activities for children which can be a valuable source of support and community:
We also recognise the importance of wider locally based opportunities such as sports and learning opportunities that reduce isolation and foster communities of support. Many such opportunities are provided through local authorities who are currently subject to significant fiscal challenge.9
In oral evidence, the Minister for Social Care and Mental Wellbeing underlined the Scottish Government's commitment to taking a whole-systems approach to addressing the needs of people with neurodevelopmental conditions:
The issue is complex. Neurodevelopmental needs span health, education and social care, and they are shaped by a wide range of factors. A traditional national health service waiting list approach is not sufficient. What is needed is a coordinated multi-agency response that focuses on timely, needs-based support and reflects the evolving nature of neurodevelopmental needs and the diversity of individual experiences.10
The Minister went on to outline the Scottish Government's intention that its new task force would take a cross-sectoral approach, bringing together education and health to implement the National Neurodevelopmental Specification.
On the subject of proposals for a Learning Disabilities, Autism and Neurodivergence Bill and the Scottish Government's subsequent decision not to proceed further with these proposals during the current parliamentary session, the Minister told the Committee:
I cannot commit to any specific time, but the undertaking given by my predecessor to publish draft provisions still holds and is one that I will honour.10
The Committee highlights the broad range of evidence it has heard throughout this inquiry in support of a whole society approach as the most effective means, longer term, of supporting people with neurodevelopmental conditions, improving wider public awareness and combatting stigma.
In this context, the Committee welcomes the Scottish Government's commitment that its new task force will take a whole-systems approach, working across the health and education sectors to implement the National Neurodevelopmental Specification.
Beyond this, the Committee calls on the Scottish Government, in responding to this report, to set out what actions it will take to further promote a whole-systems or whole society approach, including:
learning the requisite lessons and developing associated guidance from examples of best practice in whole systems approaches, such as that seen in NHS Ayrshire and Arran;
what, if any, steps it intends to take towards developing a national workforce plan as an important component of a whole-systems approach;
how distribution of funding will be adapted in future to facilitate a more integrated, cross-sectoral approach to support;
promoting educational settings that are more inclusive of people with neurodevelopmental conditions;
addressing the particular needs of families with multiple family members who are living with neurodevelopmental conditions; and
promoting closer collaboration between the various different public services people with neurodevelopmental conditions come into contact with.
The Committee has heard evidence from many contributors to the inquiry who have expressed regret that the Scottish Government has paused plans for a Learning Disabilities, Autism and Neurodivergence Bill, which it was felt would contribute positively towards promoting a whole systems or whole society approach to supporting people with neurodevelopmental conditions. The Committee notes the Minister's commitment, in the absence of further progress on a Bill, to publish draft provisions. It calls on the Scottish Government, in responding to this report, to set out a timetable for publication and to provide further details of what these might cover.
Data
To date, data concerning waiting times specifically for neurodevelopmental assessment has only been made available via Freedom of Information requests and one-off publications. Many submissions to the Committee's call for views made the case for additional data to improve transparency about waiting times and to support service planning.
As set out in the SPICe Briefing on Neurodevelopmental Pathways and Waiting Times in Scotland, in the past, neurodevelopmental cases have been included in CAMHS waiting times statistics. However, in recent years, these cases have been separated from those statistics. This is done in recognition of the fact that neurodivergence is not a mental health condition and that, unless they meet the national referral criteria for treatment by CAMHS, neurodivergent children do not need to be 'treated' in a medical sense. As such, they are not recorded as patients requiring mental health support.
On the subject of data, NAIT's Children's Neurodevelopmental Pathway Practice Framework states:
Data is essential for quality assurance and quality improvement in a neurodevelopmental pathway and it informs service delivery. With better data, local teams are better placed to understand improvement or change required to local neurodevelopmental pathways. In order to monitor the implementation of evidence based guidelines and pathways, services should establish good quality and efficient processes for data collection, linked to standards for the service and local electronic patient record systems.
Many submissions highlighted the existence of a significant data gap in relation to referrals and waiting times for neurodevelopmental assessment in Scotland. In its written submission, the National Autistic Society Scotland (NASS) pointed out that NHS England routinely publishes autism assessment waiting times on its dashboard. NASS argued that it:
Want[s] data on autism assessment referrals and waiting times to be recorded and published in Scotland. In England, this data is routinely collected, published and disaggregated every quarter, yet in Scotland there is currently no available data on waiting times for autism assessment. This would help to provide a clearer idea of the national picture, specifically which areas are performing well and where improvements or additional resource is needed.1
The ADHD Coalition agreed with this viewpoint, arguing that improved data collection could support planning and thus improve efficiency.
STAND's written submission also commented on the lack of consistent data on waiting times and outcomes and the challenges this creates in terms of accountability and service improvement:
In our experience, it is extremely difficult to understand what is actually happening in relation to referral pathways, delays, and waiting lists. There is no consistent public reporting (that we are aware of) on waiting times or outcomes, and there is also a lack of consistency in terminology across Scotland. For example, some areas refer families to “CAMHS” for neurodevelopmental assessment, while others treat this as a separate pathway. This makes it difficult to compare services or hold systems accountable. Greater clarity and standardisation in language is required, and robust data gathering and reporting will be essential to properly design, deliver and monitor services.2
The Royal College of General Practitioners Scotland highlighted the impact this lack of information can have on patient trust:
The absence of clear and accessible information on waiting times creates uncertainty for both GPs and patients. This lack of transparency undermines trust and can damage the therapeutic relationship, particularly when patients are left to manage their condition for extended periods without specialist input.3
During an oral evidence session, representatives from NHS Highland, NHS Ayrshire and Arran, NHS Tayside and Child Heads of Psychology Services expressed a collective desire to see the development of national standards for reporting on data. However, they also highlighted the barriers to improved data gathering that exist within current systems. They suggested that specific challenges arose from data being processed on a variety of different software, some of which allowed for easier reporting than others, as well as data being located across different systems, for instance across child and adult services. They also argued that data from specialist services ought to be collated together with data from other services that refer people to pathways, such as GPs and schools.
Thelma Bowers from NHS Ayrshire and Arran made the case for much greater standardisation of data gathering:
Having standards, frameworks and a mandate around that agenda certainly would drive it forward and make it more of a priority. Unless we have data—real information about what is happening in our communities, our referral patterns, and our assessments at every level—it is difficult to inform what the future should look like and the changes that we need to make to the system. The situation has been made more complex because those issues run across the whole system.4
Similarly, Dr Gill Kidd from Child Heads of Psychological Services argued for clear and consistent guidance on data gathering and reporting:
It would be helpful to have national data reporting to enable us to be really clear about what you want us to report on and how you want us to do so and, beyond that, to consider how each health board could do that in a robust way.4
In oral evidence, the Minister for Social Care and Mental Wellbeing acknowledged the need for improved data:
We also recognise the need for better data to inform planning and improvement. Work is under way with health boards and local authorities to get a clearer understanding of service demand and provision.6
Accompanying the Minister, Stephen McLeod from the Scottish Government explained that one of the aims of the new Scottish Government task force was to review the available data with a view to improving accountability and utilising data more effectively across systems:
We have talked about the data being poor, and one of the longer-term actions of the task force is to agree on the data points and understand the support arrangements in each area ... Use the information that we gather routinely— particularly from universal services such as health visiting and education, but also from elsewhere, such as general practitioners—and to use that data better, by digitising it and contributing it to any future professional assessments ... At the end of the day, we have to have better data on outcomes for children, young people and families, so that all the statutory bodies and players in this game can be accountable.6
The Committee highlights the importance of consistent, reliable, high quality data on neurodevelopmental referrals and waiting times across Scotland to be able to plan services effectively and to make ongoing improvements.
In this context, the Committee has been concerned to hear evidence of significant gaps and a lack of standardisation in data gathering, including across NHS Boards.
The Committee therefore calls on the Scottish Government to set out what steps it plans to take to enable routine quarterly reporting of data on referrals and waiting times for autism and ADHD, underpinned by national guidance.
While welcoming that this will be an area of longer term focus for the new Scottish Government task force, the Committee further calls on the Scottish Government to address how it intends to overcome potential barriers to more consistent data collection and reporting, such as use of different software systems and location of data across multiple different systems and services.
The Committee considers that future work to improve data gathering and reporting should culminate in the establishment of a comprehensive dashboard, with the aim of improving transparency, enhancing effectiveness, and reinforcing patient trust.
Annexe A: Extracts from the Minutes of the Health, Social Care and Sport Committee Meetings
24th Meeting, 2025 (Session 6), Tuesday 23 September 2025
The Committee received a background briefing from the National Autism Implementation Team (NAIT).
25th Meeting, 2025 (Session 6), Tuesday 30 September 2025
The Committee took evidence from—
Bill Colley, Chair, Scottish ADHD Coalition; Dani Cosgrove, Chief Operating Officer, Stronger Together for Autism and Neurodivergence (STAND); Rob Holland, Director, National Autistic Society Scotland; Mark McDonald, Media and Policy Officer, Scottish Autism;
and then from—
Kabie Brook, Chair, Autism Rights Group Highland (ARGH); Matthew Day, National One Stop Shop Manager, Number 6; Sofia Farzana, Director and Co-founder, Scottish Ethnic Minority Autistics (SEMA); Lyndsay Macadam, Chief Executive Officer, SWAN Scotland.
The Committee agreed to consider the evidence it heard earlier at its next meeting.
27th Meeting, 2025 (Session 6), Tuesday 7th October 2025
The Committee took evidence from—
Dr Pavan Srireddy, Vice Chair, Royal College of Psychiatrists in Scotland; Glenn Carter, Head of Scotland Office, Royal College of Speech and Language Therapists; Dr Chris Williams, Vice Chair, Royal College of General Practitioners Scotland; Anya Kennedy, Divisional Lead Occupational Therapist, Royal College of Occupational Therapists;
and then from—
Thelma Bowers, Head of Mental Health Services, NHS Ayrshire and Arran;Louise Bussell, Board Nurse Director, NHS Highland; Dr Gill Kidd, Consultant Clinical Psychologist, Child Heads of Psychology Services (CHOPS); Cath Malone, Consultant Clinical Psychologist/Lead Clinician, NHS Tayside.
The Committee considered the evidence it heard earlier under agenda item 2 and at its last meeting.
The Committee agreed to change the title of the inquiry to “ADHD and autism pathways and support”.
28th Meeting, 2025 (Session 6), Tuesday 28th October 2025
The Committee took evidence from—
Tom Arthur, Minister for Social Care and Mental Wellbeing, Gavin Gray, Deputy Director, Mental Health, Stephen Mcleod, Professional Adviser, Mental Health, and Lynne Taylor, Professional Adviser, Mental Health, Scottish Government.
Clare Haughey MSP declared an interest as a bank nurse for NHS Greater Glasgow and Clyde.
Dr Sandesh Gulhane MSP declared an interest as a practising NHS GP.
The Committee considered the evidence it heard earlier under agenda item 2.
Annexe B: Official Reports of meetings of the Health, Social Care and Sport Committee
Tuesday, September 30, 2025 - Evidence from third sector organisations
Tuesday, October 7, 2025 - Evidence from healthcare professionals and health boards
Tuesday, October 28, 2025 - Evidence from Minister for Social Care and Mental Wellbeing, Scottish Government