Health, Social Care and Sport Committee
Stage 1 report: Assisted Dying for Terminally Ill Adults (Scotland) Bill
Membership changes
The following changes to Committee membership occurred during the Committee's scrutiny:
On 18 June 2024, Joe FitzPatrick MSP replaced Ivan McKee MSP.
On 10 October 2024, Brian Whittle MSP replaced Tess White MSP.
On 30 October 2024, Elena Whitham MSP replaced Ruth Maguire MSP.
The following declarations of interest were made during the Committee's scrutiny:
Dr Sandesh Gulhane MSP declared an interest as a practising NHS GP and as chair of the Medical Advisory Group set up to advise and inform the Member in Charge of the Bill in advance of its introduction.
Emma Harper MSP declared an interest as a former NHS Scotland and NHS England employee and as a registered nurse.
Clare Haughey MSP declared an interest as holding a bank nurse contract with NHS Greater Glasgow and Clyde, as being currently registered with the Nursing and Midwifery Council, and as having commissioned the Scottish Mental Health Law Review when she was a Minister.
Elena Whitham MSP declared an interest as a member of Humanist Society Scotland, as a member of the Cross-party group on End of Life Choices, and as a Canadian citizen.
Executive summary
This report sets out the results of the Health, Social Care and Sport Committee’s scrutiny of the Assisted Dying for Terminally Ill Adults (Scotland) Bill at Stage 1.
The Committee acknowledges strongly held views on all sides of the debate on assisted dying, which it has considered carefully as part of its Stage 1 scrutiny. We are grateful to everyone who has contributed to our scrutiny and acknowledge the considered and respectful way in which individuals and organisations have done so.
There is broad recognition across the Parliament that the proposed legalisation of assisted dying is a matter of conscience. On that basis, the Committee has chosen to make no overall recommendation concerning the general principles of the Bill.
At the same time, the Committee has identified a number of areas which it has concluded would benefit from further consideration as part of formal Stage 2 proceedings, should the Bill be approved at Stage 1.
Palliative care provides physical and emotional support to people at the end of life. The Committee believes that everyone who needs it should be able to access good quality palliative care at the end of their lives. Regardless of the outcome of this Bill, we hope the current debate will provide a catalyst for further improvements to be made to the quality and availability of palliative care services in Scotland.
The Committee has considered those human rights under the European Convention on Human Rights that are engaged by the Bill. We have concluded that the following will be important factors that inform individual members of the Scottish Parliament in deciding how they wish to vote on the general principles of the Bill:
the likelihood and seriousness of a perceived risk that the Bill may be subject to human rights based legal challenge that could result in eligibility for assisted dying being extended over time; and
the extent to which it strikes an appropriate balance between providing a right for terminally ill adults to access assisted dying and the requirement to protect vulnerable groups.
If the Bill progresses to Stage 2, we have also concluded that the safeguards in the Bill and its compliance with human rights requirements could be strengthened via amendments to establish an independent oversight mechanism such as an independent review panel or a potential monitoring role for the Chief Medical Officer.
On balance, we are satisfied with the rationale of Liam McArthur (as the member in charge of the Bill) for not including a timescale for life expectancy in the definition of terminal illness. However, the following areas may require further clarification should the Bill progress to Stage 2, to ensure this definition meets its intended purpose:
the minimum age-related eligibility criterion, currently proposed as 16, where key stakeholders and young people should be consulted as part of that further consideration; and
the residence criterion, where we welcome Mr McArthur’s willingness to consider potential amendments at Stage 2.
We believe the issue of capacity would benefit from further consideration via amendment should the Bill progress to Stage 2, including:
further reflection on the resource implications for the medical professions of assessing capacity of those requesting assisted dying;
ensuring the capacity of people with a mental disorder is assessed in a way that is fair and non-discriminatory while also giving suitable protection for vulnerable individuals; and
defining how eligibility for assisted dying will be determined for those with fluctuating capacity.
In respect of the process through which individuals can make an initial request for assistance, we believe amendments may be needed should the Bill progress to Stage 2 to address the following:
ensuring suitable legal clarity and protections for medical practitioners, whether they choose to raise assisted dying with their patients or not;
exploring additional safeguards against so-called 'doctor shopping'; and
giving healthcare professionals and individuals requesting assisted dying access to tailored psychological support.
We recognise that the period of reflection in the Bill can be reduced to no fewer than 48 hours in certain circumstances. However, we believe further consideration should be given to whether a default 14-day period of reflection is appropriate.
We recognise practical concerns about the provisions of the Bill on signing by proxy. We recommend that these are addressed via amendment should the Bill progress to Stage 2, based on further advice from the legal profession.
We welcome Liam McArthur’s preparedness to consider further those sections of the Bill that relate to the provision of assistance. We have concluded that a combination of Stage 2 amendments and detailed guidance on self-administration and provision of assistance would be needed. These will be crucial to ensuring absolute clarity and appropriate protection for all parties involved, should the Bill become law.
We have also concluded that, should the Bill become law, both the condition which led to a request for assisted dying and the administration of an approved substance to enable an assisted death should be recorded on the death certificate of the individual concerned. This will provide transparency and aid data collection.
We recognise Mr McArthur’s intention that assisted dying should be delivered via a service model that enables integration with existing services rather than being provided as a stand-alone service. If it becomes law, it will be important to monitor the impact of the Bill on existing healthcare services over time. If the Bill progresses to Stage 2, we believe it may also be appropriate to explore via amendments whether specific aspects of assisted dying would be better delivered on a stand-alone basis, in particular to ensure consistent access across the country.
Should the Bill progress to Stage 2, we believe further attention should be given to amending the wording of the conscientious objection clause in the Bill. This is needed to ensure it provides an appropriate level of legal clarity and certainty for all parties involved in the assisted dying process.
Where health practitioners exercise a conscientious objection, we believe there should be a minimum expectation that they will refer patients requesting assisted dying on to a colleague who does not share such an objection. As a bare minimum, they should provide additional information about the process. We note concerns that creating a 'no duty' clause (meaning those exercising a conscientious objection would not be required to refer patients on) could create unreasonable barriers to access to assisted dying.
We believe the potential inclusion of a 'no detriment' clause would merit further investigation via amendment should the Bill progress to Stage 2. The purpose of such a clause would be to protect healthcare staff from workplace discrimination due to their involvement or non-involvement in assisted dying.
We have noted Mr McArthur’s willingness to explore further the possibility of creating an 'opt-in' model of participation in assisted dying for health practitioners. We consider this to be an area that may warrant further debate and amendment if the Bill progresses to Stage 2.
Irrespective of whatever position the Parliament takes on allowing or prohibiting institutional objection, we believe amendments will be needed should the Bill progress to Stage 2 to provide further clarity so institutions understand how they will be permitted to act should the Bill become law.
There are significant discrepancies in estimates of training costs associated with the Bill. These costs may also vary significantly according to a number of factors. Should the Bill become law, we would expect the Scottish Government to set out how it intends to meet the associated costs of training in a way that does not negatively affect available funding for existing services.
We have taken a particular interest in potential alternative models for assessing coercion, such as that created in relation to living donors by the Human Tissue Act 2004. We believe such alternative models should be explored further via amendments should the Bill progress to Stage 2.
We welcome Mr McArthur’s preparedness, should the Bill be approved at Stage 1, to consider mechanisms for reviewing and updating guidance on coercion. This will ensure health practitioners are suitably equipped to assess coercion effectively and to allow the related offence created by the Bill to be appropriately policed.
We note the potential competence-related issues involved in the practical implementation of the Bill. We welcome the Scottish Government’s commitment, should the Bill progress beyond Stage 1, to open dialogue with the UK Government with a view to resolving these. We call on the Scottish Government to keep the Parliament regularly updated on progress.
The Committee believes certain aspects of the information, reporting and review provisions of the Bill may warrant further consideration and amendment should the Bill progress to Stage 2. These include:
additional detail to be included in the forms set out in the Bill’s schedules;
additional information to be collected as part of the review process;
whether five years is an appropriate review period for the legislation; and
potential inclusion of a 'sunset clause', meaning the legislation could not remain in force beyond a defined period without a further vote in the Parliament.
In conclusion, the Committee makes no overall recommendation on the general principles of the Bill. However, we hope this report will be helpful to individual members of the Scottish Parliament in deciding how they wish to vote at Stage 1, and in informing further detailed scrutiny should the Bill progress to Stage 2.
Introduction
A draft proposal for a Member's Bill on Assisted Dying for Terminally Ill Adults was originally lodged in the Scottish Parliament by Liam McArthur MSP on 22 September 2021. A consultation on this proposal ran from 23 September 2021 until 22 December 2021 and received 14,038 responses. Of these, 81 were from organisations. 13,957 were from individuals, including academics, professionals and members of the public.
A summary of responses to the Member's consultation was published along with a final proposal on 8 September 2022. On 10 October 2022, Liam McArthur obtained a right to introduce the Assisted Dying for Terminally Ill Adults (Scotland) Bill in the Scottish Parliament.
After the close of the consultation, the Member in charge of the Bill invited a group of individuals to form a Medical Advisory Group (MAG) to advise and inform him ahead of the Bill being introduced. This was chaired by Dr Sandesh Gulhane MSP and included ten other professionals, experts and academics. The MAG published its report on 12 December 2022 and this was considered as part of the Bill drafting process.
Liam McArthur introduced the Assisted Dying for Terminally Ill Adults (Scotland) Bill1 in the Scottish Parliament on 27 March 2024. In preparing the Bill and its accompanying documents, Mr McArthur was supported by the Parliament's Non-Government Bills Unit.
The Health, Social Care and Sport Committee was designated as lead committee for Stage 1 consideration of the Bill on 16 April 2024.
Under the Parliament's Standing Orders Rule 9.6.3(a), it is for the lead committee to report to the Parliament on the general principles of the Bill. In doing so, it must take account of views submitted to it by any other committee. The lead committee is also required to report on the Financial Memorandum and on its Delegated Powers Memorandum.
Overview of the Bill
The Policy Memorandum1 accompanying the Bill describes the Bill's aim as being:
...to allow mentally competent terminally ill eligible adults in Scotland to voluntarily choose to be provided with assistance by health professionals to end their lives.
The Policy Memorandum further states:
The Bill establishes a lawful process for an eligible person to access assisted dying, which is safe, controlled and transparent, and which the Member believes will enable people to avoid the existential pain, suffering and symptoms associated with terminal illness, which will in turn afford the person autonomy, dignity and control over their end of life.
The Bill contains 33 sections and 5 schedules, which can be broken down as follows:
Sections 1 to 3 establish the lawfulness of the provision of assistance to a terminally ill eligible adult to end their own life, and deal with the criteria which must be met in order for a terminally ill adult to be eligible to request, and be provided with, assistance to end their life in accordance with the provisions of the Bill.
Sections 4 to 14 set out the preliminary procedural steps which must be taken, and how criteria will be assessed and determined, in order for a person to be eligible to be provided with assistance to end their life.
Sections 15 to 20 deal directly with the provision of assistance to an eligible terminally ill adult for them to end their life by self-administered means. This includes provision that there is no duty on anyone, including registered medical practitioners and other health professionals, to participate in the process if they have a conscientious objection to doing so, and also provides that it is not a crime to provide an eligible person with assistance where the requirements of the Bill have been met, and that there is also no equivalent civil liability. These sections also deal with the process after a terminally ill adult has died as a result of taking the substance supplied, including the completion of a final statement and how to record the death on the death certificate.
Sections 21 to 33 deal with general and final provisions which include making it an offence to coerce or pressure a terminally ill adult into requesting an assisted death, provisions relating to the collection and reporting of data, the publication of an annual report, and a requirement to review the Act after five years of operation.
Schedules 1 to 4 contain the forms which are required to be completed, signed and witnessed at various stages of the process. These consist of a first and second declaration form, in which a terminally ill adult asks to be provided with assistance to end their life, two medical assessment statement forms, to be completed by registered medical practitioners, which assess eligibility, and a final statement form, to be completed after a death has taken place.
Schedule 5 sets out criteria that would disqualify a person from being a witness or proxy for the purposes of the Bill.
Further details on the Bill can be found in the Explanatory Notes and Policy Memorandum accompanying the Bill.
Background to the Bill
Legal position
The current legal position differs in Scotland compared to other parts of the United Kingdom in that there is no specific statutory offence of assisting someone’s suicide. By contrast, in England and Wales, under the Suicide Act 1961, and in Northern Ireland, under the Criminal Justice Act 1966, it is not a crime to take your own life, but it is a crime to encourage or assist suicide.
Although assisted dying is not a specific criminal offence in Scotland, a person assisting the death of another person could nonetheless be prosecuted for a range of offences, including murder or culpable homicide.
In England and Wales, all prosecutions for assisting a suicide must have the consent of the Director of Public Prosecutions. The Director of Public Prosecutions has produced specific guidance to outline how the discretion to prosecute will be exercised. There is no similar guidance in Scotland, and the Policy Memorandum concludes that, in Scotland, “...it remains unclear what forms of assistance to die a medic, family member or friend may give to a terminally ill person without fear of being prosecuted”. However, the courts have supported the Lord Advocate’s decision not to produce specific guidance on the basis that the factors outlined in the general Prosecution Code (2023) are sufficiently clear.
Previous attempts to legislate in the UK
There have been multiple previous attempts to legislate on assisted dying in the Scottish Parliament. Jeremy Purvis MSP lodged a proposal for a Member’s Bill in 2005 which failed to gather sufficient support to earn the right to introduce a Bill and subsequently fell. Two proposals lodged by the late Margo Macdonald MSP did secure sufficient support to be introduced as Bills, in 2010 and 2013, but both Bills fell at Stage 1 after failing to secure enough votes from MSPs in support of their general principles.
There have also been a number of attempts to legislate for assisted dying in England and Wales at the UK Parliament via Private Members’ Bills. Bills introduced by Lord Falconer of Thorton in 2014 and by Baroness Meacher in 2021 both fell due to running out of parliamentary time. A Bill introduced by Rob Marris MP in 2015 was defeated at its second reading.
In December 2022, the House of Commons Health and Social Care Committee launched an inquiry into assisted dying/assisted suicide. The Committee published its concluding report on 29 February 2024.
On 5 January 2024, a petition was opened calling for the UK Government “to allocate Parliamentary time for assisted dying to be fully debated in the House of Commons and to give MPs a vote on the issue”. The petition closed for signatures on 5 July 2024. Lord Falconer introduced the Assisted Dying for Terminally Ill Adults Bill in the House of Lords on 26 July 2024.
On 16 October 2024, Kim Leadbeater MP introduced the Terminally Ill Adults (End of Life) Bill 2024-25 in the House of Commons, having been drawn highest in the private members’ bill ballot for the 2024-25 session. The purpose of the Bill, which would apply to England and Wales, is described as being to “...allow adults who are terminally ill, subject to safeguards and protections, to request and be provided with assistance to end their own life”. Following the introduction of Kim Leadbeater's Bill, Lord Falconer announced he would not progress his own Bill.
The Terminally Ill Adults (End of Life) Bill 2024-25 was supported at 2nd Reading on 29 November 2024 by 330 votes to 275. At time of writing, the Bill is currently at Committee Stage in the House of Commons.
Legislation around the world
Around the world, the following countries and jurisdictions are known to have legalised a form of assisted dying or suicide:
Ten American States (Oregon, California, Hawaii, Washington, Colorado, Vermont, Montana, New Jersey, New Mexico, Maine) plus the US district of Washington DC;
All six Australian States (Victoria, Tasmania, Queensland, New South Wales, South Australia, Western Australia) plus Australian Capital Territory;
New Zealand;
Canada;
Colombia;
Belgium;
The Netherlands;
Luxembourg;
Switzerlandi;
Spain;
Portugal.
Meanwhile, a number of other countries and jurisdictions are known to be actively engaged in considerations to legalise forms of assisted dying or suicide.
Within the British Isles, Jersey and the Isle of Man have both recently taken steps towards legislating for forms of assisted dying. On 21 May 2024, the States Assembly of Jersey approved proposals for assisted dying and requested the Minister for Health and Social Services to bring forward primary legislation to permit assisted dying in Jersey for those with a terminal illness; the legislation is expected to be considered by late 2025. On the Isle of Man, a Private Member’s Bill on assisted dying, introduced in 2023, secured support at its second reading and was subsequently scrutinised by an ad hoc Bill committee, which published its report on 28 March 2024. It was subsequently considered by the House of Keys, which voted to approve the Bill at third reading on 23 July 2024, and was then passed (with amendments) by the Legislative Council, the Isle of Man’s upper chamber, on 28 January 2025. On 25 March 2025, the upper chamber approved the Bill at its final reading.
Health, Social Care and Sport Committee consideration
The Committee issued two calls for evidence which were open for submissions between 7 June and 16 August 2024:
a short survey for people who wished to express general views about the Bill as a whole; and
a detailed call for evidence for people, groups, bodies or organisations who wished to comment on specific aspects of the Bill.
The Committee received 13,821 responses to the short survey. Individual responses to this survey were not published. Instead, the Scottish Parliament Information Centre (SPICe) produced a summary analysis of these responses which was published on the Committee's webpage.
The Committee received 7,236 responses to the detailed call for evidence, which were published on Citizen Space. The Scottish Parliament Information Centre (SPICe) also produced a separate summary analysis of these responses.1
On 30 September 2024, the Committee received a letter from the Cabinet Secretary for Health and Social Care including a memorandum setting out the Scottish Government's position on the Bill.2 The letter concludes by stating the Scottish Government's intention to maintain a neutral position on the Bill at this stage while also concluding that "In the Scottish Government’s view, the Bill in its current form is outside the legislative competence of the Scottish Parliament."
The Committee took formal oral evidence on the Bill during November 2024 and in January and early February 2025 (see further Annex A):
On 5 November, the Committee held a private session with representatives of the Non-Government Bills Unit. This was followed by a public evidence session with witnesses in Australia about experiences of implementing assisted dying in that jurisdiction.
On 11 November, the Committee took evidence from witnesses in Canada on experiences of implementing assisted dying in that jurisdiction.
On 12 November, the Committee took evidence from two panels of witnesses, the first comprising legal and human rights experts and the second focusing on mental health considerations related to the Bill.
On 19 November, the Committee took evidence from two further panels of witnesses, the first comprising representatives of healthcare professionals, the second comprising representatives of providers of palliative care.
On 14 January 2025, the Committee took evidence took evidence from two panels of witnesses representing people with long-term conditions and people with disabilities respectively.
On 21 January 2025, the Committee took evidence from two panels of witnesses representing campaign organisations respectively supportive of, and opposed to, the Bill.
On 28 January 2025, the Committee took evidence from the Crown Office and Procurator Fiscal Service and then from the Cabinet Secretary for Health and Social Care (Neil Gray) and supporting officials.
The Committee concluded its oral evidence programme on 4 February 2025 by taking evidence from the Member in Charge of the Bill, Liam McArthur MSP, his adviser and accompanying Scottish Parliament officials.
On 7 January 2025, members of the Committee undertook informal engagement with members of the Scottish Assembly, an organisation that brings together people with a learning disability and autistic people across Scotland and helps them to engage with the political process and a range of support and services. An anonymised note of this informal engagement has been published on the Scottish Parliament website.
To better understand the experiences of individuals living with a terminal illness, the Committee engaged with a number of organisations involved in the provision of frontline care and support to explore options for those that may wish to contribute additional testimony to the Committee’s scrutiny of the Bill. As a result of this further engagement, the Committee received two written testimonies which were published on the Committee website and which members reflected on in public at the Committee's meeting on Tuesday 25 March 2025.
The Committee wishes to thank everyone who contributed evidence to its Stage 1 consideration of the general principles of the Bill.
Consideration by other committees
The Finance and Public Administration Committee issued a call for views on the estimated financial implications of the Bill as set out in its accompanying Financial Memorandum.1 This was open for submissions between 10 June and 16 August 2024 and received 22 responses. On 28 January 2025, the Finance and Public Administration Committee wrote to this Committee setting out the outcome of its scrutiny of the Financial Memorandum:
Our scrutiny of this FM has highlighted potential gaps in the information provided, including underestimates of the direct financial impact as well as of potential wider societal changes. We also found a lack of information on estimated savings that could arise from the Bill. This has led the Committee to conclude that the FM as introduced is not sufficiently comprehensive.
The Delegated Powers and Law Reform (DPLR) Committee considered the Bill at its meetings on 28 May 2024 and 10 September 2024. It published a report on the Bill on 20 September 2024 in which it set out a series of recommendations in relation to the ten powers to make subordinate legislation conferred on Scottish Ministers by the Bill.
Specifically, in relation to the regulation-making powers conferred by section 4(5)(a) (specification of qualifications and experience of the "coordinating registered medical practitioner") and section 6(6)(a) (specification of the qualifications and experience of the "independent registered medical practitioner"), the DPLR Committee recommended that the Bill be amended at Stage 2 to include a statutory requirement for Ministers to consult the Chief Medical Officer for Scotland and the General Medical Council. With respect to the power conferred by section 15(8) (specification of "approved substance"), the DPLR Committee recommended that the Bill be amended at Stage 2 to include a statutory requirement for Ministers to consult the Chief Medical Officer for Scotland.
Views for and against assisted dying
The debate on assisted dying is underpinned by core philosophical concepts such as autonomy, suffering, dignity, and the sanctity of life. Often these concepts are valued by both supporters and those opposed to assisted dying, but the importance placed on each may differ.
The Committee undertook two calls for views, both of which asked people to rank the three most important considerations which influence their opinion on assisted dying. Respondents were offered the same list of options whatever their stated views on the Bill:
Reducing suffering;
Personal dignity;
Personal autonomy;
Risk of coercion of vulnerable people;
Sanctity of life;
Impact on healthcare professionals and the doctor/patient relationship;
Risk of devaluing lives of vulnerable groups;
Risk of eligibility being broadened and safeguards reduced over time; and
Other – please provide further details in the text box.
The combined ranking showed a noticeable difference between those who support assisted dying and those who oppose it in the level of importance allocated to each of the options.
As summarised in figure 1 (below), the most important factors for those expressing support for assisted dying were:
reducing suffering;
personal dignity; and
personal autonomy.
Those who expressed opposition to assisted dying were most concerned about:
the risk of coercion of vulnerable people;
the sanctity of life; and
devaluing the lives of certain groups.
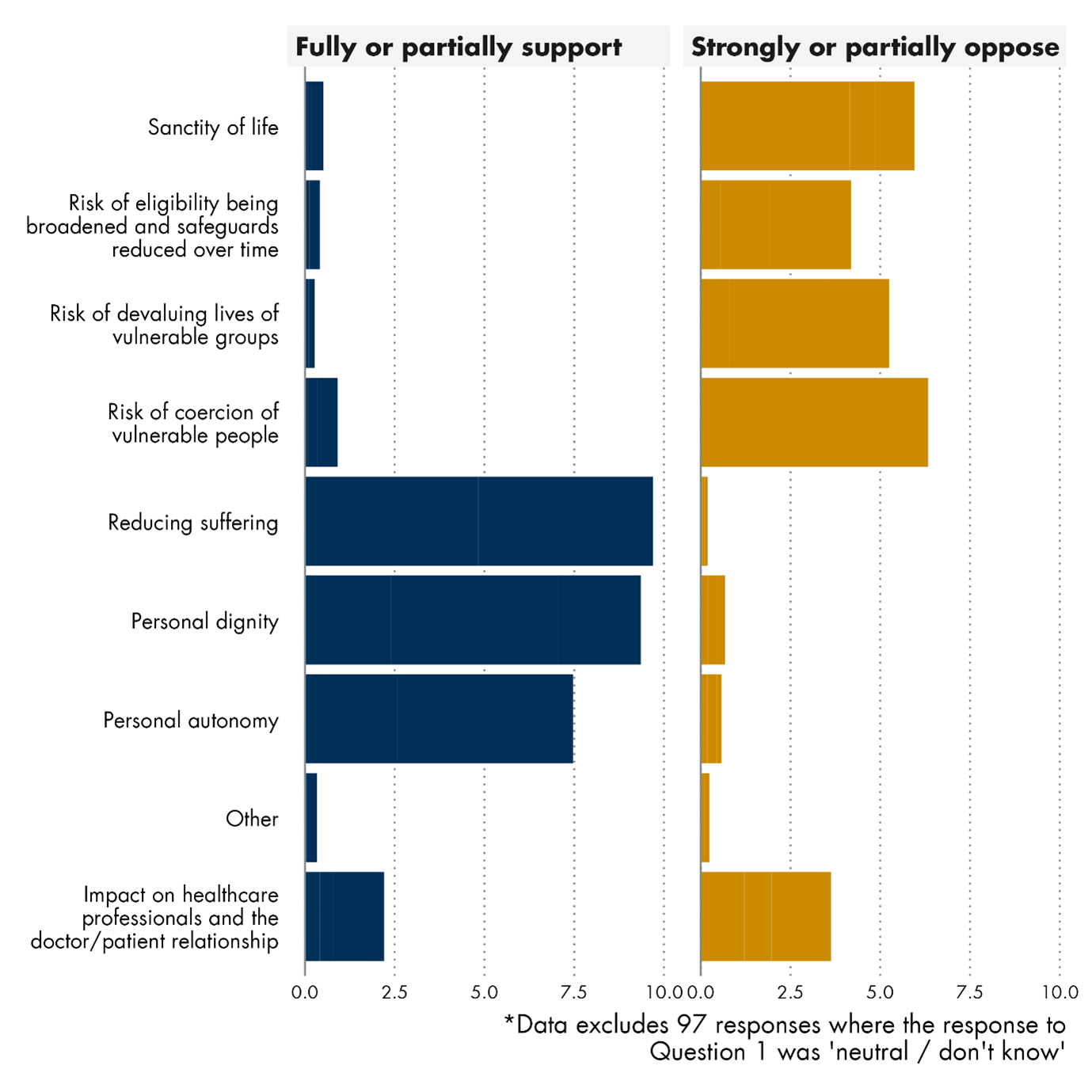
These themes featured heavily in the written and oral evidence and are explored in more detail in the following sections.
Suffering
In evidence submitted to the Committee, the relief of suffering was one of the key considerations of those in support of the Bill. However, it also featured heavily in the detailed responses of people opposed.
For some, palliative care was seen as the natural way to ease suffering. However, others believed palliative care could not relieve the suffering of everyone and was limited in how it can address forms of suffering beyond physical pain. This argument was often supported in written evidence by personal accounts of having watched a loved one die.
Some also argued that, in and of itself, having the option of an assisted death has a therapeutic value in helping to alleviate suffering by giving greater choice and control at end of life, pointing to an increasing proportion of people in places like Oregon, who are approved for an assisted death but ultimately do not make use of the option.
However, some opposed to the Bill did not accept the suggestion that some suffering cannot be alleviated and emphasised the importance of palliative care. Dr Gillian Wright from Our Duty of Care argued:
We can always do something. We have heard many distressing stories, and we absolutely need to respond to them, but there is much more that we could be doing as a community.
...I am aware that there are many failures of care but it is not a case of asking people to thole it, as you might be implying. There is so much that we can do that is not being done.1
The issue of palliative care is discussed in more detail later in this report.
Dignity
A substantial proportion of those supporting the Bill argued that many people at the end of their lives experience a loss of dignity and a level of dependence that is unacceptable to them. These submissions generally argued that it is inhumane to force a person to suffer when their wish is to die. Many drew upon personal experiences of having witnessed a loved one die.
Those opposed to the Bill also spoke of dignity, insisting that this does not diminish because a person is ill or requires assistance from others. These responses argued that a person's sense of dignity is shaped by societal attitudes and norms and that assisted dying would fundamentally change these norms in a way that would reinforce any perceived loss of dignity.
Autonomy
The ‘right to autonomy’ was cited in arguments from both those supporting and opposing the Bill.
Supporters of the Bill argued that individuals have the right to determine the value and quality of their own lives and to make end-of-life decisions based on that judgement. These arguments were often cited alongside the importance of 'choice' and a belief that individuals should have the right to choose the timing and manner of their death. This was reiterated in oral evidence. For example, Alyson Thomson from Dignity in Dying Scotland told the Committee:
The bill does not give people a choice between living or dying; that choice has already been taken away. The bill gives a choice between two kinds of death.1
In contrast, opponents of the Bill argued that autonomy is not absolute and that, in certain circumstances, it is the role of legislation to restrict individual autonomy for the wider benefit of society. Some respondents argued that respecting individual autonomy ignores the interconnected nature of society and the impact such a decision can have on others. In its written submission, the Scottish Council on Human Bioethics argued that, in supporting individual autonomy, the Bill should be carefully assessed for any unintended consequences it may have for society as a whole:
...in an interactive society, making a choice about the value of a life (even one’s own) means making a decision about the value of other lives.2
Devaluing the lives of certain groups
Some of those opposed to the Bill also took the view that legalising assisted dying would send a message that certain individuals’ lives are less valuable than others and that these individuals are considered to be a burden on society. This was considered by these contributors to be a particular risk for people with disabilities and for older people.
In oral evidence, representatives of disability organisations described their fears that the scope of the Bill would quickly be expanded to include those with disabilities within the eligibility criteria for assisted dying. On the back of this, these witnesses expressed concerns that assisted dying would then be presented to them as a viable alternative to support for living. Tressa Burke from Glasgow Disability Alliance told the Committee:
...we take a very clear stand against assisted dying. We simply believe that it will creep and that disabled people will be at the thin end of the wedge.1
Arguments around the potential expansion of eligibility criteria are addressed in more detail in the 'Slippery slope' section.
At the same time, some questioned the extent to which opposition to assisted dying was as widely shared amongst disabled people as was implied by the representatives of disability organisations who gave oral evidence to the Committee. Alyson Thomson from Dignity in Dying Scotland told the Committee:
We know, from our own polling, that the majority of disabled people support a terminal illness assisted dying law. We speak to many people who are disabled and take a different view. I have a letter from a group of prominent disabled activists, which I believe has been circulated to Parliament. In the letter, they say: “We do not wish disabled people to be cited as a homogenous group in efforts to deny dying people choice.”
In a similar vein, some contributors questioned how comfortably the legalisation of assisted dying could sit alongside an effective suicide prevention strategy and work undertaken in Scotland to date to reduce levels of unassisted suicide. These contributors felt that the Bill was at odds with this work and that legalising assisted dying would effectively mean that the state was sanctioning the idea that some lives are not worth living.
In response to these criticisms, Liam McArthur stressed that, under the terms of the Bill, only those with a terminal illness would be deemed eligible for assisted dying. He further highlighted a statement made by a number of Australian organisations which outlined what they considered to be the critical difference between suicide and assisted dying:
Suicide is when a person tragically and intentionally ends their own life...
Voluntary assisted dying is not a choice between life and death. It is an end-of-life choice available to eligible terminally ill people who are already dying. It offers an element of control and comfort over how they die when death becomes inevitable and imminent...
Both suicide prevention and voluntary assisted dying are as important as they are distinct. Confusing these terms can delay access to suicide prevention services for people in distress, and complicate care for those who are at end of life.2
Risk of coercion
Many respondents to the calls for views argued that no law could ever truly safeguard against coercion and the only effective way to protect people from coercion was not to legalise assisted dying in the first place.1
This issue was also explored in more detail during oral evidence. Julian Gardner from the Voluntary Assisted Dying Review Board in Victoria, Australia, told the Committee that, while he had seen no evidence of people being coerced into assisted dying in that jurisdiction, he had seen evidence of the opposite.2
The only reports that we have had have been the reverse, in that people have experienced coercion—that might be too strong a word—or undue influence not to go ahead with ending their life, generally from relatives who have objections or from faith-based institutions.2
However, during an evidence session with witnesses in Canada, Dr Ramona Coelho gave an opposing view on the potential risk of coercion, arguing that, in her view, coercion to undergo medical assistance in dying in Canada would manifest itself in more subtle ways:
If you look at the Health Canada reports, you will see that fear of being a burden and loneliness are high up among the top five reasons for people choosing MAID. [Medical assistance in dying]4
This same concern was also raised in written evidence and characterised by some respondents as constituting a form of ‘internalised’ coercion.1 This issue is addressed in more detail later in this report (see Coercion).
'Slippery slope'
Many submissions from those opposed to assisted dying contended that the passing of the Bill would be the start of a 'slippery slope'. This contention was underpinned by two principal arguments:
That the law tends to expand eligibility or reduce safeguards over time.
That the number of people having an assisted death inevitably rises over time.
Expanding eligibility criteria / reduced safeguards
Those arguing there would be a high likelihood of eligibility criteria expanding over time tended to make reference to experience in Canada, the Netherlands and Belgium, where it was claimed that eligibility criteria had been widened and safeguards had been progressively relaxed or removed since the legislation in those jurisdictions entered into force.
Conversely, those who supported the Bill tended to highlight other jurisdictions where they claimed eligibility criteria and safeguards had not changed since assisted dying legislation entered into force. For these contributors, Oregon was the most commonly cited example, where contributors argued that the legislation had remained largely unchanged since its introduction in 1997.
The Committee also heard evidence, including from legal and human rights stakeholders, that expansion of eligibility criteria under assisted dying laws was more likely to have taken place in jurisdictions that had amended their constitutions or criminal codes to give effect to legalised assisted dying as a result of court rulings, as opposed to jurisdictions which had passed statute to legalise assisted dying, in the absence of such constitutional pressure. By contrast, it was contended that, due to the constitutional set-up in this country, any such changes in Scotland would have to take place through updated legislation that was subject to Parliamentary scrutiny, meaning that such changes could not be achieved through constitutional challenge and were therefore not inevitable (See The risks of a legal challenge extending the eligibility criteria in the Bill).
Liam McArthur argued:
The Canadian model, which is often cited, has evolved through court process, which is sometimes brought into the debate here as something of a risk, but the constitutional arrangements in Canada are very different from those in Scotland and in the UK. The legislation was introduced as a result of a case that was brought before the supreme court in Canada on the basis that the ban on assisted dying was unconstitutional. The Parliament then introduced legislation, which was not felt to go far enough, so it was then legally challenged on appeal, which was upheld, and the scope of the legislation was expanded.1
However, Dr Mary Neal from the University of Strathclyde argued that the Bill contained many areas that were subject to potential ‘slippage’ and that, irrespective of how tightly the law was felt to have been drafted, there was ultimately no way of preventing people from challenging it.2
Liam McArthur contended that, in jurisdictions where eligibility is based on terminal illness and mental capacity, there was no evidence of those criteria having been subsequently expanded. He also highlighted this as one of the key findings of the House of Commons Health and Social Care Committee inquiry into assisted dying.3
Increasing numbers over time
Evidence submitted to the Committee suggested that, in jurisdictions that had legalised assisted dying, there was a general tendency for the number of assisted deaths as a proportion of overall deaths to increase over time. However, many argued that this tendency was an inevitable result of increased awareness of assisted dying as an option following legalisation, while some contended that such an increase should not necessarily be considered a bad thing. Dr Stefanie Green from the Canadian Association of MAiD Assessors and Providers told the Committee:
I am also compelled to point out that actual numbers are irrelevant, of course, because there is a value judgment being added here. Let us say that we believe that heart attacks are bad. If the rate of heart attacks is increasing, we should be worried about that and try to do something to bring it down, but that is because we have made a somewhat non-controversial value judgment that heart attacks are bad. If you think that assisted dying is bad, there is no good number.4
Fraser Sutherland from the Humanist Society Scotland was in agreement with Dr Green's assessment and concluded:
There is an idea that more people accessing the right to assisted dying is evidence of a slippery slope but, if the eligibility criteria have stayed the same, it is only an issue if you inherently have a moral and ethical problem with the principle in the first place.5
The Committee acknowledges all of the evidence it has received during its scrutiny of this Bill at Stage 1 and the strongly held convictions and good intentions of contributors from all sides of the debate on assisted dying. At the same time, the Committee considers that many of the arguments on the fundamental question of whether assisted dying should or should not be legalised are philosophical in nature. It will be a matter for individual members, in deciding how they wish to vote on the general principles of the Bill, to take these into account and to determine what prioritisation and weight they wish to give them.
On the debate around the potential risks of a 'slippery slope' towards a broadening of eligibility criteria and a relaxation or removal of safeguards over time, the Committee notes the very different ways in which legalisation of assisted dying has come about in different jurisdictions around the world. Should the Bill progress to Stage 2, the Committee believes there could be merit in exploring what suitable mechanisms, if any, might be necessary or desirable to address these potential risks in the specific legal and constitutional context in which the Bill would become law.
The Committee notes evidence from other jurisdictions that there has been a general tendency towards the number of people requesting assisted dying increasing over time following legalisation. Some have argued that such trends are a cause for concern while others take the view that such a trend should not, in and of itself, be considered concerning. Should the Bill progress to become law, the Committee considers it important for such trends to be monitored in conjunction with other factors including the availability of palliative care and social care.
Palliative care
The Committee received substantial evidence on the importance of palliative care as part of the debate on assisted dying. For those in favour of assisted dying, there was a belief that, for some people, no amount of palliative care would alleviate suffering. These contributors tended to view palliative care as complementary to assisted dying.1
Conversely, those opposed to assisted dying expressed concerns on two fronts:
That inadequate palliative care will act as a driver of requests for assisted dying; and
That assisted dying will erode the quality and availability of palliative care.
Palliative care as a driver of assisted dying
The Committee heard concerns that current inadequacies in palliative care provision may lead people to consider assisted dying to be their best or only option. The Committee heard evidence of current shortcomings in services which some contributors argued needed to be addressed before the prospect of legalising assisted dying should be considered.
Contributors on both sides of the debate called for greater resourcing of palliative care and shortcomings in availability of palliative care were highlighted repeatedly in evidence. For example, in her written submission, Rachel Kemp told the Committee: “… there are more MSPs than palliative care consultants in Scotland.”2
Sarah Mills from the University of St Andrews told the Committee that palliative care services have become increasingly stretched since the COVID-19 pandemic and suggested they were unable to keep up with demand:
When everything works—when the planets align and we can provide the services to the patients—palliative care is excellent, but the services are not adequate to meet the need.3
Others argued that, irrespective of whether or not the current Bill were to become law, providing good quality palliative care to all who need it would remain a key challenge. In this context, they suggested that assisted dying and palliative care should not be viewed as being in opposition to one another. Rami Okasha from Children's Hospices Across Scotland said:
There are important questions about access, equity of funding, and ensuring that the appropriate palliative care services are there. Even if this bill were not to proceed and parliamentarians were not to support it, the need for palliative care would remain; and, even if parliamentarians do support it and it becomes law, there would be many people who may wish to access assisted dying, but for whom palliative care would be necessary and would provide significant relief and support for many, many years prior to death.3
Some witnesses who were supportive of the Bill also highlighted evidence that, in jurisdictions where assisted dying had been legalised, a high proportion of those seeking an assisted death were already in receipt of palliative care and that the number of people engaging with palliative care services had increased since assisted dying was legalised.
In his evidence to the Committee, Liam McArthur emphasised his expectation that all care and treatment options, including palliative care, would be discussed with individuals requesting access to assisted dying, to enable them to make a properly informed decision:
One of the safeguards that is built into the process is the discussion that needs to take place between the co-ordinating physician and the patient to ensure that the patient is aware of all the options that are available—palliative care, social care or other types of health and care treatments—so that the decision is informed.5
Effect of assisted dying on palliative care
Some palliative care and hospice professionals who responded to the call for views expressed concerns that the Bill could undermine their work and divert resources from the services they provide.1 These concerns were also explored when the Committee took evidence from witnesses on experiences of assisted dying in Canada.
During this session, Dr Ramona Coelho told the Committee:
...in the words of the [Canadian Society of Palliative Medicine], we are seeing “the diversion of limited palliative care resources to support [medical assistance in dying], and the potential for patients refusing palliative care services for fear it will hasten their death.”7
This viewpoint was disputed by Dr Stefanie Green from the Canadian Association of MAiD Assessors and Providers who pointed to an increase in funding for palliative care services that had been provided by the Canadian Government since assisted dying was legalised:
One simply cannot say that resources have been diverted from palliative care to MAID. In fact, as in every other legal jurisdiction in the world where we see assisted dying provision, the funding and levels of palliative care have increased since that became legal.7
Alyson Thomson from Dignity in Dying Scotland echoed this view and pointed to similar evidence from a number of jurisdictions while also highlighting the additional benefits legalisation of assisted dying could have in improving end-of-life care practices more broadly:
I mentioned the Westminster Health and Social Care Committee inquiry. Another of its findings was that, in jurisdictions that have legalised assisted dying, end-of-life and palliative care can improve. The inquiry can point to a number of jurisdictions where massive investments in palliative care were made at the same time as assisted dying was introduced. A whole host of other end-of-life practices improve as well, as conversations about death and dying and the culture around those things open up, as people have more open and transparent conversations and as more doctors are trained in supporting people at end of life.9
Throughout its scrutiny of the Bill at Stage 1, the Committee has heard compelling evidence of the overarching importance, irrespective of whether or not the Bill becomes law, of ensuring that everyone who needs to is able to access good quality palliative care at the end of their lives. The Committee hopes that, regardless of the outcome, the current debate on assisted dying will provide a catalyst for further attention to be given towards improving the quality and availability of palliative care services in Scotland.
Should the Bill progress beyond Stage 1, the Committee highlights to the Scottish Government the importance of giving ongoing careful consideration to how the Bill, if it becomes law, will interact with all other key aspects of end-of-life care provision, including palliative care.
Legal and human rights considerations
Assisted dying and human rights - legal context
Both the courts in the UK and the European Court of Human Rights have recognised that the right to decide when and how to die is an aspect of the right to respect for private and family life under Article 8 of the European Convention on Human Rights (ECHR). However, states have wide discretion in relation to how they set the law in this area. This is sometimes referred to as a wide “margin of appreciation”.
There is also a recognised need to ensure protection for vulnerable groups. No country has yet been found in breach of the ECHR on the basis of not providing access to assisted dying.
The law relating to accessing assisted dying has been challenged on human rights grounds on several occasions in England and Wales. In a recent challenge – of R (Nicklinson and another) v Ministry of Justice ([2014] UKSC 38) – a majority of judges declined to declare the law in England and Wales incompatible with Article 8 of the ECHR. Out of a panel of nine justices, two would have made a declaration of incompatibility; three thought the UK Parliament should be given the opportunity to change the law first; and a further four thought that the issue was for Parliament rather than the courts to decide.
Several respondents to the Committee’s call for views addressed the human rights implications of assisted dying. They noted that legislating for assisted dying engages several of the rights set out in the ECHR:
Article 2 – the right to life – the courts have held that the right to life does not include a right to access an assisted death. However, it does include a duty on the state to adequately investigate deaths to ensure the state’s obligations under Article 2 are being met. Where a state has introduced assisted dying, it would also include a requirement for safeguards for vulnerable people.
Article 8 – the right to respect for private life – court decisions have found that this does include a right to choose when and how to die. However, states have wide discretion in the control of this right for the protection of others.
Article 14 – prohibition of discrimination – there must be no discrimination on any grounds in relation to exercising the rights protected by the ECHR.
Eleanor Deeming from the Scottish Human Rights Commission described the human rights context for the Bill as follows:
If legislation is adopted, the key point is that, to be compliant from a human rights perspective, the legislation must have in place appropriate and sufficient safeguards, particularly to ensure free and informed consent of anyone accessing assisted dying. It is especially important to consider the rights of particular groups of people, such as disabled people, in the debate on whether to adopt legislation.1
The risks of a legal challenge extending the eligibility criteria in the Bill
A key concern for many people and bodies who oppose the Bill is that the eligibility criteria for assisted dying will be expanded over time and potentially without parliamentary scrutiny. This 'slippery slope' argument is discussed in more detail in the section above on Views for and against assisted dying.
Under the terms of the Scotland Act 1998, provisions in Acts of the Scottish Parliament can be struck down on the basis that they are outwith the legislative competence of the Scottish Parliament. One of the grounds for doing so is that a provision is not compliant with the rights set out in the ECHR.
Dr Mary Neal from the University of Strathclyde specifically addressed the potential for the Bill to be subject to human rights challenges in her oral evidence to the Committee. She discussed two lines of argument raised in the context of the Terminally Ill Adults (End of Life) Bill being considered by the UK Parliament:
Under article 14... the argument is that, once assisted dying is allowed within a jurisdiction, questions begin to arise about discrimination and about whether the rules for eligibility will discriminate against some groups who are not eligible. Once you start to allow it for some people, the question that arises is whether human rights require that you allow it for others, too.1
In reference to Article 2 of the ECHR, Dr Neal added:
Under article 2, an argument is being aired to the effect that, although the article does not preclude assisted dying, it might preclude a state providing assisted dying. Obviously, that is as much of an issue in Scotland as it is in England and Wales, because the national health service would be involved in both cases.1
However, other witnesses were less concerned about the potential for the Bill to be subject to human rights challenges. Eleanor Deeming from the Scottish Human Rights Commission argued that decisions of the European Court of Human Rights give states wide discretion in dealing with such cases:
As recently as last year, in the case of Karsai against Hungary, you again see the court at Strasbourg level [the European Court of Human Rights] re-emphasising that this is an area where states are afforded a wide margin of appreciation. That is not to say that it would never intervene under article 2 were it needed to ensure that stringent safeguards were in place to support the right to life, but it was clear that, from the perspective of article 8, the margin extends not just to the decision to intervene or legislate in this area, but, once an intervention has been made, to the detailed rules that are laid down to achieve a balance between different interests.1
Lynda Towers from the Law Society of Scotland agreed with this assessment and added:
…it is worth remembering that the Supreme Court in this country has also indicated that it is pretty unwilling to become involved in cases that are perhaps more to do with social rather than regulatory aspects.1
However, Dr Gordon Macdonald from Care Not Killing challenged the view that the UK courts would continue to take a relaxed attitude in this area:
The fact that, up until now, the courts have said that this is a matter for the Parliament does not mean that they will make the same judgment in future. Once the Parliament has accepted the principle, the question before the courts would not be whether it should be legalised, but whether the law is being implemented fairly and whether there are any discrimination issues.5
The Committee acknowledges that, should it become law, there may be a risk of the Bill being subject to human rights or other court challenges and that this could result in eligibility for assisted dying being extended over time. The Committee further recognises that one's view of the likelihood and seriousness of this risk is likely to vary according to one's overall view of the Bill. The Committee notes that this will be one of a range of factors for individual members to consider in deciding how they wish to vote on the general principles of the Bill.
Views on whether the Bill sufficiently protects vulnerable groups
The Committee received evidence from groups representing people with long-term health conditions as well as from groups representing disabled people. Witnesses from these groups were asked whether, in their view, the Bill provides sufficient protections for vulnerable groups, as required under Article 2 of the ECHR.
Some witnesses expressed a view that the issue was nuanced, reflecting a difficult balance between supporting autonomy and protecting potentially vulnerable people. Vicki Cahill from Alzheimer Scotland said:
The decision to either include people with dementia or exclude them from accessing the bill’s provisions will have significant implications for their human rights, regardless of which way we go and the direction of travel on that. For example, excluding people with dementia from accessing provisions for an assisted death could be seen as an erosion of their rights. However, there also has to be a balance between protecting those human rights and the need for protection and safeguarding, because people with dementia are a particularly vulnerable group and we need to ensure that no harm is done.1
However, those witnesses representing disabled people’s organisations who gave oral evidence to the Committee were strongly of the view that the provisions in the Bill as introduced represented a direct threat to disabled people’s rights. A key concern for these witnesses was the context in which a disabled person might reach a decision to request assisted dying, in light of the structural inequalities disabled people currently face.
Lyn Pornaro from Disability Equality Scotland described the nature of these structural inequalities:
Some disabled people have a fight on their hands from the moment that they are born. They have to fight to get the support that they need, to be heard, to be listened to, to be valued and, sometimes, to be educated. They have to fight to live life and have opportunities in the same way as non-disabled people do—they have to fight for fairness. They are neglected, and they have their human rights taken away from them.1
Marianne Scobie from Glasgow Centre for Inclusive Living went on to describe the impact disabled people experienced as a result of having their lives devalued by society:
Our lives as disabled people are portrayed as tragic and worthless all the time on television, in literature and in the media, and many people start to internalise those feelings and think that they would be better off dead if they cannot walk, talk, feed themselves or go to the toilet.1
Giving evidence to the Committee, Dr Miro Griffiths from Not Dead Yet UK set out how the Bill, in his view, was incompatible with Article 2 of the ECHR and failed to provide the appropriate protections for vulnerable people required by that article in the context of legalising assisted dying:
My view, as someone who is most interested in the implications that the bill has for disabled people’s communities, is that the state has a role and a responsibility to protect disabled people, particularly because of the systemic inequalities that are faced by disabled people’s communities across the country. The state therefore has a role in protecting all life associated with disabled people’s communities. I think that what you are proposing is incompatible not only with disability rights, but with the principle that the state is there to protect disabled people.4
However, this view was challenged by supporters of the Bill. Alyson Thomson from Dignity in Dying Scotland recognised the structural inequalities disabled people face and the urgent need for these to be addressed but argued that this was a separate debate to the one concerning assisted dying:
I can completely understand why we need to make urgent progress on all those fronts, but we do not do that by banning choice for dying people. All that that does is exacerbate the suffering for a group of people who are dying. The bill does not give people a choice between living or dying; that choice has already been taken away. The bill gives a choice between two kinds of death.4
Meanwhile, while similarly recognising the structural inequalities disabled people face and the urgent need for these to be tackled, Liam McArthur told the Committee that anyone who feared that disabled people might be forced into a situation of requesting assisted dying should be reassured that, according to the eligibility criteria set out in the Bill, “...having a disability alone does not make you eligible to access an assisted death—you need an advanced, progressive, terminal illness and mental capacity to be able to do so."6
The Committee notes the compelling evidence it has heard concerning the significant structural inequalities and barriers to services and support disabled people face every day. It recognises that these and the negative societal attitudes that lead disabled people to feel their lives are devalued need to be urgently and systematically addressed.
The Committee notes the concerns raised by organisations representing disabled people and by others about what they perceive to be the risks to vulnerable groups posed by the Bill. It also notes the views expressed by those who support the Bill in arguing that it provides appropriate protections for vulnerable groups, in accordance with the requirements of Article 2 of the ECHR. The question of whether the Bill strikes an appropriate balance between providing a right for terminally ill adults to access assisted dying and the requirement to protect vulnerable groups will be a matter for further consideration by individual members in deciding how they wish to vote on the general principles of the Bill.
Views on oversight of decisions to protect human rights
During the Committee's Stage 1 scrutiny, stakeholders argued that aspects of the Bill could be improved to strengthen human rights compliance. One suggestion in this regard was that the Bill should include stronger oversight mechanisms in relation to decisions to access assisted dying.
In its response to the Committee’s call for views, Edinburgh Napier University Centre for Mental Health Practice, Policy and Law Research raised concerns that the oversight mechanisms included in the Bill as introduced were weak. To strengthen the Bill, it proposed the development of local multi-disciplinary panels to monitor practice and review individual cases.1
The Law Society of Scotland also highlighted stronger oversight mechanisms as a potential means of strengthening human rights compliance within the Bill:
Given the need for robust legal and institutional safeguards to ensure compliance with Article 2 ECHR..., we note that the Bill doesn’t appear to provide oversight provisions beyond collection and reporting of data. We understand that some countries have review boards and review committees to provide oversight, especially when the death certificate will only record the terminal illness and won’t disclose an assisted death. It may be appropriate for consideration to be given to strengthening oversight measures.2
In oral evidence to the Committee, Eleanor Deeming from the Scottish Human Rights Commission emphasised the importance of introducing review options both at the beginning and the end of the assisted dying process outlined in the Bill. She argued that pre-event reviews, carried out in an independent or judicial capacity, could be seen as “...a robust means of reducing concerns about inappropriate use".3 She went on to explain:
Article 2 requires that there is sufficient subsequent review to ensure that there is effective, independent and prompt investigation of deaths. That is why we have recommended that the Parliament considers including a system of judicial or independent oversight, with both prior and subsequent reviews, to comply with human rights standards. That would provide a much higher degree of scrutiny and stronger safeguards around the right to life.3
Other respondents to the call for views raised what is sometimes referred to as a 'civic model' for assisted dying. Under this model, decision-making in relation to assisted dying would sit with the courts rather than with health professionals (although health professionals would still have a role in carrying out assessments). The Terminally Ill Adults (End of Life) Bill currently before the UK Parliament would, as originally drafted, require every application for assisted dying to be considered by the High Court for England and Wales.
During his evidence to the Committee, Liam McArthur was asked whether he had considered a role for court oversight in the assisted dying process. He responded:
I did, because I was aware that it had been an aspect of earlier bills that had come before the Westminster Parliament. However, I was not necessarily convinced that I could see what additional safeguard it would put in place. The balance is always to ensure that the safeguards do what they are intended to do, and do not simply act as an unnecessary obstacle while not providing any protection.5
However, Liam McArthur went on to highlight the role of the Crown Office and Procurator Fiscal Service’s (COPFS) Scottish Fatalities Investigation Unit in investigating all deaths in Scotland which are sudden, suspicious or unexplained. He concluded:
That may offer the sort of reassurance that the public might have expected court oversight to provide.6
The Committee took evidence from representatives of COPFS during its meeting on 28 January 2025. Andy Shanks, Head of the Scottish Fatalities Investigation Unit, outlined the role the Unit would ordinarily fulfil with respect to the investigation of fatalities:
Deaths are already investigated independently by the COPFS on behalf of the Lord Advocate, which would bring that degree of independent scrutiny to the circumstances of the death. That is not only done in relation to the potential for criminality but, beyond that, in terms of wider death investigation purposes, it is done to see whether there are systemic issues or issues of public concern that require further investigation— or, indeed, whether it is in the public interest to hold a fatal accident inquiry. Therefore, I think that independent scrutiny would already exist.7
The representatives of COPFS who gave evidence to the Committee confirmed that medical practitioners are already provided with guidance on those deaths that are required to be reported to the COPFS. Andy Shanks concluded:
Ultimately, it is a matter for the Lord Advocate whether that guidance would be changed: I cannot commit to a position on her behalf today. However, were the provisions to come into force, it is likely that deaths using the assisted dying process would require to be reported to the procurator fiscal as a mandatory category of reportable death.7
At the same time, witnesses representing COPFS indicated that, in the event of the Bill becoming law, they would normally expect their involvement in investigating cases of assisted dying to be relatively short and unlikely to uncover any concerns. Andy Shanks went on to argue that, even in circumstances where a process was considered not to have been lawful, this may not automatically mean that a criminal offence had been committed.7
The Committee notes evidence from those contributors to its scrutiny of the Bill who have argued that the safeguards in the Bill, and its compliance with human rights requirements, could be strengthened by the introduction of an independent oversight mechanism. It also notes evidence from COPFS regarding the role it would expect to play in investigating cases of assisted dying if the Bill were to become law. Should the Bill progress beyond Stage 1, the Committee would welcome the opportunity to consider amendments to provide for independent oversight within the Bill at Stage 2. Options include the creation of an independent review panel at a local or national level or a potential role for the Chief Medical Officer in monitoring the Bill's implementation, as has been provided for in the Terminally Ill Adults (End of Life) Bill, currently under consideration in the UK Parliament.
Views on options for challenging decisions made by doctors
During the Committee's Stage 1 scrutiny, several stakeholders have noted that the Bill as introduced provides no mechanisms for the decisions made by doctors as part of the process outlined in the Bill to be challenged, be that in a court or via another independent forum. According to the Bill as introduced, doctors would be responsible for assessing:
whether someone met the requirements of having a terminal illness as defined in the Bill;
whether someone had capacity to make a decision to access assisted dying at each stage of the process; and
whether someone had been coerced into reaching a decision to access assisted dying.
In its written response to the Committee, Edinburgh Napier University Centre for Mental Health Practice, Policy and Law Research raised the following concerns:
We are concerned at the lack of any accessible mechanism by which the decision of a doctor can be appealed or independently reviewed by the courts. This may raise concerns about compliance with Article 6 of the ECHR and, even if this is not the case, we believe it is a significant gap.1
It went on to draw comparisons with provisions in the Adults with Incapacity (Scotland) Act 2000 which allow “anyone with an interest” to challenge a decision by a doctor in relation to the treatment of an adult with incapacity. However, it also argued that additional safeguards would be necessary if such a process were to be established, to prevent abuse by campaign groups.
The Equality and Human Rights Commission raised similar concerns in its written submission:
The Bill and accompanying documents are unclear on a process for requesting redeterminations in the situation a registered medical practitioner does not agree that the conditions in relation to provision of assistance have been met, or where different medical practitioners do not agree that they’ve been met.2
Liam McArthur discussed his expectations of what would happen in the event that an individual wished to challenge the view of a doctor who had concluded that they did not qualify for assisted dying:
If the patient does not meet those criteria to the satisfaction of both medics, the option to go to another medical practitioner remains open to them...3
However, in terms of introducing a more formal mechanism for reviewing or challenging decisions, Mr McArthur went on to say:
There is the option for an individual to seek a diagnosis, but medical professionals will make these assessments. If the patient does not meet the criteria, it is important for the patient, the medics and public confidence that the law, as it stands, remains extant.3
The Committee notes concerns from certain contributors to its scrutiny that the Bill lacks clear provision for the decisions of medical practitioners, as part of the assisted dying process, to be independently challenged or reviewed. Should the Bill progress beyond Stage 1, the Committee would welcome the opportunity to consider amendments to the Bill that would allow such decisions to be subject to an independent review or appeals process. The Committee notes from evidence that this need not be a formal process, such as via a court, but could equally be fulfilled by a more informal process, such as via an independent review panel, as referenced above. In this context, it further suggests that consideration would need to be given to who would be entitled to access any such review process to ensure it is protected against potential risks of being abused.
Eligibility and capacity
Section 1 of the Bill sets out that an "...eligible terminally ill adult may, on request, be lawfully provided with assistance to end their life" as long as that assistance is provided in accordance with its provisions.1 Section 2 provides a definition of terminal illness for the purposes of the Bill and Section 3 sets out additional eligibility criteria for access to assisted dying.
Definition of terminal illness
Section 2 defines terminal illness, for the purposes of the Bill, as follows:
a person is terminally ill if they have an advanced and progressive disease, illness or condition from which they are unable to recover and that can reasonably be expected to cause their premature death.1
The definition in the Bill follows that set out in the Social Security (Scotland) Act 2018, which was intended to widen access to disability benefits for those living with terminal illnesses. The definition in the 2018 Act does not include a prognostic timescale, as it was determined that for many terminal illnesses, particularly non-cancer conditions like motor neurone disease (MND), chronic heart failure or chronic obstructive pulmonary disease (COPD), accurate prognosis can be difficult because of the unpredictable trajectories of these conditions. This definition moved away from prognostic timescales to allow registered medical practitioners and registered nurses to use their clinical judgement to determine if an individual meets this eligibility criterion, using guidance issued by the Chief Medical Officer.
As a comparison, the definition used by the UK Department of Work and Pensions (DWP) for determining eligibility for disability benefits under terminal illness rules contains a 12 month prognostic timescalei and the Terminally Ill Adults (End of Life) Bill introduced in the House of Commons in November 2024 determines eligibility for access to assisted dying on the basis of a 6 month prognostic timescale.
The Policy Memorandum accompanying the current Bill notes that the definition of terminal illness does not include reference to a period of life expectancy. However, it states that "...the definition requires a person to be in an advanced stage of terminal illness (i.e. close to death)."2
Many respondents to the Committee's calls for evidence on the Bill raised concerns about the breadth of the definition of terminal illness on the basis that there would be potential for the definition to include a wide range of long-term conditions. Some proposed the inclusion of a prognostic timescale, such as 6 or 12 months, as a means of narrowing the definition. Conversely, others have raised concerns that the definition is already too narrow and discriminates against people experiencing other conditions that, although they may not meet the definition of terminal illness, nonetheless bring "unbearable suffering".
When taking evidence from representatives of organisations that provide palliative care and support at the end of life in Scotland, the Committee heard concerns that the definition and language proposed in the Bill could lead to inconsistency of application. Mark Hazelwood from the Scottish Partnership for Palliative Care told the Committee:
...the key terms "advanced and progressive" disease and "premature" mortality are not precise and do not have agreed definitions, so the definition in the bill does not deliver the clearly defined and quite narrow cohort that seems to be the policy intent as set out in the policy memorandum. That will result in variation in interpretation, with the public and practitioners being confused about who might be eligible, and there will be inconsistency.3
During a separate evidence session, Vicki Cahill from Alzheimer Scotland also argued that the terminology used in the definition of terminal illness should be more descriptive, as the current lack of specificity could be problematic:
It is not specific enough or clear enough to make sure that we are not missing out those individuals who either might be able to or who should not be able to access those provisions.4
Witnesses representing medical professions were not in a position to indicate a particular collective view of their members regarding the definition of terminal illness set out in the Bill. However, Dr Chris Provan from the Royal College of General Practitioners Scotland expressed his support for the definition contained in the Bill and for the decision of Liam McArthur not to include a prognostic timescale within that definition:
The definition is not one of the areas that we have significant concerns about, because it appears to cover much of what is relevant and is relatively narrow, without giving a timescale.3
Giving evidence about the experience of introducing assisted dying in Victoria, Australia, Professor Ben White from the Australian Centre for Health Law Research described how the Australian Capital Territory has taken a similar approach to Scotland in explicitly excluding a prognostic timescale from its defined eligibility criteria. He emphasised the importance of considering eligibility criteria in legislation on assisted dying in a holistic way:
We are talking about people who have an advanced progressive illness that has reached the stage of an illness that is going to cause their death; it is a cohort of terminally ill people. Removing the arbitrary nature of whether the timeframe is six months, eight months or 12 months is a significant step forward in the Scottish bill.6
Dr Sarah Mills from the University of St Andrews illustrated how difficult it can be for medical practitioners to predict a patient's prognosis with any degree of certainty and, on this basis, argued that including a prognostic timescale within the definition of terminal illness in the Bill would be unhelpful:
Any doctor who feels that they are able to adequately predict somebody’s prognosis in months and years is usually mistaken. I have seen three people this week who I thought were going to be dead but are not. It is very imprecise. Until we improve on the precision and accuracy with which we can identify somebody’s prognosis, it is meaningless to include a timescale in the bill, because you will find that, with 10 doctors in a room, you will get 10 different opinions.3
Some stakeholders raised concerns about the use of the term 'unable to recover' in the definition. In her evidence to the Committee, Dr Mary Neal argued that 'unrecoverable' is not the same as 'untreatable' and that someone could render their condition unrecoverable by refusing treatment.
In his evidence to the Committee, Liam McArthur set out the intention behind the wording of the definition in the Bill, namely that "...the expectation is that there would be a requirement for the terminal illness to be advanced and progressive, so that the patient would not recover." He went on to argue that, ultimately, determining whether an individual meets this eligibility criterion would be a matter for clinical judgement before concluding: "...medics are used to making that diagnosis and are comfortable with it."8
Mr McArthur further outlined what he considered to be the critical distinction between a condition that is 'untreatable' and one that is 'unrecoverable' and how different conditions might be judged to make an individual eligible for assisted dying or not on that basis:
Defining "terminally ill" on the basis of a "disease, illness or condition" from which the patient will not recover is important. That separates it out from some of the conditions that have been raised in evidence that, to my mind, would not meet the eligibility criteria, because there are options that would lead to a recovery. Whether the patient chooses to take those options is a matter for the individual patient, but such conditions would not meet the eligibility criteria that are set out in the bill.8
The Committee notes from evidence that the definition of terminal illness set out in the Bill largely follows that set out in social security legislation. It further notes concerns from certain stakeholders that, although the definitions are largely the same, the purpose of each piece of legislation is fundamentally different. With these concerns in mind, the Committee concludes that, should the Bill progress beyond Stage 1, the definition may require further clarification via amendment to ensure it is appropriate for its intended purpose.
The Committee has heard a range of evidence on the question of whether the definition of terminal illness should include a prognostic timescale. It acknowledges substantial evidence of how difficult it can be to accurately predict the prognosis of an individual living with a terminal illness. At the same time, the Committee also recognises that not including a life expectancy timescale within the definition of terminal illness means widening eligibility for assisted dying to include individuals who, although living with an illness or condition that is progressive and untreatable, may not be approaching death for a considerable period of time. However, on balance, the Committee recognises the rationale of Liam McArthur for not including a prognostic timescale in the definition of terminal illness set out in the Bill and for arguing that it is ultimately better to leave determination of whether or not an individual meets that specific eligibility criterion to clinical judgement.
Additional eligibility criteria
Section 3 of the Bill sets out that, in addition to being terminally ill, to be determined as eligible for assisted dying, a person must be 16 or over (section 29 defines an "adult" as a person who is aged 16 or over) and must also:
be ordinarily resident in Scotland for at least 12 months before the date on which the first declaration is made;
be registered with a general practitioner/medical practice in Scotland; and
have capacity to understand the issues at hand and be able to make, understand, communicate, and remember the decision made.
Additional eligibility criteria: Age
Contributors to the Committee's scrutiny expressed a range of concerns around the age-related eligibility criterion in the Bill. Arguing that the age threshold for eligibility should be higher than 16, some respondents to the Committee's call for written evidence expressed a view that young people are not mature enough to make a decision to request assisted dying. These respondents based this on a range of arguments, including views that the human brain continues developing until a person is in their mid-20s, and that young people are impulsive and their emotions can fluctuate.
The Policy Memorandum states that the age requirement in the Bill is set at 16 years of age to "...ensure that only those who have reached the age of majority (i.e. have full legal decision-making capacity) in Scots law can access assisted dying."1 The Age of Legal Capacity (Scotland) Act 1991 allows competent under-16-year-olds to make decisions about medical procedures and treatment. This includes giving them the legal ability to refuse treatment.
Witnesses representing groups that support assisted dying were generally supportive of setting the age requirement at age 16. Fraser Sutherland from the Humanist Society Scotland argued:
Sixteen is the age of majority in a number of areas, particularly in healthcare, in which young people have capacity, if they are assessed as such. It is important to respect that2.
In other jurisdictions which limit assisted dying to adults, the Committee has heard evidence that 18 is typically the age at which someone becomes eligible. Julian Gardner AM, representing the Voluntary Assisted Dying Review Board in Victoria, Australia explained the rationale for setting the age-related eligbility criterion at 18 in Australia as being:
Because that is the age at which someone becomes an adult in Australia. It was simply to make the legislation consistent with all other laws relating to adulthood.3
While giving evidence to the Committee, Assistant Chief Constable Steve Johnson from Police Scotland highlighted a discrepancy between the age threshold set out in the Bill and the age of adulthood that is stipulated as being 18 years of age in the UN Convention on the Rights of the Childi. He expressed concern that the differing definitions could lead to ambiguity in how the Bill was legally enforced:
The United Nations Convention on the Rights of the Child is clear and unambiguous that a person is a child until they are 18. However, the bill sets out that a person is considered to be an adult from the age of 16. So—which is it? Which definition would you want me, as a law enforcement officer, to use? Clearly, someone who is 17 is considered to be a child under the convention and would have rights to parental support, but according to the bill a 16-year-old could determine that they want to move forward with a provision that would allow them to seek to end their life. I seek clarity as to whether the bill considers a person to be an adult at 16. If so, that is not consistent with many other pieces of legislation in Scotland.4
Assistant Chief Constable Johnson concluded:
If the Parliament deems that [it] wants assisted dying provisions to be available to children, as they are defined by the UNCRC, there would need to be very clear guidance and guidelines about the roles of parents and of children4.
Rami Okasha from CHAS raised a concern that the age requirement in the Bill "would make Scotland an outlier in relation to legislation of this type." He argued that there are precedents in Scottish public policy for defining a higher threshold for adulthood, on the basis of younger adults' relative vulnerability:
We know that the sentencing guidelines consider young people to be less able to exercise good judgment in relation to really complex decisions, and that there is an acknowledgment that younger adults, particularly those around the ages of 16 to 18, are more susceptible to negative influences, more likely to go into difficult relationships and less likely to think about risk.6
In its written submission, CHAS also argued that the Bill fails to include due consideration of the specific needs of young people (those aged between 16-21 years of age):
We believe that the proposals do not take into account the medical, neurological and psychological differences between an adult at the end of life with a terminal illness, and a young person with a life-shortening condition that may meet the Bill’s definition of ‘terminal illness’ – but who may have years of life left to live.7
The organisation went on to make the case for "...additional tailored safeguards for younger adults up to the age of 25."7 Other respondents to the Committee's call for views also argued for additional safeguards to be included for young people, such as a requirement for them to have to observe a longer period of reflection and to be assessed by a paediatric psychiatrist.
Liam McArthur reflected on the age criterion during his evidence to the Committee and concluded that there were strong, persuasive arguments for the requirement to be set either at 16 or 18 years of age. Mr McArthur further indicated that he was "...keen to reflect further should the bill pass at stage 1 and as we look ahead to stage 2" and acknowledged that further engagement might be beneficial on this particular issue.1
The Committee recognises Liam McArthur's intention, in setting the age-related eligibility criterion for assisted dying at 16, to align with the age of majority as defined in Scots law and the age at which persons are deemed able to make their own decisions about medical procedures and treatment under the Age of Legal Capacity (Scotland) Act 1991. At the same time, the Committee also notes stakeholder concerns that there is a discrepancy between this position and the UN Convention on the Rights of the Child (Incorporation) (Scotland) Act 2024 which stipulates that a person is deemed to become an adult at age 18. The Committee further notes evidence that public bodies are required by the 2024 Act to respect the rights set out in the UN Convention and concerns that this discrepancy could create particular challenges in terms of legal enforcement of the current Bill.
The Committee further notes more specific concerns expressed by Children's Hospices Across Scotland (CHAS) and certain other contributors regarding the need for additional provisions and safeguards within the Bill to address the specific circumstances of young adults aged up to 25.
In this context, the Committee welcomes Mr McArthur's willingness, should the Bill progress beyond Stage 1, to consider this issue further at Stage 2. The Committee is in agreement that, in these circumstances, it would wish to undertake further targeted engagement with CHAS, other relevant stakeholders and young people themselves, prior to that further consideration taking place at Stage 2.
Additional eligibility criteria: Residence
The Bill requires someone to be 'ordinarily resident' in Scotland for 12 months and be registered with a general practitioner/medical practice before they would be eligible for assisted dying. During his appearance before the Committee, Assistant Chief Constable Johnson questioned what was meant by the term 'ordinarily resident' and whether this was sufficiently clear to prevent, for example, people living in other jurisdictions where assisted dying was not legal (or where eligibility criteria were more restrictive) from accessing assisted dying in Scotland. He gave an example to illustrate a situation where this definition could create unhelpful complexity for a police investigation into a potential offence of coercion that would be created by section 21 of the Bill:
That [definition] could increase the burden on us in terms of investigations, and might involve more people outside the jurisdiction. A lack of clarity on that could make the process more challenging and we might have to conduct investigations that would span a person who used the legislation in Scotland when most of their relatives would be in England and Wales.4
Julian Gardner AM confirmed that the same residency requirement exists in legislation on assisted dying in Victoria, Australia, but went on to outline circumstances in which the provision was found, in practice, to have created an unintended barrier to access to assisted dying for certain individuals:
...as you have in your bill, we have a requirement for 12 months’ residence. We have discovered that, as people become close to death, they move back home to be with family. There might well be people who come from south of the border in order to have the support of their family who become ineligible because of the residence requirement, so you might need to have a provision that says that an exemption could be granted in special circumstances.3
Liam McArthur told the Committee that, in his view, the concept of "ordinarily resident" was well established and understood and therefore should not give rise to unintended consequences. He added:
That is another area where I would be happy to reflect on any proposed changes. However, the fact that the “ordinarily resident” requirement sits alongside a requirement for people to be registered with a GP probably gets around the concerns.1
The Committee acknowledges Liam McArthur's argument, in explaining his choice of wording of the residence criterion in the Bill, that the term 'ordinarily resident' is used in a variety of legal contexts, is therefore well established and understood, and should be considered in conjunction with other requirements such as being registered with a GP. At the same time, the Committee welcomes Mr McArthur's willingness to consider this matter further should the Bill progress beyond Stage 1.
Additional eligibility criteria: Capacity
Section 3(2) sets out how a terminally ill adult’s capacity to make the decision to request assistance to end their life should be determined. To be eligible for assisted dying, the person must have the mental capacity to make the request for an assisted death. The Bill describes a person as having capacity if they are not suffering from a mental disorder which might affect the making of the request, and they are capable of the following:
understanding information and advice about making the request;
making a decision to make the request;
communicating the decision;
understanding the decision; and
retaining the memory of the decision.
The Bill requires that capacity be confirmed by the assessing registered medical practitioners, and contains an option to refer to a specialist if this is considered necessary to be able to determine capacity.
The Bill uses criteria from the Adults with Incapacity (Scotland) Act 2000 to define capacity. However, Lynda Towers from the Law Society of Scotland argued that, in her view, capacity was a problematic concept, particularly at a time when there was a degree of ongoing legal uncertainty about its definition. She went on to refer to the Scottish Mental Health Law Review (also known as the “Scott Review”) which reported in 2022 and recommended a complete overhaul of Scotland’s mental health legislation, including those aspects of the legislation governing capacity. The review included a proposal that approaches to determining capacity should be reconsidered, moving from a determination of whether someone has capacity or not towards carrying out a test of autonomous decision-making ability. In light of the findings of the Scott Review, proposed amendments to the Mental Health (Care and Treatment) (Scotland) Act 2003, and an upcoming review of the Adults with Incapacity (Scotland) Act 2000, Lynda Towers concluded:
When you have a piece of legislation, you have to take a view on the definition at that particular time but, if there is to be further thinking about and reviews of those pieces of legislation, and when so many potential changes are going through, this is a very unfortunate time to have to consider what “capacity” means.13
Professor Colin McKay from Napier University had a different view on the timing of this debate in the context of this Bill, surmising that "...for the purposes of trying to make the bill work in the context of the legal framework that we have, the approach is probably your best bet".13 He told the Committee:
...the recommendations of the Scott review are with the Scottish Government, but I do not think that it will make any fundamental change around capacity for several years. For the moment, capacity as a concept is broadly understood by the profession. There are more and less scientific ways of assessing it. With improved training and guidance, I think that it is workable as a test, provided that people are given the right support and a careful enough assessment.13
On the whole, stakeholders were supportive of the requirement in the Bill for a person to be able to demonstrate capacity to be deemed eligible for assisted dying. However, in written submissions to the Committee's call for views, many respondents questioned how this would be assessed and expressed concern that many doctors do not have the required expertise or time to undertake capacity assessments effectively. Often, these submissions called for specialists to be allocated responsibility for undertaking capacity assessments, yet some highlighted that there would also be resource implications associated with this approach. During her evidence to the Committee, Stephanie Fraser from Cerebral Palsy Scotland also argued there would be a need for specialist knowledge to assess capacity of people with certain conditions, such as cerebral palsy. The Scottish Association of Social Work also wrote to the Committee highlighting the specific role of social workers and Mental Health Officers in determining capacity and safeguarding vulnerable adults.16
During oral evidence sessions, certain witnesses argued that assessing capacity should already be a core practice of every medical practitioner. Dr Chris Provan from the Royal College of General Practitioners Scotland told the Committee that GPs are "...used to assessing capacity" before noting that "...it can be complex and difficult".13 He went on to note that "...sometimes, we ask specialist psychiatry services to help us to make a decision."13 When asked if assessing capacity of people seeking an assisted death should be a responsibility that is reserved to psychiatric doctors, Dr Stephen Potts from the Royal College of Psychiatrists in Scotland responded:
Assessing capacity for decisions about medical treatment should be part of the core skills of all doctors in all specialties and should not be reserved to a specialist who is regarded as having additional expertise.13
However, when asked whether the Bill provided sufficient clarity on the definition of capacity and the process for assessing it, Dr Potts responded that, in his view, the language in the Bill required further clarity and that this should include placing additional requirements on medical practitioners in cases where they seek a psychiatrist's assessment of capacity:
The bill provides that, if either of the assessing doctors has doubts about a person’s capacity, they "may" refer to a psychiatrist—that is, they do not have to. The bill also provides that they are required to "take account of" the psychiatrist’s assessment of capacity, but it is not clear what "take account of" means. For example, it could mean that I have heard your opinion and I disagree with it, so we are going ahead... The language within the bill itself should be strengthened, and not left to a future code of practice.13
The Bill states that to be eligible for assisted dying, the person must have the mental capacity to make the request for an assisted death. It describes a person as having capacity if they are not suffering from a mental disorder which might affect the making of the request.ii
During oral evidence, Professor Colin McKay from Napier University argued that the approach to determining capacity in the Bill reverses the typical test of capacity in that, under this Bill, a person has to actively prove they have capacity rather than there being a presumption that they have capacity unless it can be shown otherwise:
...it looks as if, in the drafting of the bill, the test of incapacity in the Adults with Incapacity (Scotland) Act 2000 has been taken and made into a test of capacity.13
Professor McKay raised this reversal of approach particularly in relation to the inclusion of 'mental disorder' in the definition of capacity. He noted that the reversal of the incapacity test could mean that people with a mental illness could be automatically excluded and questioned, on this basis, whether the reference to mental disorder should be removed from the Bill:
The impact of that [reversal] is that, if someone has a mental disorder that might affect the making of their request, you do not even have to think about the second part of the test, on capacity, which is a slightly odd thing. I think that the ethical issue is whether the mental disorder means that the person is not really able to make a genuinely autonomous decision about ending their life, so the focus should be on capacity.13
Some respondents to the Committee's call for views thought the definition of capacity in the Bill could imply that all people with a mental disorder, which could include anyone with a mental illness, learning disability or personality disorder, may be deemed to lack capacity and that this could potentially be viewed as discriminatory.
A number of witnesses giving oral evidence to the Committee took the view that excluding someone from access to assisted dying on this basis would indeed be discriminatory. Eleanor Deeming from the Scottish Human Rights Commission argued that the success or otherwise of any case that was brought on the basis of a failure to comply with Article 12 of the United Nations Convention on the Rights of Persons with Disabilities and specifically the right to equal recognition before the law would depend on the individual circumstances of that case. She told the Committee:
The bill appears to refuse assisted dying to someone on the basis of a diagnosis of mental disorder that is unrelated to the reason why they are seeking assisted dying. We have concerns that that could be discriminatory, unless it can be justified in the individual circumstances. We highlight in our written evidence that one approach would be to offer support to all people who are considering assisted dying, in the form of peer support counselling so that they can consider their decision before embarking on the process.13
Dr Potts illustrated how, from a psychiatric perspective, having a mental disorder as defined in the 2003 Act, could in and of itself be deemed to disqualify an individual from eligibility for assisted dying:
The bill states that the person must not be “suffering from a mental disorder that might affect the making of a request”. Well, any mental disorder might affect the making of a request. The question at issue for the doctors involved is whether the mental disorder does affect the making of the request. We have recommended that, if the bill is passed at stage 1, the wording be amended to reflect that concern.13
Professor Colin McKay suggested that, in his view, a potentially workable solution to this issue could be to remove reference to mental disorder from the Bill entirely:
You could take out the reference to mental disorder altogether and I am not sure that the bill would be any the worse for it, because you would still have the requirement that the person has to be capable of understanding information about making a request, making a decision, communicating and so on. That is a very familiar test of capacity that is already well understood, so I am not sure that the definition of mental disorder has to be in the bill, to be honest.13
Certain contributors to the Committee's scrutiny were concerned about how people with declining or fluctuating capacity would be provided for under the Bill. The Bill requires a person seeking an assisted death to have capacity at every stage of the process, including the point at which they receive the assistance. However, some stakeholders questioned what impact these provisions would have on people with conditions such as Alzheimer's and dementia, which are recognised as life-shortening illnesses that, at a certain point for certain individuals, may meet the definition of terminal illness and therefore make those individuals eligible for access to assisted dying. In her evidence to the Committee, Vicki Cahill from Alzheimer Scotland called for "...flexibility in the legislation to allow those with fluctuating conditions to find opportunities to express themselves".26
During his evidence, Dr Potts offered an illustration of how fluctuating capacity might be dealt with by those charged with assessing the capacity of individuals requesting access to assisted dying:
With regard to your point about fluctuating capacity, that is recognised more in the condition of deliriumiii than in dementia. It tends to come on later in the course of a dementing illness, and it can make it hard for those who are assisting a patient to know what they want if their capacity varies from morning to afternoon, for example. On an issue as important as this, it is important that the capacity is taken at its best, as far as is possible. If you have somebody who regularly loses capacity late in the day, but they retain capacity in the morning, you go with their morning decision as much as you can.13
Some respondents to the Committee's call for views also voiced concern that the Bill makes no provision for 'advance directives'.iv These respondents argued that a failure to recognise these, coupled with the exclusion of a prognostic timescale in the definition of terminal illness could result in people pursuing an assisted death much earlier than they would otherwise wish, for fear of subsequently losing capacity and therefore being deemed as no longer eligible for assisted dying. However, certain witnesses contributing oral evidence argued that permitting the use of advance directives could be problematic.
Vicki Cahill from Alzheimer Scotland argued that permitting the use of advance directives may be counter-productive as their use may not take account of circumstances where, after signing an advance directive, an individual's subsequent experience of living with a condition might cause them to change their mind. She told the Committee:
...if someone is going to create an advance directive, they are more likely to do so early in their diagnosis and may have a preconceived idea of what it is to live with a condition such as dementia. Their actual experience may be different, particularly if they have access to high-quality health and social care—the kind of care and support that enables people to live well with dementia.26
Professor Colin McKay argued that allowing the use of advance directives in the context of this Bill could equally be problematic from a legal perspective:
I would argue against providing for advance directives to be the authorisation for assisted dying. One thing that I would say is that we do not currently have very clear law on advance directives about other things, such as the refusal of treatment.13
Using the example of advance directives being used to decline future possible medical treatment, Dr Potts highlighted the challenges of interpreting these and outlined the potential role of proxy decision-makers in this context:
When it comes to declining future possible medical treatment, advance directives can be notoriously difficult to interpret in the face of the particular set of circumstances that apply. To anybody seeking to write an advance directive, we would normally recommend that they appoint a proxy decision maker to interpret the directive in the light of the circumstances on the scene. That does not mean that the proxy decision maker helps them do what they have said that they want to do.13
The Committee has heard concerns that existing legal definitions of capacity are currently subject to ongoing debate and review and, as such, any definition included in the current Bill risks becoming outdated. However, the Committee has equally heard evidence that existing definitions are unlikely to change in the near future, that capacity is a well-established and well-understood concept within the medical professions and that the provision of additional training and guidance should help to ensure medical professionals are suitably equipped to be able to test for capacity, should the Bill become law.
The Committee has heard various views on whether determining capacity of individuals should be the responsibility of the medical professional responsible for handling a request for access to assisted dying or should be outsourced to other professionals with specific expertise in this area. The balance of opinion from organisations representing the medical professions seems to be that assessing capacity is within the existing core skillset of general practitioners. At the same time, the Committee notes evidence that such assessments can at times be time-consuming and complex and may require external input, for instance from psychiatry. In such circumstances, it notes calls for additional clarity in the wording of the Bill regarding the status of such external input in determining an assessment of capacity.
The Committee notes evidence of the potential need for additional specialist expertise to enable the capacity of individuals living with certain life-limiting conditions to be appropriately assessed. It further notes evidence of the important role other professionals, including social workers and mental health officers, can play in assessing capacity.
The Committee concludes that, should the Bill progress beyond Stage 1, it will be important for the Scottish Government, in consultation with relevant specialist bodies, to reflect further on the potential resource implications for the medical professions of assessing capacity of individuals requesting access to assisted dying.
The Committee has heard a number of concerns about the reference to "mental disorder" in the sections of the Bill dealing with assessment of capacity. Specifically, it has heard concerns that the current wording of these provisions could result in a situation where anyone with a mental disorder could automatically be deemed not to have capacity and would therefore be excluded from eligibility for assisted dying. Some contributors have argued that such a blanket approach could be deemed as discriminatory under the terms of Article 12 of the UN Convention on the Rights of Persons with Disabilities. Others have suggested that this issue might best be resolved by removing reference to "mental disorder" from the Bill entirely. The Committee concludes from this evidence that, should the Bill progress beyond Stage 1, it will be necessary for the Scottish Government, in consultation with relevant specialist bodies, to examine this issue further to determine the most appropriate form of words that will enable the capacity of individuals with a mental disorder to be assessed in a way that is fair and non-discriminatory while also offering suitable protections for vulnerable individuals.
The Committee has concluded from evidence that there is a need for further clarity as to how those with fluctuating capacity will be assessed to determine their eligibility or otherwise for assisted dying. The Committee highlights this as a point for further examination by the Scottish Government, in consultation with relevant specialist bodies, should the Bill progress beyond Stage 1.
The Committee acknowledges evidence it has received making the case for the use of advance directives to be permitted in relation to requests for assisted dying. At the same time, it has heard persuasive evidence that permitting the use of advance directives would be legally and practically problematic in the context of this Bill. It also recognises Liam McArthur's intention in drafting the Bill explicitly not to permit advance directives.
Initial request for assistance
Section 4 of the Bill is entitled "Request for assistance: first declaration". As set out in the Explanatory Notes1 accompanying the Bill, "Section 4 sets out the preliminary step in the process a terminally ill adult must complete in order to be provided with assistance to end their own life. This is called a "first declaration" and takes place after a terminally ill adult has indicated to a registered medical practitioner (doctor) that they wish to be provided with assistance to end their life."
Duty to raise assisted dying
The Committee heard a range of views on the question of whether medical practitioners should have a duty to raise assisted dying as an option when considering end-of-life care with a terminally ill patient.
In written evidence, Dying with Dignity Victoria Inc, Australia highlighted the existence in legislation on assisted dying in that jurisdiction of a clause explicitly prohibiting medical professionals from initiating a conversation about assisted dying with their patients. They expressed concern that this provision has had the effect of unnecessarily restricting access to "voluntary assisted dying" (VAD) in Victoria:
This was intended to ensure that doctors were not able to coerce patients to access VAD, but in an open and honest patient-doctor relationship, it would be expected that a doctor provides all treatment options for a patient to consider before providing informed consent to a specific course of treatment or the refusal of any treatment. The omission of VAD as an option could undermine the doctor-patient relationship with distrust. There is a much lower usage of VAD in Victoria than in other states, suggesting unnecessary suffering here.2
A number of submissions to the Committee's call for views highlighted existing case law as potentially already establishing a legal duty on medical professionals to raise all reasonable treatment options with their patients and the implications this could potentially have with respect to the current Bill. In her written submission, Dr Juliet Spiller argued:
Case law mandates that all reasonable therapeutic options should be offered and discussed (Montgomery vs. NHS Lanarkshire 2015). The Bill fails to address the possibility that doctors may be under a legal duty to raise the subject of AD [assisted dying] with all eligible patients where it might be considered a potential reasonable “treatment” option. If this is not a desired outcome of the Bill then there should be a clause stating that there cannot be a duty of care on doctors or other healthcare professionals to raise the option of AD.3
Asked whether there should be a duty on medical practitioners to raise assisted dying as an option for end-of-life treatment and care, Stephanie Fraser from Cerebral Palsy Scotland was clear in her view that there should not:
I come back to the point that people with CP [cerebral palsy] struggle to access care and support. We are concerned about the change in the doctor-patient relationship if assisted dying were to be proactively suggested.4
Lyn Pornaro from Disability Equality Scotland argued that assisted dying should not be considered as a treatment option and that individuals should be made aware of it as an option only in specific circumstances:
They should be aware of the option, but other options should be fully discussed first—that is what our members were saying—rather than people being given all the information about assisted dying at the same time as all the other information. That would give people time to gradually process that and have their questions answered, as and when they need that.4
Conversely, Dr Sandra Lucas and Dr Rhona Winnington from the University of the West of Scotland argued that the Bill should be clarified in a way that would enable health practitioners to initiate a conversation about assisted dying as part of a broader discussion of treatment options, pointing to the example of the law governing assisted dying in Western Australia:
Clarity would be welcome on how discussions about assisted dying may be initiated. For example, section 10 of Western Australia’s Voluntary Assisted Dying Act 2019 allows healthcare workers to proactively discuss assisted dying if relevant to the patient’s condition as part of a broader conversation about treatment options, likely outcomes, and palliative care. This proactive approach offers an opportunity for clear and transparent conversations and ensures patients are fully informed of all options within their palliative care plan.6
Witnesses representing medical professions were generally of the view that medical practitioners would wish to have the freedom to discuss all available options with their patients and that this could include non-treatment options such as assisted dying.
Dr Iain Kennedy from British Medical Association (BMA) Scotland told the Committee:
The BMA’s position is that doctors should have the right not to discuss assisted dying but that they should also not be penalised in any way for raising the issue. We want doctors to be protected, whether they wish to raise the issue or decide not to do so. Both aspects must be explicitly provided for.7
Colin Poolman from the Royal College of Nursing argued that placing no duty on health practitioners to raise assisted dying with their patients was also important to protect health practitioners' own mental health:
That goes beyond the idea of conscientious objection because some people might find it mentally harmful to have that discussion, which is why it is our view that there should not be a duty on people to have those conversations.7
Mark Hazelwood from the Scottish Partnership for Palliative Care reiterated concerns that the Montgomery vs. NHS Lanarkshire case could be interpreted as already constituting a common law duty for doctors to raise the topic of assisted dying with patients. He added:
If a doctor raises assisted dying proactively, that has the potential to shut down the exploration of other issues and problems. It has the potential to send very negative messages to the patient that their life is not valued, that other measures might have been deemed to be inadequate, and that there is not hope.7
Dr Sarah Mills from the University of St Andrews argued that placing a duty on doctors to raise assisted dying proactively could also put them in a difficult position given that predicting the point at which a patient might be approaching end of life is often very difficult to do. She went on to argue:
There is also the fact that a doctor cannot raise something in a medical consultation in a way that is neutral. If a doctor says to someone, “Have you thought of quitting smoking?”, that is not a neutral question. With most of what we bring up in a consultation, patients take it to mean that we are in favour of it, whether or not we try to present it in a neutral way.7
Dr Mills concluded by saying:
Given the difficulty in identifying patients who may be dying and the weighted nature of bringing up the issue of assisted dying in a consultation, it is not possible to tell doctors that they have a duty to do so.7
Rami Okasha from CHAS outlined three reasons why, in his view, it would not be ethical to proactively raise assisted dying as an option in end-of-life care with a young person or their family:
The first is the very privileged relationship that healthcare professionals have with children and young people and their families; they may have known the young person for a considerable period of time prior to the age of 16.
Secondly, there are the broader issues around the appropriateness of the age threshold—we may come on to those. The third reason is the difficulty of prognosis in relation to disease that presents in young people. It is often extremely difficult to understand what a prognosis may look like where an individual clinician is dealing with a very rare condition that they may not have previously seen in Scotland.7
Dr Mills highlighted a further potential complication which she felt would make it inappropriate to place a duty on doctors to raise assisted dying proactively as an option in end-of-life care:
Primary care practitioners may be in a position, because of the state of the NHS, where they do not have a diagnosis for a patient whom they have referred to secondary care. It is unfair to require a GP to have a discussion with an as-yet-undiagnosed patient about assisted dying from a condition that has yet to be diagnosed. I think that that circumstance would not be unique in the way that one might hope that it would be.7
During his evidence to the Committee, Liam McArthur underlined that, although he did not wish to interfere in discussions between a medical practitioner and their patient, his intention in drafting the Bill was that any discussion of assisted dying would have to be initiated by the patient:
Listening to the evidence that the committee has heard in recent weeks, I recognise that, as much as one would like definitive clarity, proscribing or prescribing what a medical professional can and cannot discuss with their patient is territory into which we, as parliamentarians, probably need to tread very carefully. The expectation is that the process is initiated by the patient making the request, and thereafter the process and the safeguards that we have taken the time to discuss this morning would kick in.14
The Committee notes the range of evidence it has received on whether or not it should be specified on the face of the Bill that medical practitioners should have a duty to raise assisted dying when discussing end-of-life care options with their patients. It further notes Liam McArthur's intention, in drafting the Bill, to create an expectation that the assisted dying process should be initiated by the patient making an initial request for assistance.
The Committee considers that, should the Bill progress to Stage 2, there may be merit in further exploring the extent to which the wording of the Bill may need to be amended to provide suitable legal clarity and protections for medical practitioners, whether they choose to raise assisted dying with their patients or not. The Committee is equally conscious that this issue borders on the limits of the legislative competences of the Scottish Parliament. As such, there may also be merit, should the Bill become law, in exploring alternative non-statutory means of providing additional legal clarity, for instance through the issuing of guidance.
'Doctor shopping'
Evidence submitted to the Committee raised the prospect that there may be a risk, under the legislation, of individuals engaging in so-called 'doctor shopping', whereby they would seek multiple opinions from multiple doctors in an effort to have their request to access assisted dying ultimately accepted. Witnesses representing the medical professions were asked whether a requirement for any medical professional wishing to be able to consider requests for assisted dying to be included on a register might address this potential issue.
In its written submission, the Mental Welfare Commission for Scotland made the case for creating a central register of psychiatrists involved in assisted dying as a means of combatting the potential risk of 'doctor shopping' and outlined a number of other related benefits of such an approach:
Creating a central register of psychiatrists who opt-in to undertake the role overseen by an independent body (akin to the list the MWC holds for psychiatrists who undertake other legal duties) might also safeguard against ‘shopping’ for a psychiatrist if the opinion provided does not concur with the views of the medical practitioner under section 6. It will also help to ensure (as part of the measures expected by the European Court of Human Rights for decriminalising medical assistance in dying (MAID)) that there are increased protective measures for vulnerable people.15
Dr Stephen Potts from the Royal College of Psychiatrists in Scotland was in agreement with the Mental Welfare Commission for Scotland's assessment:
Yes. A register could do that, provided that there was provision for a second opinion from somebody else on the register. In other words, opinions are sought from the registered professionals; if there is doubt or disagreement, it is reasonable to allow room to request a second opinion through the same route, but not a third, fourth or fifth opinion.16
However, Dr Potts went on to suggest that such an approach may not be applicable to other categories of medical practitioner involved in assisted dying:
I am not so clear about whether that could also apply to the assessing doctors who refer to psychiatry. There is certainly room for doctor shopping there.16
As well as supporting the creation of a register, Professor Colin McKay from Edinburgh Napier University floated the idea of creating an ethics committee to oversee decisions by medical practitioners on agreeing individuals' requests to access assisted dying as an alternative means of combatting the risk of so-called 'doctor shopping':
We suggested that consideration might be given to a broader model, such as an ethics committee-type of model. That is not unheard of in other areas, such as, historically, gender reassignment, human tissue donation, in vitro fertilisation and even research. If an academic researcher wants to interview a person with a learning disability, they have to justify that to an ethics committee, and one might think that the decision that we are discussing is more consequential than that one. It is about having something that supports a more nuanced, individualised and multidisciplinary process.16
Dr Chris Provan from the Royal College of General Practitioners argued that creating a separate service responsible for administering requests for assisted dying would be the best means of minimising the risk of so-called 'doctor shopping'.7
Dr Iain Kennedy from BMA Scotland expressed similar concerns about the risk of 'doctor shopping' and set out what provision might be needed within the Bill to minimise that risk:
There should be open and transparent regulation, and there should be an independent body to provide oversight, monitoring and review and therefore reduce the likelihood and risk of doctor shopping.7
Giving evidence to the Committee, Liam McArthur argued that the process set out in the Bill was suitably robust to ensure that 'doctor shopping' would be an ineffective mechanism for circumventing its multiple safeguards:
The bill has pretty robust protections regarding how the request and any assessments will be made. When those eligibility criteria are not met, the process will cease. It would still be possible for any patient who was deemed ineligible to access assisted dying to go to another medic and seek another opinion, but it is not immediately obvious why another medic would automatically come to a different opinion.21
He concluded:
We trust our medical professionals to make many life-altering or even life-ending decisions, and we ensure that they have the training to make the decisions that they must make. In this instance, we will require a second medical practitioner to make assessments, too. Ultimately, if the bill were put in place, it would be the most heavily safeguarded end-of-life choice available.14
The Committee notes the concerns that have been raised about the risk of individuals engaging in so-called 'doctor shopping' as a means of accessing assisted dying in situations where their initial request for assistance is declined following assessment by a medical practitioner. It further notes the conclusion of Liam McArthur that the safeguards set out in the Bill should be sufficient to prevent 'doctor shopping' from taking place.
Nonetheless, should the Bill progress to Stage 2, the Committee considers it may be beneficial to explore further, via amendments, the potential additional safeguards against 'doctor shopping' proposed in evidence, including creation of a central register of psychiatrists or an independent body or ethics committee to oversee, monitor and review medical practitioners' decisions.
Psychological support
In their written submission, Dr Sandra Lucas and Dr Rhona Winnington from the University of the West of Scotland made the case for the provision of comprehensive psychological support to all those involved in the assisted dying process from the outset:
One specific problem that has emerged from the New Zealand legislation is the lack of grief and bereavement support for family members and friends after an assisted death. To address this, grief and bereavement support should be incorporated into the Scottish legislation from the beginning, ensuring a comprehensive, wrap-around service for all involved. This is particularly important as assisted dying represents a new legal medical service that challenges traditional boundaries of care. Additionally, this provision should be extended to all healthcare professionals who may encounter assisted dying. Providing structured support for families, friends and healthcare providers will help to navigate the emotional impacts and ensure that those involved in the assisted dying process receive the necessary emotional and psychological support.6
Scottish Action for Mental Health (SAMH) and See Me went so far as to argue that the Bill should include an explicit right to psychological support:
We believe the Bill should be amended to ensure that psychological support is offered as standard at the time of the initial application, and is also available at any point during the process (including during the proposed period of reflection following the medical assessments). If the Bill becomes law, the Scottish Government should work with stakeholders and people with lived experience to develop an appropriate person-centred offer of psychological support to accompany the new rights arising from the Bill.24
Witnesses representing the medical professions were asked whether, before commencing the assisted dying process, the individuals and medical staff involved should be offered some form of tailored psychological support. Dr Stephen Potts from the Royal College of Psychiatrists in Scotland responded:
I suppose that the answer to that question partly depends on what is meant by “support”. In an ideal world, every medical service should have access to psychosocial assessment and management for their patients where that is needed...
As for whether staff members might need it, if you are part of a nursing team and one of your patients seeks and is granted assisted dying, that is likely to be a significant emotional issue for you and for the rest of your team, and you might well need some discussion about it. As with what happens after a suicide on a psychiatric ward—a very significant adverse event—there should be routine provision of psychological support to all the members of the team from all of their disciplines.16
Professor McKay from Edinburgh Napier University pointed out that, to ensure such support was consistently available, the Bill would need to specify who should be responsible for providing that support:
It might be an issue for health boards, for example, to ensure that that is the case. After all, if we do not have that, I am not sure where support will be found.16
The Committee notes various calls in evidence for the Bill to make additional provision for individuals requesting assisted dying and the healthcare professionals supporting them to be able to access tailored psychological support as part of the process outlined in the Bill. The Committee highlights this as an issue that will need to be addressed by the Scottish Government and organisations representing healthcare professionals, should the Bill become law.
Period of reflection
As set out in the Explanatory Notes accompanying the Bill, section 9 of the Bill "...provides for a period of reflection which begins on the date the first declaration is made." The Explanatory Notes go on to describe the purpose of the period of reflection as being to provide an opportunity for the terminally ill adult requesting an assisted death "to consider their decision and discuss with others if they wish". The provisions in section 9 of the Bill mean that, in normal circumstances, a second declaration cannot be made until a period of at least 14 days has elapsed. Where it is judged that the terminally ill adult may have fewer than 14 days to live, the 14-day period can be reduced to no fewer than 48 hours, provided both registered medical practitioners involved agree and have completed the relevant part of the practitioners' statements.
In oral evidence to the Committee, Julian Gardner, Chairperson of the Voluntary Assisted Dying Review Board in Victoria, Australia, highlighted some potential practical challenges with stipulating a 14-day period of reflection as part of the process set out in the Bill:
Of those who have a first assessment in Victoria, 34 per cent die before they get to the point of having the medication dispensed. Of those who die without medication, 60 per cent die within 14 days of the first assessment. You can shorten that period, as you can in the Scottish bill. I was told last week that 25 per cent of the cases in Queensland and WA involve a request to shorten the nine-day period, so unless you have a vastly different health system, I suspect that the majority of people who seek such end-of-life care would die before they ever got the medication, because 14 days is too long.1
This view was echoed in the written submission from Christians Supporting Choice for Voluntary Assisted Dying (Australia), who similarly expressed a view that the normal period of reflection should be reduced from the period of 14 days proposed in the Bill:
I believe that the 14-day period for reflection could be reduced without reducing the effectiveness of the safeguards. The reason for this is that the person diagnosed with the terminal illness generally has already had considerable time to reflect on the outcome of their illness and their desire for assistance for an assisted death before making their initial request, as well as time during the assessment process. A 14-day time frame merely extends the time of the suffering they find intolerable. In Australia the maximum time of reflection varies between no set time and seven days.2
Conversely, in their written submission to the Committee's call for views, Jordon Anderson argued that the period of reflection should be considerably longer than 14 days:
The decision to end a life shouldn’t be taken after one consultation with a GP. There must be lots of contact, health checks and discussions. There should also be a waiting period between the initial request and final decision of at least 12 weeks to allow for reflection.3
In its written submission, End of Life Ireland described the period of reflection set out in the Bill as "probably unnecessary", concluding:
No-one arrives at the decision to apply for AD without careful reflection.4
The written submission from Scottish Action from Mental Health and See Me described the 14 day period of reflection as being, in their view, "relatively short" and, whilst acknowledging this may be desirable for those seeking an assisted death, concluded:
We do note that significant periods of negative mental ill health which, while not resulting in a lack of capacity, could nevertheless influence decision-making can last for periods much longer than this.5
In its written submission, Totara Hospice in New Zealand argued that, whatever the period of reflection, it was fundamentally important that the timetable was patient-led:
Two weeks is a very long time for some people if they continue to suffer. It is reasonable for others. The point being - make sure that the reflection period is patient centred and supports patient choice and does not inadvertently become a tool for bias or barrier.6
The Committee notes the varying views expressed in evidence on the proposed period of reflection in the Bill. Whilst acknowledging concerns that a period of 14 days is viewed by many to be too long, the Committee further notes that this period can be reduced to no less than 48 hours in circumstances where the individual concerned is expected to have less than 14 days to live. Nonetheless, should the Bill progress to Stage 2, the question of whether the default 14-day period of reflection should be revised may be a legitimate area for further debate and potential amendment.
Signing by proxy
According to the Bill's Explanatory Notes1, section 12 of the Bill provides that, in the event they are unable to sign their own name (for instance, due to a physical impairment or being unable to read), "...a terminally ill adult can authorise a proxy (that is, a person legally allowed to act on behalf of another person) to sign the first and/or second declaration forms on their behalf". The proxy's signature must be witnessed and the proxy must be either "....a solicitor, a member of the Faculty of Advocates, or a justice of the peace in Scotland" but cannot be "...a relative, or person otherwise closely connected to the terminally ill person" or "...a person who is a beneficiary in the will of the terminally ill person".
Parkinson's UK Scotland expressed support for this provision in the Bill as addressing the particular circumstances of individuals living with Parkinson's:
People with Parkinson’s often experience issues with handwriting from an early stage with the condition and can have particular difficulties with signatures. We recognise that the Bill provides for a person who has issues with handwriting to use a professional proxy to sign paperwork on their behalf. We believe that this would be a necessary safeguard against potential coercion.2
The Law Society of Scotland highlighted specific concerns around the role of solicitors when asked to be a proxy for someone who could not sign assisted dying forms themselves. The Law Society of Scotland was concerned that the way section 12 was worded may place duties on solicitors which were not intended. In its response to the Committee’s call for views, they explained:
… our concern with section 12 of the Bill is that this requires a solicitor to perform more than a ‘notarial’ execution. This is because section 12(4) requires the proxy to reach a judgment about the person’s understanding of the effect of the document. 3
It continued:
We would also suggest that it is extremely likely that a solicitor acting as a proxy would give rise to a solicitor-client relationship between the solicitor and the person. In the event that acting in this capacity does establish a solicitor-client relationship a solicitor requires to exercise and give due regard to the rules of professional conduct and behaviour, recognising that his or her professional obligations are not only to their clients, but to the courts, the legal profession and the public.3
Lynda Towers from the Law Society of Scotland expanded further on this point in oral evidence to the Committee:
Doing that might, in effect, go into giving legal advice to that patient. If lawyers give legal advice, they are obliged to go through a whole lot of bureaucratic, if you like, steps to establish a client-solicitor relationship.
Therefore, you are asking lawyers to do something more than has been done in the past. You are creating a new relationship, and the lawyer would have to be satisfied that they had explained all the legal implications of the document. That is probably not what was intended, but given the way that it is worded, that is the effect of the provision.5
In written evidence, Dr Michelle McMurray highlighted concerns about a potential conflict of interest in making provision for solicitors to act as proxies in signing documents:
If solicitors can be proxies, they would financially gain via legal fees. Which is an incentive to provide such a service.6
In written evidence, Logos Scotland raised concerns about what it perceived to be the risks of permitting signing by proxy as part of the process outlined in the Bill and what it saw as an associated contradiction in the Bill's provisions:
The use of proxy within the Bill also increases the likelihood of bad faith actors being involved in the process. The legislation requires the individual to be able to take the medication themselves – that is the underpinning principle of the Bill. However the Bill also makes provision for those who are unable to sign the papers themselves and allows the use of a proxy.7
The Committee draws attention to the range of practical concerns that have been expressed in evidence regarding the provisions of the Bill that enable signing by proxy. It considers that, should the Bill progress to Stage 2, it is likely that these will need to be addressed via amendment, based on further advice and input from the legal profession.
Provision of assistance
Section 15 of the Bill sets out how a person will be provided with assistance to lawfully end their own life, once all of the qualifying conditions are meti. The Explanatory Notes state that it is for the person themselves to decide if, when, and where they wish to be provided with an approved substance to enable them to end their life. The Explanatory Notes also state that "there is no time limit by which a person must have decided to end their life, and/or have ended their life, after a second declaration has been made".1
The assistance that may be provided under section 15 of the Bill includes:
providing the substance with which the terminally ill adult can end their own life;
staying with the adult until they have decided whether they wish to use the substance and, if so, until they have died; and
removing the substance if they decide they do not wish to use it.
Respondents to the Committee's call for views raised questions over what is described as assistance, particularly around what types of physical assistance by medical practitioners or a third party would be permissible, and whether different means of administration would be permitted under the Bill.
The wording of the Bill does not explicitly state that the substance would have to be self-administered. However, the Policy Memorandum states:
It is fundamental to the Member’s policy that a person is making a settled, voluntary choice to end their life, to be, if assessed as being eligible, legally provided with assistance to do so, which they must administer themselves.2
A definition of self-administration is provided in the Explanatory Notes accompanying the Bill and there are also numerous provisions within the Bill that make reference to the person ending their own life. For example, the long title of the Bill is:
An Act of the Scottish Parliament to provide for the lawful provision to terminally ill adults of assistance to voluntarily end their own lives; and for connected purposes.1
Some stakeholders called for further clarity around whether, in circumstances where an individual is physically incapable of self-administering the substance, they could be physically assisted to do so by a medical practitioner or third party. In its written submission, MND Scotland raised concerns that people with progressive and degenerative terminal illnesses, such as MND, may lose the ability to use their hands or swallow over time and that this would mean that they would also lose the ability to self-administer. The organisation argued that this is not only discriminatory but might also lead individuals with such conditions to seek an assisted death at a point earlier in their illness than they might otherwise choose.4
The Committee took evidence from witnesses in a number of countries on their experiences of the implementation of Assisted Dying in those jurisdictions. Professor Ben White described the process in Victoria, Australia, where the law on assisted dying had originally required self-administration. However, he went on to explain that:
...it became clear that there is a cohort of people who might not be able to access that because they have a physical disability so, to avoid discrimination on the basis of physical disability, the option of practitioner administration where self-administration is not possible became part of the debate and discussion around the Victoria law.5
"" "
Julian Gardener AM added that, according to the current law on assisted dying in Victoria:
it is also possible to administer the medication yourself via a nasogastric tube or a percutaneous endoscopic gastrostomy—PEG—tube.5
The Bill does not explicitly require oral administration. Responses to the Committee's call for views suggested that, on this basis, there was an assumption that administration could be through a number of alternative means. In his evidence to the Committee, Dr Potts from the Royal College of Psychiatrists in Scotland offered examples from other jurisdictions to argue that the definition of "self-administration" might be considerably broader than might be initially interpreted from the text of the Bill:
In other jurisdictions, notably Holland and Belgium, there is much more use of active administration of medication, sometimes by intravenous injections. There are jurisdictions where a doctor can set up an intravenous infusion and all the patient has to do is to press a button to release the medication into their bloodstream. The question in relation to the bill is, does that count as self-administration? Is that assisted administration by a doctor? Yes, but who has taken the final decision? It is still the patient. There is the possibility that a patient, could, for example, with the blink of an eye, turn on a machine that administers the medication. As I read the bill, that would still count as self-administration.7
Vicki Cahill from Alzheimer Scotland argued that the Bill would benefit from more clarity on the question of self-administration, particularly as it interacts with the assessment of capacity:
I go back to the point about ensuring that part of that capacity is the ability to act. Being able to self-administer requires that ability, so legislation needs to consider that.8
Stephanie Fraser from Cerebral Palsy Scotland offered examples of head switches and percutaneous endoscopic gastroscopy as potential alternative means of self-administration but also argued that there was a need for greater detail on the face of the Bill on this point:
The way in which it would happen is being left to secondary legislation. We would like to see some aspects of it being explored at this stage rather than left to later direction. 8
Witnesses representing medical professions were strongly of the view that additional clarity was needed on the parameters of self-administration to ensure that healthcare professionals were suitably protected under the terms of the Bill. Colin Poolman from the Royal College of Nursing Scotland told the Committee:
We do not want to leave any ambiguity, because we know that, in all areas of life, these things are tested when there are disputes. I would hate for us to have gone through a process and for there to be issues for practitioners, who will not just be medics—I think that nurses, predominantly, will be in the position of being authorised practitioners. The bill needs to be much clearer—as clear as it can be—so that there is no ambiguity about what self-administration is.10
Some respondents to the Committee's call for views called for the scope of the Bill to be expanded to enable the substance to be administered by a health professional, for example, by injection. However, in his evidence, Dr Chris Provan from the Royal College of General Practitioners Scotland sounded a note of caution on this point:
As it stands, the bill is about self-administration. There might be issues with a patient not being able to self-administer because of their condition, as you have heard in other evidence, but extending the bill’s provisions to cover a doctor administering medication to end a life would be a step that would alter the whole framework under the bill. 10
During his evidence, Liam McArthur argued that "the self-administration element is an integral part of the process."12 He went on to reflect on the differences between this Bill and the Terminally Ill Adults (End of Life) Bill currently under consideration in the House of Commons, which provides comparatively more detail regarding the definition of self-administration. The UK Bill states that a health practitioner may:
prepare that substance for self-administration by that person
prepare a medical device which will enable that person to self-administer the substance, and
assist that person to ingest or otherwise self-administer the substance.
Dr Amanda Ward, advisor to Liam McArthur, told the Committee that it was necessary for the UK Bill to make these provisions due to an important difference in the existing law in England and Wales compared to Scotland:
They have the Suicide Act 1961, which specifically prohibits assistance in dying. We do not have that prohibition in Scotland, so there is a distinction in the existing law.12
Some stakeholders raised concerns over complications that might arise as a result of taking the substance provided. The Committee heard evidence from witnesses on the efficacy of substances used in assisted dying in other jurisdictions and the experience of incidences of complications (based on differing means of administration). Julian Gardner AM reported in his evidence to the Committee that in Victoria, Australia, "100 per cent of the people who have taken the medication in whichever form have died" albeit within differing timescales. He added that he was "not aware of any situations in other states where the medication has not been totally efficacious."5 Dr Stefanie Green from the Canadian Association of MAiD Assessors and Providers told the Committee that, in Canada, where intravenous administration is used, "the substance is 100 per cent effective when it is in the intravascular system".15
Fiona McIntyre from the Royal Pharmaceutical Society Scotland emphasised the importance of ensuring the substances used were properly authorised and licensed, as a means of reducing the risk of complications:
The preferred option for the Royal Pharmaceutical Society is for all medicines that are being used to have a marketing authorisation and to be licensed for use, because that safeguards all the healthcare professionals who support the use of that medicine and manages all the risks of that use. We would therefore have a preference for a licensed product.10
Dr Amanda Ward, advisor to Mr McArthur, informed the Committee that, in developing the Bill, the Member had engaged extensively with pharmaceutical colleagues and other stakeholders on the subject of medication and methods of self-administration:
I want to assure the committee that, although there are sensitivities around discussing the medication and the pharmaceutical aspects, we have explored those matters in detail. As Liam McArthur said, there were issues 20 years ago in Oregon, when assisted dying was new or emerging, but there is now a very refined protocol that we know works at 100 per cent effectiveness.12
Dr Chris Provan from the Royal College of General Practitioners Scotland highlighted doctors' concerns around the extent to which, and in what way, they would be expected to intervene should complications arise during the process and emphasised the need for clear guidance on this point:
Should they treat the adverse reaction, because they are not allowed to end a patient’s life? That comes back to the protocols and the need to know exactly what the role of the doctor is in such situations.10
Similarly, Dr Gillian Wright from Our Duty of Care highlighted concerns of Allied Health Professionals around their potential involvement in the process set out in the Bill and a lack of clarity over how they might be expected to respond in the event of complications:
What do staff do if, for example, the patient has seizures and they [the Scottish Ambulance Service] are called, and there is a healthcare professional—perhaps a nurse—sitting with the patient? What do they do at that point? Do they transfer the patient to hospital or wait with the patient until that person dies? ...I was also concerned when I read the report from the medical advisory group, which contains talk of “a rescue IV” being made available to the doctor. What does that mean? Does it mean that the doctor has licence to kill the patient and administer a lethal drug at that point or that the doctor has licence to sedate the patient if they are seizing?19
Dr Gordon Macdonald from Care Not Killing expressed concern that evidence from other jurisdictions where assisted dying is legal suggested to him that, over time, models based on self-administration would transform into models where physician-administration was permitted:
It is interesting to note that, in Australia, which has a mixed model, in some states, the method is primarily self-administration, but the doctor can step in and euthanise the patient if that is not working. In other states, the method is primarily euthanasia by the doctor. It seems to be the case that, over time, the method has moved towards euthanasia.19
When asked about potential concerns from health professionals that they may be liable to prosecution if called upon to intervene in case of complications during an assisted death, Laura Buchan from the Crown Office and Procurator Fiscal Service was not convinced that such a scenario would necessarily constitute an offence but went on to suggest that further clarity would be helpful:
I do not see from the proposals in the bill that there would be an offence if, for some reason, something went wrong and the medical practitioner was required to step in. I cannot think of, or consider, what such an offence might be. However, again, it would be far better for medical practitioners to have clarity. We have dealt with cases in which there is a “Do not resuscitate” notice or plan in place, so that it is clear for those involved. It would be helpful to have some clarity in the bill around that process and what happens in terms of self-administration.21
Assistant Chief Constable Steve Johnson from Police Scotland was of a similar view that clear guidelines in this area would be important. To illustrate this point, he cited the example of a third party who may be present in the room when the substance is administered but, because of being unused to witnessing a person's death, may be inclined to intervene when they perceive the individual to be in distress when, in reality, this would be "perfectly normal and is how the substance works". He concluded:
You would seek to limit people’s desire to intervene, rather than leaving it to happenchance.21
Section 15 of the Bill also makes provision that the coordinating registered medical practitioner (cRMP) or authorised health professional:
may be accompanied if they deem necessary;
must remain with the person until the person decides whether to use the substance provided to end their own life and, if they decide to do so, until they have died;
need not be in the same room as the person; and
must take back the substance and remove it from the premises if the person decides not to take the substance.
Some respondents to the Committee's call for views questioned the resource implications and practicalities of these provisions, particularly the requirement that the health professional should stay with the individual until they have died. Certain of these respondents observed that some deaths may take longer than others while others noted there would be additional time and resource commitments associated with a health professional being expected to travel to the individual's home, if that is where they decided to administer the substance.
In its written response to the Committee, Police Scotland also questioned how, if there was no requirement for the health professional to stay in the room where the substance was being administered, they could be sure there had been no intervention by a third party who was in the room, in breach of the provisions of the Bill. During his oral evidence to the Committee, Assistant Chief Constable Johnson elaborated on Police Scotland's concerns:
Section 15(5) says that someone could provide the substance and remain present until the person had ended their life. However, on my reading— which I think is a shared one—of section 15(6), having provided the substance, that person may then leave. Between subsections (5) and (6) there is ambiguity on whether there needs to be external observation of what takes place in the room when the person goes on to self-administer, or what happens if other people present in the room intervene. From the perspectives of policing and investigation, we need clarification of those aspects. It would be terrible to think that the person might have changed their mind but that someone else in the room had administered the substance on their behalf. At that point, this legislation would feel very frail.23
Addressing these concerns, Liam McArthur highlighted the process of assisted dying that is in place in certain other jurisdictions, where "the medication is dispatched to the patient and the medical professional is not present when the medication is delivered12". He argued that, compared to the approach in these other jurisdictions, the requirement under section 15 of the Bill for the health professional to be present throughout the provision of assistance added important additional safeguards, "not least to ensure that a final assessment of capacity and intent is made".12 Mr McArthur went on to address the intention behind section 15(6) (that the attending health professional need not be in the same room as the person), which he explained was to allow the person "in their final moments, to have a degree of privacy". He added:
How you manage that while ensuring that there are safeguards is probably a question to reflect on further... I am not necessarily sure that the patient’s wish for a degree of privacy and discretion at the end of their life is something that we would want to see denied, but I am happy to look at any further clarifications that might be helpful in that regard.12
The Committee acknowledges Liam McArthur's position that self-administration is an integral element of his overall approach to developing the Bill. At the same time, the Committee has heard concerns that, without further clarity, there may be a risk that this approach could result in individuals with certain conditions or physical disabilities experiencing discrimination by being unable to exercise their right to access assisted dying.
More broadly, the Committee notes stakeholder concerns that there is a lack of clarity regarding the precise parameters of the definition of self-administration and what assistance a health practitioner could legitimately provide under the Bill.
The Committee notes the additional detail provided in the UK Bill on this point but further notes that this difference in approach can be attributed to the difference in existing law in England and Wales compared to Scotland by virtue of the Suicide Act 1961.
The Committee notes concerns from some contributors to the Committee's scrutiny over the potential risk of complications associated with administration of the approved substance at the point where assistance is provided. However, it equally notes evidence from other jurisdictions where assisted dying has been legalised which suggests that such incidences of complications are rare and predominantly minor in nature. Nonetheless, the Committee highlights evidence from the Royal Pharmaceutical Society Scotland which concludes that, to further minimise the risk of such complications, it will be important to ensure any substances used in the assisted dying process are properly authorised and licensed.
Certain stakeholders have highlighted what they consider to be an inconsistency in the drafting of section 15(5) and (6) of the Bill. The former requires the healthcare professional to remain with the person until that person has ended their own life and the latter allows the healthcare professional to leave the room. The Committee recognises the intention behind these provisions, namely to allow for practical or privacy considerations, but notes concerns that any lack of clarity may have implications for law enforcement. The Committee therefore welcomes the Member's commitment to give further consideration to the drafting of this section, should the Bill progress to Stage 2.
The Committee is strongly persuaded of the importance of developing detailed guidance on self-administration and provision of assistance to ensure absolute clarity and appropriate protection for anyone who may be involved in the assisted dying process at the point where assistance is provided, be that the individual requesting assisted dying or any attendant health practitioner or third party.
Death certification
Section 17 of the Bill concerns death certification and what should be recorded on a person's death certificate when they have lawfully been provided with assistance to end their own life and died as a result. The Bill stipulates that, in the case of an assisted death, the cause of death to be recorded on the death certificate is the illness, disease or condition which led to them requesting and being provided with assistance to end their life, as opposed to the approved substance provided to them. The Explanatory Notes also state:
It is expected that the use of the approved substance will also be recorded on the death certificate.1
Some respondents to the Committee's call for views expressed concerns about the provisions of the Bill relating to death certification. Those respondents who supported the Bill thought that both the underlying illness and the assisted death should be recorded on the death certificate. Those opposed to the Bill felt strongly that recording the underlying illness would be an inaccurate and misleading record of the cause of death and argued that suicide should be recorded as the main cause.
In its written submission, NHS Education for Scotland (NES) outlined its work to design and develop educational resources to support doctors to accurately complete a Medical Certificate of Cause of Death (MCCD):
The education resources developed have a heavy emphasis that you are required to complete a MCCD honestly, accurately, and to the best of your knowledge and belief. In the case of assisted dying the cause of death will be the self-administration of the lethal medication. Therefore, to deliberately exclude the actual cause of death from the death certificate, as suggested in the Bill, would be an issue of professional conscience and would be at odds with the guidance for all other causes of death and out of line with the approach adopted in what might be considered other “sensitive” circumstances of death.2
During oral evidence, Andy Shanks from the Crown Office and Procurator Fiscal Service spoke about the process of death investigation, its purpose being to determine if there is any criminality associated with a death in Scotland. He told the Committee:
First and foremost, it is about ensuring that every death in Scotland has a medically certified cause of death. It is also about ensuring that bereaved relatives have an understanding of the circumstances in which their loved ones died and answering any concerns that they might have. It is also about identifying any lessons that can be learned for the future in order to prevent similar deaths from occurring.3
Mr Shanks confirmed that how the cause of death was recorded on a death certificate would not have any bearing on a death investigation. However, he also told the Committee that the proposed approach in the Bill would be a departure from the normal approach to death certification:
...in normal circumstances, the medical practitioner who is certifying a medically certified cause of death would do that to the best of their knowledge and belief, so the provisions would signify a departure from that. That is probably most relevant in respect of national data collection.3
The Chief Medical Officer guidance for doctors completing medical certificates of the cause of death sets out in detail how to complete a medical certificate and how to report deaths to the Procurator Fiscal. The relevant forms are included within this guidance at Annex 1. The National Records of Scotland reports on vital events, including births, deaths, marriages and life expectancy. These will include links to definitions of certain causes of death, and, in some cases, other information about statistics on those causes of death.
When asked whether his intention, in drafting the Bill, was that the terminal illness would be captured in section 1a of the death certificate with assisted dying being listed in section 2, Liam McArthur replied:
That would certainly be my view; I am conscious that others take a different view on that. I think that there is a way of ensuring that the information that is needed is captured appropriately. ... I was reassured to some extent in my discussions with the CMO and his colleagues that there is a way of navigating the matter so that it is undertaken sensitively but makes absolutely sure that the relevant information is available so that we have the understanding that we need about how the legislation is working in practice.5
During its scrutiny, the Committee also explored how recording an assisted death on a death certificate might affect the ability to make a claim on an individual's life or other relevant insurance policy. Mr McArthur told the Committee:
That was probably one of the first conversations that I had. The Association of British Insurers has confirmed that assisted dying would not be considered to be suicide.5
The Committee has heard differing views regarding what should be recorded as the cause of death on the death certificate of someone having had an assisted death. It notes that this difference of view broadly aligns with those contributors' respective positions either for or against the Bill. For transparency and data collection purposes, the Committee has concluded from this evidence that, as also acknowledged by Liam McArthur, it will be important to ensure both the illness, disease or condition which led to an individual requesting assistance to end their life, and the approved substance provided to enable them to do so is detailed on the death certificate. It further notes that there is provision for both pieces of information to be included on the MCCD form. Should the Bill progress to Stage 2, the Committee concludes that further attention will need to be devoted towards determining how best to achieve that outcome, be that through amendments to the Bill itself, the development of follow-up guidance or both.
Implications for the health service and healthcare professions
Overall service model
During its scrutiny of witnesses from Australia, the Committee heard evidence of a mixed model of service delivery across Australia in relation to voluntary assisted dying. Asked whether voluntary assisted dying is delivered as a specialist service in Australia, Julian Gardner, Chairperson of the Voluntary Assisted Dying Review Board in Victoria, responded:
It is not a specialist service, with one exception in New South Wales... It is simply a mix of general practitioners and specialists who undertake the prescribed training, and who meet the qualification requirements on length of experience and admission to a college of specialists. They might be medical practitioners who are employed in public hospitals, or they might be in private practice.1
However, Julian Gardner went on to clarify that certain aspects of the service are delivered on a centralised or specialist basis:
We do have a specialist pharmacy, though, which is centralised and Government run, which delivers the medication no matter where a person lives, free of charge. We also have a specialist service in Victoria that uses what we call “care navigators”. They are generally nurses, and they do a lot of the liaison to ensure that people have access and to overcome access difficulties.1
Professor Ben White from the Australian Centre for Health Law Research then explained the "specialist service" approach to service delivery taken in Queensland and New South Wales, with the emphasis being on ensuring there is universal access to the service across large geographical areas of the country:
In Queensland, when the service was initially established, the idea of outreach and ensuring state-wide access was not contemplated as part of that body’s role, but it became clear that there was a need; for example, some remote areas did not have access to practitioners who could assess voluntary assisted dying, which is why the centralised service, which includes both the pharmacy and the navigators that Julian Gardner mentioned, stepped in to do that role.1
In oral evidence to the Committee, Dr Chris Provan from the Royal College of General Practitioners Scotland confirmed his organisation's view that assisted dying, if made legal, should be provided as a dedicated, stand-alone service rather than being integrated into existing health services:
To get the best service for the patient, we are in favour of there being a separate service, with those people who have bought in to the service and are used to going through the process with their own protocols. Trying to add it on to a busy general practice would be very difficult, given the subtleties and importance of such situations.4
Dr Provan added:
I was very surprised to see in the bill and the notes around it the idea that such a discussion could be added into an extended consultation. The complexity of that cannot be added into an extended consultation. You heard some evidence from Australia, I believe. One of the comments from those witnesses was that such discussions do not work well in busy practices, and there is no such thing in Scotland as a quiet practice. There are even some areas where there are not many GPs, which is why we think that, for the system, the clinicians and everybody involved, especially patients, we need a central service to run this.4
Fiona McIntyre from the Royal Pharmaceutical Society in Scotland expressed similar concerns about the prospect of assisted dying being integrated into existing pharmacy services in Scotland:
The Royal Pharmaceutical Society has not discussed how the service would look if the bill were passed, but we are in favour of there being an opt-in situation, whereby a network of healthcare professionals would be able to opt in to deliver the service. Pharmacy services are experiencing similar challenges to other parts of the health service, and it is difficult to see how an assisted dying service could be accommodated within our current provision.4
In its written submission, the Nursing and Midwifery Council highlighted the example of Jersey, where provision of assisted dying is being proposed via a separate service and set out what it considered to be a number of potential advantages of such an approach:
health and care professionals would have greater choice about whether they want to opt in and take part in the service
greater oversight at a local level of the professionals involved in the service
better assurance that those participating in assisted dying have the necessary skills and knowledge required for the scope of their role
ease for people seeking assisted dying to identify the health and care professionals willing and able to carry out the functions of the assisted dying service
limited impact on existing health and care services.7
It concluded:
When considering the detail of how the service would operate in Scotland, it is important that the Scottish Government considers whether the proposed model could be delivered within the current resources without adversely impacting on existing services and already over-stretched staff.7
In evidence to the Committee, Liam McArthur expressed some concerns about the idea of assisted dying being delivered via a stand-alone service as opposed to being an integrated part of existing services provided by the NHS:
I find the idea of a stand-alone service problematic. Expecting somebody to be lifted and shifted out of a current pathway into another service at what is probably one of the most vulnerable points of their life—their final days—does not seem acceptable.9
The Committee acknowledges those views expressed in evidence, particularly from representatives of the medical professions, that providing assisted dying via a stand-alone service would, in their view, have a number of important benefits, including reducing the potential burden on existing healthcare services.
At the same time, the Committee also recognises the concerns of Liam McArthur that such an approach risks being unnecessarily disruptive to the individuals affected and could negatively affect the accessibility of assisted dying. It further notes Mr McArthur's view that the small number of individuals likely to request access to assisted dying, initially at least, should mean that the impact on existing healthcare services of providing assisted dying as an integrated part of existing services should be relatively limited. Finally, the Committee notes evidence from other jurisdictions where assisted dying has tended to be delivered as an integrated part of existing services, rather than as a stand-alone service model, with a few limited exceptions.
The Committee concludes that, should the Bill progress to become law using the service model as currently proposed, it will be particularly important to monitor the impact on existing healthcare services over time. Should the Bill progress to Stage 2, there may be merit in exploring further through amendments whether specific aspects of assisted dying would be better delivered on a stand-alone basis, in particular with a view to ensuring consistent access throughout the country.
Conscientious objection
Section 18 of the Bill, as described in the Bill's Explanatory Notes1, "provides that no one, including any individual health professional, is under any legal duty to play an active, participatory role in anything authorised by the Bill". During the Committee's scrutiny, this provision has been generally referred to as the "conscientious objection" clause of the Bill.
Scope of the conscientious objection clause
The Committee heard a range of views concerning the proposed scope of the conscientious objection clause.
BMA Scotland argued that the scope of section 18 of the Bill should be widened to allow professionals to exercise an objection to being involved in assisted dying, whether that was for reasons of conscience or not:
The BMA believes that, if assisted dying were legalised, doctors should be able to decline requests to carry out these types of activities for any reason. Therefore, there should be a general right to object which does not need to be based on matters of conscience. If it was considered important to retain some reference to conscience in the Bill, this could be achieved by modifying the wording to indicate that a decision not to participate may be for reasons of conscience or for any other reason.2
In its written submission, Hospice UK was in agreement that there may be other reasons not related to conscience that might prompt professionals to not want to be involved:
The framing of this decision by medical professionals as being one of conscientious objection is not necessarily helpful. Some professionals may have no issue with assisted dying being legalised but would wish to not participate in order to protect their own mental health and wellbeing.3
Mark Hazelwood from the Scottish Partnership for Palliative Care similarly made the case for this section of the Bill to be broadened, both in terms of the admissible grounds for exercising a right to object and the category of individuals who might be permitted to exercise that right:
We have said that professionals need to have the ability not to participate, regardless of whether that is grounded in a conscientious objection.
Lastly, the conscientious objection that is in the Abortion Act 1967—on which, to an extent, the bill draws, I think—is quite narrowly drawn. We wish to see flexibility in the bill such that people who may be peripherally involved in the process of assisted dying would also have the ability not to participate.4
In its written submission to the Committee, the Humanist Society Scotland expressed support for a conscientious objection clause but were equally clear that it must not be allowed to become a barrier to access to assisted dying:
If an individual medical practitioner objects to participating in the assisted dying process, an alternative professional must be available to ensure that a patient’s wishes are respected. Under no circumstances should a patient be unable to access an assisted death, if they meet the criteria, because medical practitioners involved in their treatment and care conscientiously object.5
Dr Sarah Mills from the University of St Andrews pointed to the need for greater contingency planning for circumstances where certain health professionals exercising an objection, conscientious or otherwise, to participating in assisted dying might have wider implications for adults with a terminal illness living in certain areas being able to access that service:
For example, if the service is to be delivered through general practices, what happens if a single-handed GP in Orkney has a conscientious objection? Who takes care of their patients? There needs to be a lot more specificity throughout the bill in order for the conscientious objection to have meaning and for there to be a legitimate back-up plan for patients whose only medical contact may be someone who conscientiously—or non-conscientiously—objects.4
Dr Murray Earle from the University of Edinburgh recognised the benefit of having a conscientious objection clause but pointed to areas where further thought needed to be given to the practical implications of having such a clause for the implementation of the Bill if it were to become law:
If we are going to have such a provision, that is good—it brings the medical profession on side. More than that, however, we need some form of referral so that a medical practitioner, if they do not wish to act in accordance with the act, as it would be, can refer someone to a practitioner who does. Naturally, that becomes problematic when we look at the Highlands and Islands and so on, where that might be difficult to do.7
Marianne Scobie from the Glasgow Centre for Inclusive Living expressed a concern that medical professionals wishing to exercise a conscientious objection might choose to leave the profession and the impact she felt this could have over time:
Our concern is that doctors with a conscientious objection would leave the profession, and that those remaining would be more likely to support assisted dying. That would shift the balance among doctors towards those who are for assisted dying, which would further compromise the doctor-patient relationship and erode trust in the medical profession.8
During the evidence session involving a number of academics and legal experts, there was general agreement amongst the witnesses participating that it would be important for conscientious objection to be clearly and comprehensively defined on the face of the Bill, as opposed to relying on follow-up guidance. Lynda Towers from the Law Society of Scotland told the Committee:
It would be desirable to have the legislation as clear as possible, and, if necessary, to have definitions, recognising that there is always a danger that, when including definitions, you will leave something out. It would be dangerous to leave something as subjective as this issue to guidance as opposed to having it in the primary legislation. Getting the conscience clause correct in the bill is the right way forward.7
In its report on the Bill, the Delegated Powers and Law Reform Committee highlighted correspondence with Liam McArthur regarding the practical application of the conscientious objection clause in section 18 of the Bill. The report states:
In its letter to the Member, the Committee explained that it could envisage a situation in which either the relevant Scottish Minister or another prominent individual, such as the Chief Medical Officer for Scotland (both of whom may have a role in the making for regulations under the Act) might conscientiously object to assisted dying. The Committee invited the Member’s thoughts on the potential problems which might arise in such a situation and how they might be addressed.10
The report goes on to outline Liam McArthur's response:
In his response, the Member reiterates the Bill does not place anyone under a duty to participate in anything to which they conscientiously object and does not envisage any prohibitive barriers to the making of regulations or the implementation of the Act in consequence of section 18.10
In evidence to this Committee, Liam McArthur explained his rationale for keeping the scope of the conscientious objection clause relatively tight:
...it would be my expectation that the clause would apply to the people who are directly involved in the process, which I think is a proportionate approach to conscientious objection. A degree of caution needs to be exercised when drawing parallels between the process that is described here and abortion legislation. I think that the way in which the conscientious objection clause works is appropriate in the context of assisted dying.12
He concluded:
Extending that conscientious objection too extensively is problematic. It is about choice for those who are actively participating in the process. Extending it more widely runs the risk of putting up unnecessary and unjustified barriers to individual patients who meet all the eligibility criteria by denying them access to that choice.12
The Committee notes the range of views it has heard concerning the proposed scope of the conscientious objection clause in the Bill. In defining its scope, it recognises the importance of striking an appropriate balance between:
protecting the interests of healthcare professionals who may, for a range of reasons not necessarily related to conscience wish not to be involved in assisted dying; and
ensuring the clause does not become an arbitrary and unnecessary barrier that, in practice, curtails the freedom of individuals to choose to request access to assisted dying.
The Committee further notes concerns expressed in evidence that the current wording of the clause is insufficiently clear. It has also been struck by the emphasis legal stakeholders have placed on the importance of ensuring there is a clear and comprehensive definition on the face of the Bill, as opposed to relying on secondary legislation to provide additional clarity.
The Committee also notes the exchange of correspondence between the Delegated Powers and Law Reform Committee and Liam McArthur concerning the practical application of section 18 and potential challenges that might arise in the event that a prominent individual such as the responsible Scottish Minister or the Chief Medical Officer for Scotland were to exercise a conscientious objection in relation to assisted dying.
In light of this evidence, the Committee concludes that, should the Bill progress to Stage 2, it will be important to give further attention to the wording of section 18, to ensure it provides an appropriate level of legal clarity and certainty for all parties involved in the assisted dying process.
Duty to refer/'No duty' clause
In their written submission, Christians in Pharmacy argued that the conscientious objection clause in the Bill should extend to there being no expectation for the professional exercising a conscientious objection to have to refer the patient requesting assisted dying to a professional who did not conscientiously object:
It is vital that conscientious objection provisions are watertight and not only protect the right of any health professional to opt out from personal involvement but also protect them from having to 'signpost' to other health professionals who do not object. Care needs to be taken that exercising their conscience does not have a chilling effect on the career progression of the health professional concerned.14
Dr Mary Neal from the University of Strathclyde took issue with the idea of placing a duty on those medical professionals exercising a conscientious objection to refer patients requesting access to assisted dying to a colleague who did not conscientiously object. In arguing her case, Dr Neal drew a comparison with abortion:
The duty to refer is morally problematic; it involves a degree of moral complicity in the practice. In the case of abortion, it is generally agreed that compromise is necessary, legally and ethically, because of the time limits that are involved... In abortion, that compromise might be necessary; in assisted dying, the case for a compromise is much weaker.7
At another point in her evidence, Dr Neal argued that, in addition to a conscientious objection clause, the Bill should include a 'no duty' clause to give full protection to any medical professional who wished not to be involved in assisted dying:
There would be a common-law duty on doctors to discuss assisted dying as treatment with their patients unless the statute specifically prescribed that they did not have to do so. That is why the Leadbeater bill has clause 4 in it and why the Scottish bill needs something similar. Section 18 would not exclude that duty, because it refers to participating—in other words, being in a hands-on, direct capacity—but indirect bureaucratic, administrative and ancillary tasks that are remote from the actual death are potentially not covered. We need both.7
In her written evidence, Tamsin Nicholson argued the case in favour of a 'no duty' clause to protect medical practitioners, by reference to the UK Supreme Court decision in the case of Montgomery v. Lanarkshire Health Board:
Montgomery requires that we (doctors) must tell patients about all their treatment options, not just the ones we feel are most relevant. Whilst assisted suicide is not easily defined as 'treatment' without specified exemption, it could fall under that bracket. This would require doctors to present assisted suicide to any patient with a terminal illness. This is highly likely to undermine patient trust in the profession and therefore, a 'no duty to raise' clause would protect against this.17
Witnesses from Australia were asked about the experience of people exercising conscientious objections in the context of Australian law on voluntary assisted dying. Professor Ben White from the Australian Centre for Health Law Research indicated that, although conscientious objection is consistently protected across all Australian jurisdictions, there are differences in how those exercising a conscientious objection are expected to act across different states. For example, he told the Committee that, in Victoria, a practitioner who conscientiously objects is under no legal obligation to refer a patient on or to provide any further information on the matter. He continued:
In other states, such as Queensland, again, there is strong protection for conscientious objection, but there is a minimal requirement for a conscientious objector who receives, for example, a first request for voluntary assisted dying to at least share information about the care navigator service that we discussed. That would be as simple as saying, “Here’s a phone number and this is the voluntary assisted dying care navigator service.” I think that that model provides better access for patients, because it can be difficult to navigate the system—that is one of the barriers that has been identified in Victoria—and having that minimal requirement ensures connection to it.18
Liam McArthur told the Committee that, in the interests of ensuring equitable access for patients to assisted dying, he would expect medical practitioners exercising a conscientious objection to refer a patient request for assisted dying to a fellow medical practitioner who would be in a position to handle that request:
There would be an expectation, as there is with the way that conscientious objection works for abortion, for the medical professional to refer the patient on to somebody who can provide support. That is an important principle in the delivery of health and care services. It protects that choice on the part of the practitioner but does not put up unreasonable barriers to patients accessing the choice that they should have to get the support and treatment that they feel that they need.12
The Committee notes the case made by certain contributors to the Committee's scrutiny of the Bill that, in addition to the conscientious objection clause set out in section 18 of the Bill, there should be a 'no duty' clause that would absolve a practitioner exercising a conscientious objection from any duty to refer a patient requesting access to assisted dying to a fellow practitioner who was in a position to deal with their request. The Committee further notes concerns from other contributors and Liam McArthur that a 'no duty' clause would create unreasonable barriers for those individuals seeking access to assisted dying.
The Committee also highlights evidence from Australia, where the existence of a 'no duty' clause in the law governing assisted dying in Victoria was felt by witnesses to have created a barrier that made it relatively more difficult for patients to access assisted dying in that jurisdiction compared to other jurisdictions in Australia where no such clause exists.
From this evidence, the Committee concludes that setting a minimum expectation for a health practitioner exercising a conscientious objection to refer on any patient requesting access to assisted dying, or at least to provide them with additional information, would strike an appropriate balance between the right of the health practitioner to be excluded from involvement in the assisted dying process and the right of the patient to be able to access assisted dying without facing unreasonable barriers to that access.
'No detriment'
Dr Chris Provan from the Royal College of General Practitioners in Scotland raised concerns that those exercising a conscientious objection could be exposed to the risk of workplace discrimination that might adversely affect their future careers and argued the case for inclusion of a 'no detriment' clause to further protect those who choose to conscientiously object:
We are very clear that we should not have to justify or approve conscientious objection or not wanting to be involved. There should be wording about it being unlawful to discriminate against anybody who has made a decision not to be involved.4
The Royal College of Nursing Scotland took a similar view and argued there should be additional protections in the Bill to ensure the staff they represent would not face discrimination whether they chose to be involved in the assisted dying process or not:
We would also like to see the Bill amended to provide statutory protection from discrimination for registered nurses so that it is unlawful to discriminate against them based on their decision to either participate or not participate in assisted dying.21
In their written submission, Humanists UK expressed support for such additional safeguards against discrimination to be included in the Bill while stopping short of supporting a right to institutional objection (covered later in this section of the report):
We would support any additional safeguards in this area, such as ensuring that a medical professional is not discriminated against for choosing to contribute or opt out of assisting a death. However, we would be against this right to conscientious objection being extended to organisations or institutions; only individuals should be able to make this choice. Employers should not be able to make or influence this choice for their employees.22
The Committee notes evidence in support of a 'no detriment' clause or similar provision within the Bill to protect healthcare staff from potential workplace discrimination as a result of their decision either to be involved in the assisted dying process or to exercise a conscientious or other objection to being involved. Should the Bill progress beyond Stage 1, the Committee calls on Liam McArthur to give the matter further consideration ahead of Stage 2.
'Opt-in' versus 'opt-out'
In connection with the conscientious objection clause, a number of witnesses argued that they would prefer to see a model whereby, rather than having to actively opt out of participation in assisted dying by exercising a conscientious objection, healthcare professionals would have the option to opt in to participation. Dr Stephen Potts from the Royal College of Psychiatrists in Scotland told the Committee:
Although many of our members have expressed a wish to opt out of participation in any questions around assisted dying, a proportion—16 per cent, I think—have indicated a willingness to opt in to a central register if that was set up.7
In written evidence, Social Work Scotland observed that an 'opt-in' model would, in their view:
...mitigate the pressure on medical professionals, and others who may be involved in the decision about eligibility, to either conform to a view they may be uncomfortable with, or to be forced to justify their opting out position.24
The Royal Pharmaceutical Society Scotland were similarly supportive of an 'opt-in' model, arguing:
This would enable pharmacists and other healthcare professionals to support the process if they were comfortable to do so but would not compel anyone to be involved if they felt uncomfortable. This would not only support individual healthcare professionals but would ensure the best patient care and experience.25
Hospice UK outlined what they perceived to be some additional benefits of an 'opt-in' model:
An opt in model for health professionals would have the advantage of providing clarity to both healthcare professionals and members of the public (through a statutory care navigator service) of how best to access an assisted dying service if this Bill is passed. It would also allow the Scottish Government/NHS to accurately map where the service is available. For individuals, health care professionals and organisations this could provide assurance and transparency.3
Drawing on its experience of same sex marriage, the Scottish Episcopal Church also advocated for an 'opt-in' model:
We have found that an opt-in arrangement works well and gives people space to follow their conscience and continue to safely work with others of differing opinions. We consider that this would be a more robust safeguard against the coercion and control of junior staff or those in a supporting role.27
Alyson Thomson from Dignity in Dying Scotland indicated that, in her experience, there were many health professionals who support assisted dying who would equally be willing to opt in to be involved in the assisted dying process:
... at Dignity in Dying we have a group of health professionals who are in favour of assisted dying: a number of doctors, clinicians and nurses from across all specialties, particularly general practice, are very much in favour of the proposals, having had to watch the suffering of their patients as they die. They would very much like to be trained and to opt in to participate.28
Professor Colin McKay from Edinburgh Napier University expressed support for this idea and went on to highlight additional benefits of having a central register in place in a scenario where a significant number of doctors choose to opt out of participation by exercising a conscientious objection:
One of the other anxieties about the bill is the idea that lots of doctors might opt out and you might end up with maverick practitioners, as it were, with people who are very pro-assisted dying just coming in and saying that they will sign off anybody. A register with a degree of oversight and regulation would be a helpful safeguard.7
Later in the same session, Professor McKay argued that the creation of a central register would have the further benefit of avoiding having to place an obligation on a practitioner who had expressed a conscientious objection to refer a patient seeking access to an assisted death onto another doctor:
We were concerned about the idea that a doctor who has a fundamental objection would have a duty to find you another practitioner. If there is a register, that problem goes away. It becomes a process that people can access.7
Dr Mary Neal was supportive of the idea of an 'opt-in' system for medical professionals, as advocated by BMA Scotland. However, she went on to argue that, even if such an approach were to be taken, a separate conscientious objection clause would still be required:
Even if there is a parallel opt-in system, you cannot exclude the possibility that ordinary people working in the NHS during their everyday practice will be confronted by the issue, so they will have to have an opt-out.7
Although doubtful about the appropriateness of providing assisted dying through a stand-alone service, Liam McArthur told the Committee he was more willing to give potential further consideration to the idea of an 'opt-in' system of participation by healthcare practitioners, with certain important caveats:
I am perhaps more sympathetic to the notion of opt-in and opt-out, but I would need to understand how that would work in practice and how to avoid creating unnecessary obstacles to people accessing the option.12
The Committee notes evidence from a number of stakeholders in support of an 'opt-in' model of participation in assisted dying for healthcare staff. It further notes the willingness of Liam McArthur to explore this model further, subject to greater clarity as to how it would work in practice and additional reassurance that such an approach would not create additional barriers to access to assisted dying for individuals. The Committee concludes that the concept of an 'opt-in' model is an area that would benefit from further exploration through amendment should the Bill progress to Stage 2.
Institutional objection
The concept of giving organisations a right to exercise an institutional objection to assisted dying was also discussed during the Committee's scrutiny of the Bill. In oral evidence, Professor Ben White from the Australian Centre for Health Law Research told the Committee:
In Australia, the first series of laws did not mention institutional objection, and that was a problem in practice. In a different way from individual conscientious objection, where it is just one person who objects and you can navigate around that, the fact that an institution as a whole does not allow voluntary assisted dying to happen can have significant issues for people in that institution.
The subsequent three states after Victoria, and indeed the Australian Capital Territory, have specifically dealt with institutional objection in the legislation by creating a framework that makes sure that patients do not miss out, regardless of where they may be cared for. 18
In written evidence, Kerstin Braun (Associate Professor of criminal law and procedure at the University of Queensland) highlighted what she felt was an important omission from the Bill as introduced in failing to address the question of:
...what is to happen where a person who either permanently or temporarily resides in a health or aged care facility requests assisted dying and the facility is owned or managed by a religious institution opposing assisted dying. The Bill should enshrine in detail what is required of those institutions in these cases. Are they required to allow third-parties willing to provide assisted dying access to their facilities? If not, are they required to organise the person’s transport to another facility allowing assisted dying? What is to happen where a person can no longer be transported?
In its written submission, the Christian Medical Fellowship argued that, should assisted dying be legalised, the legislation should specifically include:
an institutional right of conscientious objection, so that individual hospices etc can decide not to provide assisted dying, without risking their funding. If this is not present in draft legislation, it would place an intolerable strain on the ethos of many existing services.
Fraser Sutherland from the Humanist Society Scotland cited the experience of institutional objection in Australia during his evidence to the Committee and argued that allowing institutions to conscientiously object to any involvement in assisted dying would have a detrimental impact on patients:
For example, if a patient is in hospice care and the institution says, “We’re having nothing to do with assisted dying—we won’t even allow people on our premises to do an assessment process”, that has a massive negative impact on patients. They might have to withdraw to their home, which can have an impact on their care.28
When asked if there was any aspect of legislation on assisted dying in Canada she would wish to see changed, Dr Stefanie Green from the Canadian Association of MAiD Assessors and Providers told the Committee:
The only change that I would like to see, if I could wave a magic wand, is a recognition that, although practitioners and other people have conscientious rights, bricks and mortar do not. It is probably not good that tax-funded institutions can choose to opt out of a legally covered MAID [medical assistance in dying] service in Canada, so palliative care facilities should not have the right to opt out. That is certainly the state of affairs in Quebec, and I think that the rest of the country should adopt that policy.35
Vicki Cahill from Alzheimer Scotland was asked to reflect on the impact institutional objection could have on ensuring equitable access to assisted dying:
From an equity and accessibility point of view, that would depend on the spread of objection to the provisions in the legislation and on decisions by organisations not to use the provisions. If the bill is to be enacted, we would need to consider ensuring that there is fair and equitable access for everyone, regardless of where they are. There would be a requirement to look at the spread of access and whether it discriminates against any particular group or community.8
Liam McArthur was similarly unsympathetic to the case for inclusion of a right to institutional objection within the Bill, citing similar concerns:
My problem with an institutional objection is that the organisation in question might well involve and include individuals who are supportive of a change in the law. It then ceases to be about individual choice, because the risk is that barriers can be put in place to individuals who, despite meeting all the eligibility criteria and being protected by the safeguards that are in place, find that, as a result of an institutional opt-out, they are not able to access the choice. We have seen that happen in other jurisdictions, and it has proved problematic.12
The Committee notes a range of views for and against the suggestion that the Bill should include a right to institutional objection. In the event that the general principles of the Bill are agreed to at Stage 1 and irrespective of whatever position the Parliament ultimately takes on the question of allowing institutional objection or not, the Committee notes a widespread view that there is a need for amendments to provide further clarity in the Bill regarding how institutions can reasonably expect to be permitted to act in the context of the Bill's implementation.
Staff training, qualifications and guidance
As described in the Explanatory Notes1, section 23 of the Bill "allows Scottish Ministers to issue guidance regarding the practical operation of the Act". The Explanatory Notes further explain that "Such guidance is expected to be of a practical nature (for example, guidance for individuals witnessing a first declaration, for doctors around the requirement for proof of identity, how the period for reflection is intended to work and other such requirements under the process set out in the Bill)."
Training
One key area that can be expected to be covered by such guidance relates to training of medical professionals.
During his oral evidence to the Committee, Professor Ben White from the Australian Centre for Health Law Research gave an overview of the training his organisation was contracted to design and deliver for practitioners involved in voluntary assisted dying in Queensland, Western Australia and Victoria:
The training varies slightly but globally takes about six hours. The goals are to ensure that all practitioners who are involved in providing voluntary assisted dying understand the eligibility criteria and how the oversight process and reporting would work, and that anyone who is providing voluntary assisted dying has done the training. An assessment component is attached. Anyone who is involved in that process will have that baseline level of knowledge about voluntary assisted dying.2
The Financial Memorandum3 accompanying the Bill estimates the annual cost of staff training associated with its implementation at approximately £200,000. In its written submission, NHS Education for Scotland described this estimate as "unrealistic" and concluded:
Existing training budgets are already under huge pressure and if money needs to be found for assisted dying from existing budgets, then this will result in reduction in funding in other areas. This needs more consideration and exploration of other routes of funding.4
Dr Chris Provan from the Royal College of General Practitioners Scotland agreed with this assessment:
GPs have a lot of experience, as I have said, around capacity and coercion, but this is a specific situation. Costs for continuing professional development and learning from and reflection on how the system has worked are not really reflected.5
Giving evidence to the Committee, the Cabinet Secretary for Health and Social Care referred to the separate assessment the Scottish Government had made of the costs of training the health and care workforce (specifically, doctors) to be able to fulfil the process set out in the Bill, as outlined in the Scottish Government's memorandum to the Committee. The Cabinet Secretary reconfirmed what this assessment had concluded those initial training costs would be:
... if we were to assume that half of all doctors would undergo training, and that the training time would be around seven hours—as is suggested in Mr McArthur’s financial memorandum—there would be a total cost of just over £6 million for training time, which has not been factored in.6
In their written submission, Dr Sandra Lucas and Dr Rhona Winnington from the University of the West of Scotland emphasised the importance of robust and consistent training for all healthcare professionals involved in assisted dying:
This will ensure not only equitable delivery of knowledge, but also that it becomes a legal requirement before any healthcare provider engages in service provision. This acts as a safety net to ensure the service is delivered legally and meets a minimum standard of care. To further support this, specialist and generalist training workshops should be undertaken for those involved in service delivery and those who may engage in conversations about assisted dying. A comprehensive training strategy will help to maintain high standards of care and ensure that all healthcare providers are adequately prepared to support patients through the assisted dying process.7
Hospice UK flagged the importance of ensuring, if assisted dying were to be legalised, that all staff working in hospices were provided with an appropriate level of training:
Regardless of whether or not assisted dying is delivered in any charitable hospice, based on the eligibility criteria proposed in the Bill the vast majority of adults supported by hospices would be eligible to request assisted dying. This means that all staff (and potentially volunteers) working within Scottish hospices would need, at the minimum, further training on:
how requests for assisted dying should be handled
what the process is if a patient wishes to access an assisted death
updates to existing training on how to have difficult conversations
updates to existing training on future care planning8
It concluded:
The development and delivery of any training programme or materials must include staff employed by non-statutory organisations (such as hospices or care homes).8
Giving evidence to the Committee, Liam McArthur sought to downplay the level of additional training health practitioners might require to fulfil their role as part of the process set out in the Bill:
I am reassured that medics make capacity assessments routinely in relation to a swathe of different treatments and care options. Almost certainly, additional training will be required to make a capacity assessment in the context of an assisted dying process, but I would see that as augmenting or adapting the training that registered medical professionals routinely undertake.10
The Committee notes from evidence the critical importance a number of contributors have attributed to the provision of comprehensive training to health practitioners involved in the assisted dying process. It further notes that the costs of training set out in the Financial Memorandum accompanying the Bill are considered by many to be a significant under-estimate. In connection with this, it notes a significant discrepancy between these figures and the separate calculation of training costs provided in the memorandum setting out the Scottish Government's position on the Bill.
The Committee notes that, should the Bill progress to become law, the eventual costs of training could vary significantly according to a number of factors including:
the agreed overall service model; and
the possible inclusion of an 'opt-in' model of participation of health practitioners, including a possible central register
Should the Bill progress to Stage 2, as the agreed delivery model becomes clearer, the Committee would expect the Scottish Government to set out how it intends to meet the associated costs of training in a way that does not negatively affect available funding for existing services.
Qualifications and experience
As the Bill describes, anyone fulfilling the role of "coordinating registered medical practitioner" (section 4 of the Bill) or "independent registered medical practitioner" (section 6 of the Bill) is defined as a registered medical practitioner "who has such qualifications and experience as the Scottish Ministers may by regulations specify".
The Policy Memorandum accompanying the Bill explains the rationale for giving Ministers regulation-making powers in this area as being to "...ensure that if a certain level of experience (for example, that a doctor should have completed foundation year two, or that one of the two doctors should be a specialist in the person’s terminal illness) is considered appropriate that Ministers can require it, thus ensuring that the public and those wishing to access assisted dying can have confidence that the process is carried out in the safest way possible."11
In its written submission, Together for Short Lives argued:
We believe greater clarity is needed in the Bill on the skills, experience and training that a professional should have to make these preliminary assessments and in turn, assist someone to die. The Bill also needs to explicitly state that clear guidelines would be put in place to ensure that the appropriate level of medical expertise would be involved in the decision-making process.12
One anonymous individual raised specific concerns that, according to the Bill as introduced, any fully registered doctor, irrespective of their level of experience, would be permitted to be involved in the process of assisted dying:
This would include FY2 [foundation year 2] doctors who would only have been registered for a year. If this is passed, I would not consider junior doctors, especially those early in their career to be sufficiently qualified to be involved in this process. The doctors should be consultants, or at minimum those who are, for instance, 5 years post full-registration.
Dr Stephen Potts from the Royal College of Psychiatrists in Scotland was asked whether, in his view, FY2 was an adequate level of training and experience to be able to fulfil the registered medical practitioner roles envisaged by the Bill. Dr Potts responded:
As far as the psychiatry role is concerned, we have recommended that the level of expertise should be at least equivalent to that of approved medical practitioner under the 2003 act. Essentially, that is a psychiatrist who has completed their core psychiatric training and has three more years of higher training to go before they become a consultant. It is a middle-grade doctor role, not an FY2 role.13
Reflecting on Dr Potts' evidence, Dr Iain Kennedy from BMA Scotland emphasised his organisation's overarching view that assisted dying should be provided via a separate, stand-alone service but was also supportive of the idea that those medical practitioners involved should be able to demonstrate a relatively high level of seniority and experience:
The BMA’s opinion, of course, is that we believe that there should be a separate, specialised service; therefore, by definition, those doctors would be highly trained in that area. We lean towards the involvement of more senior, highly trained doctors. However, that absolutely needs to be specified.5
Questioned about the lack of detail on the minimum level of qualifications required of medical practitioners, Liam McArthur responded:
As it stands, the bill probably goes as far as it can in expressing who is likely to be involved in this process, but there is an opportunity there. My expectation is that the Government would work with the professional bodies to identify how best to express that through secondary legislation and guidance.10
The Committee notes a range of views regarding the level of qualifications and experience a health practitioner should be able to demonstrate to be involved in assisted dying. It further notes Liam McArthur's view that, should the Bill become law, this issue would be best addressed through the development of secondary legislation, in close consultation with the relevant professional bodies.
The importance of clarity in guidance
While taking evidence on law enforcement considerations related to the Bill, the Committee heard repeated emphasis from witnesses on the need for utmost clarity in guidance to give healthcare professionals confidence that, in following the process set out in the Bill, they were acting within the law and to minimise the likelihood of assisted deaths subsequently having to be investigated. Laura Buchan from the Crown Office and Procurator Fiscal Service told the Committee:
...for the purposes of investigation and consideration, the more clarity people who want to follow the process have, the better, in order to ensure that they are following the right steps and the right process. People—family members and friends, and medical practitioners—should be absolutely clear about the process.
For us, that would mean that, when that death is reported, a limited amount of death investigation needs to be carried out in order to ensure, in a compassionate way, that families can deal with their loss and that investigations can be closed. The risk of not having that clarity is that it potentially opens more deaths up to investigation.6
The Royal College of Nursing Scotland were in agreement that detailed guidance on the precise boundaries of the law would be necessary to protect the staff they represent from potential prosecution:
Given the importance of these issues, and the risk of prosecution, explicit guidance is needed to define where the line lies, in order to protect health professionals as well as to safeguard people accessing an assisted death. This must include a checklist of what can be done lawfully and what is unlawful.17
The Committee highlights evidence that underlines the need for guidance to be suitably clear and comprehensive so that all parties involved have legal certainty over the precise boundaries of the law should assisted dying be legalised.
Coercion
Section 19 of the Bill provides that it is not a crime to provide an eligible person with assistance to end their life, as long as all of the requirements of the Bill are complied with. Similarly, section 20 provides that providing such assistance does not give rise to any civil liability.
Section 21 creates a criminal offence to coerce or pressure a terminally ill adult into making a first or second declaration. Prosecution for this offence under the summary procedure would carry a maximum penalty of two years in prison and/or a fine not exceeding level 5 on the standard scale. The current fine in this context is £5,000. Prosecution under solemn procedure (for more serious offences) would carry a maximum penalty of 14 years in prison and/or an unlimited fine.
The Bill requires that the independent registered medical practitioner (for the first declaration) and coordinating registered medical practitioner (for the first and second declaration) must be satisfied that the declaration has been made without pressure or coercion (sections 6 and 8 respectively). Furthermore, section 15 requires that either the practitioner or health professional is satisfied, at the time the substance is provided, that the person has not been coerced or pressured by any other person into requesting provision of that assistance.
The Committee has heard evidence from a number of different stakeholders who have raised concerns over how coercion would be assessed and managed under the provisions in the Bill. These concerns centred around the following themes:
The definition of coercion;
The model for identifying coercion;
The capacity and skills of healthcare staff to detect coercion; and
Clarity of the offence and its enforcement.
Neither the Bill nor accompanying Policy Memorandum specify how a healthcare professional should undertake assessment of coercion. The Bill states that a person commits an offence if they coerce or pressure a terminally ill adult into making a first or second declaration and the same wording is replicated in schedules 1, 2 and 3 on the forms to be used to record declarations to that effect. The Explanatory Notes make reference to the General Medical Council guidance on decision making and consent, which contains a section entitled 'If you're concerned a patient can't make a decision freely' and provides the following definition of what this means:
coerced (i.e. forced) or being pressured (i.e. to be subject to psychological and/or moral pressure).1
Throughout the Committee's Stage 1 scrutiny, certain contributors expressed concerns about the definition of coercion. One respondent to the Committee's call for views summarised these concerns as being that, in their view, coercion was "in reality multi-faceted, often subtle in nature and therefore cannot be assessed."2 Witnesses giving evidence to the Committee were in general agreement that overt, explicit attempts by an individual to pressure someone to go against their wishes or preferences may be relatively easy to identify. However, certain witnesses expressed concerns that there were a range of factors, internalised and societal that could also result in an individual's decision to request assisted dying being subject to undue influence. Vicki Cahill, speaking in relation to people living with Alzheimer's and dementia, told the Committee:
...we should look at it much more widely in terms of undue pressure that might come from elsewhere and influence an individual’s decision to seek an assisted death. Examples are the perception of being a burden or being stigmatised or discriminated against in day-to-day living, and someone’s experiences of health and social care or social interactions might make them feel that their life is or is not worth living.3
Dr Chris Provan was one among many witnesses who expressed concerns about the potential risk of internalised coercion. He argued that detecting these more subtle forms of coercion could be better achieved via a centralised service as an alternative to the model proposed in the Bill:
Sometimes, coercion is quite subtle—somebody might not feel that they are under coercion but just that they are a financial burden to their family or something like that, which is quite difficult to detect. There are concerns around vulnerable patients in that type of situation, which is why we think that there should be a centralised service, with excellent training and support for a team assessing each patient.4
Dr Stephen Potts from the Royal College of Psychiatrists in Scotland expressed a similar view and, as an approach the current Bill could potentially follow, pointed to the model of independent assessors who are responsible for assessing possible coercion of living donors under the Human Tissue Act 2004:
In the field of human organ donation, the relevant regulatory body is the Human Tissue Authority, whose system requires explicit assessment of possible coercion applied to living donors. It provides independent assessors to each transplant unit, oversees them and provides training. This sort of thing can be done, and it has been done by a UK regulatory body for the past 18 years.5
He went on to argue that this model had also shown itself, in his own experience, to be effective in detecting cases of internalised coercion:
...there is a duty to explicitly assess coercion on somebody who has come forward as a potential living donor of an organ. I have seen 100 or more such cases, and only in two or three have I identified explicit coercion and the transplant has not gone ahead. In a larger, though still small, number, I have identified internal pressure or a sense of duty or obligation as the potential donor’s reason to donate, and the transplant has not gone ahead. We are talking about small numbers, but I am more concerned about internal duty and obligation than I am about external pressure in that context, and I would apply the same to this context, too.5
Professor Gareth Morgan from the Scottish Christian Forum on Assisted Dying expressed an alternative view that internalised coercion in this context was different to other situations. He argued that, in his view, an internal sense of duty or obligation would, in practice, be a very unlikely primary motivation for someone to seek to request assisted dying or to go through the entire assisted dying process:
...it seems unlikely that anybody would go right through the assisted dying process purely for that reason, especially when you consider the requirements for there to be a first declaration, meetings with two doctors, a second declaration and then a decision at the point at which they are provided with the substance that will end their life. I find it impossible to think that anybody would go through all those steps primarily because of their sense of being a burden. Surely, they will be choosing those options because of the much bigger issues about all that they are going through in the dying process.7
A number of stakeholders expressed concerns around the capacity and capability of healthcare staff to be able to detect coercion. In its written submission, the Royal College of General Practitioners Scotland challenged the assumption that any discussion of assisted dying could take place as part of a regular GP appointment:
This is a complex process, morally and emotionally, involving considerable time for technical assessment of capacity and coercion which can be challenging. We do not believe that this work can or should be incorporated into an already very busy and stressed service, without potential detriment to patient care and significant emotional, psychological and ethical pressure on GPs.8
During oral evidence, Dr Chris Provan reinforced this view, arguing that GPs would not have the capacity to be able to detect coercion in every circumstance and re-iterated his view that this would be better done as part of a separate, stand-alone service:
They [GPs] do not have the time or headspace to be able to do that in the current model. A centralised model in which independent doctors or a team assess the patient would partly help. In some situations, coercion will be obvious, and we are trained in adult support and protection, but that is a complex, time-consuming area.4
Marianne Scobie, representing the Glasgow Centre for Inclusive Living, argued that current difficulties with accessing GPs, particularly for disabled people, would make it difficult for those GPs to know their patients well enough to be able to detect coercion:
One of the issues arising from the bill is about people seeing their GP. People struggle to see their GP. They struggled to see their GP before the pandemic, and they struggle even more to see them now... Many disabled people have not been able to see their GP for some years. Even now, they are not able to see a GP even when they are quite ill... How would they know whether there is any coercion in the patient’s family? How would they know whether there is any coercive control going on in a person’s particular situation?3
Stephanie Fraser from Cerebral Palsy Scotland raised a similar concern, questioning whether a GP or other medical practitioner was necessarily the best person to assess coercion. In the context of providing care and support for people with Cerebral Palsy, she argued that there should be provision in the Bill that stipulates how long a healthcare professional would need to have known the person, and their family, before they could be considered capable of assessing capacity and coercion3. Dr Gillian MacDougall from Friends at the End argued that, in carrying out an assessment of coercion, it would be important for the assessing healthcare professional to see a person on their own as well as seeing them together with loved ones or people who are important to them.7
Certain respondents to the call for views argued that doctors were not necessarily the best placed category of professionals to assess coercion. They called for the involvement of other professionals, such as councillors, social workers or other healthcare professionals in assessing coercion. Dr Gillian Wright from Our Duty of Care commented: "Generally, doctors are not trained specifically to detect coercion" and went on to argue that social workers were far more used to doing so as part of their practice.7 Dr Iain Kennedy from the British Medical Association Scotland acknowledged that doctors do have some prior experience of assessing coercion but suggested that, in the case of assisted dying, additional training would be necessary:
Doctors already have experience of identifying coercion—for example, in situations in which families might want us to start or stop treatment. However, we feel that coercion is an area that requires specialist training in relation to the provision of any new service.4
Many contributors called for better training around coercion in both written and oral evidence. The Committee took evidence from witnesses in Victoria, Australia on how coercion is assessed in that jurisdiction. Professor Ben White from the Australian Centre for Health Law Research told the Committee that, under their model of assisted dying:
A specific component is focused on training doctors in detecting coercion and in the sorts of conversations to have.15
Katherine Waller, also from the Australian Centre for Health Law Research, who has managed the delivery of training programmes for assisted dying in Victoria, Western Australia and Queensland, explained that the training is delivered via e-Learning modules, which can be completed in 6 hours. When asked how coercion is assessed and how it is addressed in the mandatory training, Ms Waller responded:
The mandatory training covers the eligibility criteria, including coercion, extensively. Relevant training content includes:
guidance on how to assess coercion, including questions to ask the patient and family members/carers to help detect coercion;
links to screening tools and studies;
learning activities such as case studies and multiple-choice questions, to reinforce learning.16
While considering the law enforcement implications of the Bill, witnesses representing Police Scotland and the Crown Office and Procurator Fiscal Service raised concerns about how the offence of coercion set out in the Bill would be enforced. In its written submission, Police Scotland highlighted a number of factors it would consider important when undertaking a police investigation into an alleged offence. In relation to coercion, these included:
clarity on how the coordinating doctor should assess that a declaration was made voluntarily and free from coercion;
no requirement for the coordinating doctor to involve any other agencies when assessing coercion or abuse; and
clarity on whether the doctor or nurse should be in the same room as the person or not when they die and whether other people can be present with the person when they die.17
Dr Gordon MacDonald from Care Not Killing argued that, in his view, coercion was not only hard to detect but also hard to prosecute. He criticised what he considered to be the 'tick box' or bureaucratic approach to assessing coercion set out in schedules 1, 2 and 3 of the Bill and argued for clearer processes and safeguards to be put in place to ensure a more thorough assessment. One of the respondents to the Committee's written call for views took a similar view, arguing that, based on experience with abortion law, the approach to assessment of coercion would be devalued over time:
Examination by two doctors was a safeguard in abortion legislation, but is well recognised to have become a mere tick-box exercise. What will stop this following a similar path?2
Laura Buchan from the Crown Office and Procurator Fiscal Service was clear that it would only be possible for an offence of coercion as set out in the Bill to have been committed while the individual requesting assistance to end their life was alive and going through the assisted dying process:
My understanding of the bill is that there is an offence of coercion during the process, so somebody could be reported for coercion if it was raised by one of the medical practitioners at any stage of the process or declarations. However, if it was raised after the person had died, that would potentially take it outwith the process and open the opportunity for a homicide investigation.19
Laura Buchan went on to outline some of the additional complexities associated with investigating a case of alleged coercion under the Bill and emphasised the need for absolute clarity around definitions and processes:
It is also not clear in the bill how, if the medical practitioner has any concerns about coercion, those concerns might be raised with the relevant authorities. There might also be scope for disagreement among practitioners about whether there is coercion. One of our observations is therefore about clarity around what we mean by coercion and pressure, how a medical practitioner would determine whether there was coercion and pressure, and how they would intimate that there had been coercion and pressure in the process so that that could be considered. There is no offence of coercion in Scots law. It is more ordinarily discussed in the context of defences. Much of our consideration would depend on whether the coercion came to light during the process or was raised by another person after the process had been completed.19
Assistant Chief Constable Steve Johnson supported this view and explained why it would be important for healthcare professionals to receive clear guidance on assessing coercion, in the event that a case was subsequently referred to the police for an investigation:
The co-ordinating registered medical practitioner and the independent registered medical practitioner are asked, at point 2 in the statement forms, to declare that, to the best of their knowledge, there has been no coercion, but how do they know that that is the case? What was the nature of their inquiries? What questions did they ask the individual who is in front of them about whether there has been a broad conversation between interested parties in their family, for example? We are therefore keen for there to be clear guidelines for medical practitioners about how they come to the conclusion that there has been no coercion or pressure.19
The Committee subsequently explored the scenario of the police having to deal with a potentially vexatious claim of coercion from a family member, who may be a member of the individual's extended family or a distant relative and is opposed to assisted dying, after the death of the individual in question had taken place. In such circumstances, Assistant Chief Constable Johnson argued that clear guidance for practitioners could help to avoid Police Scotland having to initiate a murder or culpable homicide investigation with the involvement of a family group that would already have been traumatised by the recent passing of a loved one. He described how this could work in practice:
We seek clarity on how two medical practitioners could sign statements to say, “We believe that no coercion or pressure has knowingly been put on that person”, and which would stand scrutiny by the Crown and ourselves so that the case would not be referred for police investigation. The practitioners would have to have the full protection of the law saying that they have followed the rules on assisted dying, with clear guidance for medical practitioners on how to determine that there has been no coercion or pressure. That point is, if you like, a clear-cut ending to the process. We are concerned that without that clarity, people might end up in really challenging situations with a full police investigation into circumstances that the bill could have addressed before being enacted.19
Reflecting on evidence taken by the Committee, Liam McArthur highlighted existing guidance for healthcare professionals on assessing coercion but acknowledged that this may need to be revised and expanded if the Bill were to become law:
There is probably an argument for adapting the training that medics receive to reflect the context in which those assessments would be undertaken. However, the General Medical Council has set out very clear guidance on how to assess whether coercion is taking place. It has also set out very clear guidance on assessing domestic abuse and controlling or coercive behaviour. Therefore, guidance is already in place, but I accept that it might need to be reviewed and an assessment made of whether changes are required, given the change in the law that the bill would introduce.23
When asked about the scenario of dealing with requests for the police to investigate an assisted death on the basis of potentially vexatious claims of coercion from family members opposed to assisted dying, Mr McArthur told the Committee:
...there is probably no way to prevent an individual from bringing a legal challenge, but the mechanisms in the bill provide a high level of protection against such cases arising. Challenges tend to come from family members who have a difficulty with the decision that their relative has made. Conscientious objection exists in the medical profession and we can put that into the bill, but we cannot put into the bill protections for family members who are implacably opposed to the option and who therefore might have difficulty with a relative opting to go down that route.23
The Committee has heard evidence of a range of concerns on the provisions of the Bill related to coercion, including the definition of coercion, the process for assessing coercion, the capacity and capability of healthcare professionals to be able to assess coercion and enforcement of the offence of coercion as set out in the Bill.
In relation to the definition of coercion, the Committee notes the existence of extensive guidance from the General Medical Council. It further notes a general consensus amongst expert witnesses that cases of explicit coercive behaviour should be relatively straightforward to detect. At the same time, it has heard concerns that other cases may be considerably more subtle and the associated assessment requirements may be correspondingly time-consuming and complex.
The Committee has heard interesting evidence of potential alternative models for assessing coercion such as the system of independent assessors responsible for assessing potential cases of coercion of living donors under the Human Tissue Act 2004. It notes related evidence that this model has proven effective in detecting cases of internalised coercion as well as more straightforward and explicit incidences. Should the Bill progress beyond Stage 1, the Committee notes it may be beneficial to explore further via amendments whether a similar model could be successfully applied to the assessment of coercion under the current Bill.
On the issue of training, the Committee has heard evidence from professional bodies which emphasises the need for tailored training on assessing coercion to be developed and provided to health practitioners should the Bill become law. In this context, it notes evidence from Australia which highlights existing training on assessing coercion that could be useful to learn from.
The Committee also recognises the importance of clear and robust guidance to ensure police resources are appropriately targeted towards cases where there is credible evidence that coercion may have taken place.
The Committee therefore welcomes the preparedness of Liam McArthur to consider further how existing guidance can be reviewed and updated to ensure health practitioners receive the tailored guidance and training they need to be able to assess coercion effectively and to allow the offence created by section 21 of the Bill to be appropriately policed.
Limitations on effect of Act
Overview of section 22 of the Bill (limitation of effect)
The Bill as introduced has been drafted in acknowledgement that the implementation of certain of its provisions could be outwith devolved competence. Section 22 states that the relevant provisions in the Bill – or in secondary legislation made under it – insofar as they relate to specified reserved matters, will have no effect. The specified reserved matters are:
misuse of drugs (Head B1 of Schedule 5 to the Scotland Act 1998);
regulation of the health professions (Head G2); and
medicines, medical supplies and poisons (Head J4).
The limits to devolved competence
The Scotland Act 1998 sets out the parameters within which the Scottish Parliament and the Scottish Government can act. There are two types of devolved competence - legislative competence (the power of the Scottish Parliament to pass legislation) and executive competence (the power of the Scottish Government to take executive action, such as making regulations).
Legislation or executive action which is outwith devolved competence has no legal effect. This means it can be challenged in court, even many years after the legislation was passed.
One of the factors to be considered in determining whether a certain activity is within devolved competence is whether it relates to reserved matters. These matters are those areas for which only the UK Parliament can legislate. The list of reserved matters is set out in Schedule 5 to the Scotland Act 1998. Broadly, if a subject matter is not specifically reserved, then (subject to the other restrictions on competence), it is within the devolved competence of the Scottish Parliament and Government.
There have been competing views over the legislative competence of this Bill. Both the Presiding Officer of the Scottish Parliament and Liam McArthur have issued statements outlining their views that the Bill is within the legislative competence of the Scottish Parliament.1
However, the Scottish Government’s Memorandum on the Bill2 sets out its view that the Bill is outwith the legislative competence of the Scottish Parliament. This position was confirmed by the Cabinet Secretary for Health and Social Care when he gave evidence to the Committee.3
It is ultimately up to the courts to determine whether legislation passed by the Scottish Parliament or executive action by the Scottish Government is within devolved competence.
Sections of the Bill which may raise competence issues
Several sections of the Bill have been identified by stakeholders as raising potential competence issues. These are:
Section 15(8), which would give Scottish Ministers a regulation-making power to specify an approved substance to be used to end the lives of those accessing assisted dying – this may engage with the reserved matters of misuse of drugs and medicines, medical supplies and poisons. Without further action, this reservation may prevent the Scottish Ministers from designating a substance to be used to end the lives of those accessing assisted dying. Liam McArthur acknowledges this as a “likely” issue at paragraph 8 of the Policy Memorandum.4
Section 18(1) of the Bill, which provides for a conscientious objection clause – this may engage with the reserved matter of regulation of the health professions. If it does, then further action would be necessary to make the conscientious objection clause in the Bill effective.
Section 4(5)(a) – regulations on qualifications and experience for doctors – and section 7(2)(c) requiring doctors involved in assessing patients for assisted dying to “take account of” any second opinion – this may engage the reserved matter of regulation of the health professions, although the only stakeholder to raise concerns about this was the Scottish Government. If these provisions do relate to reserved matters, then further action would be needed to make them effective.
Liam McArthur has highlighted a number of potential options to deal with issues which may be beyond devolved competence. These are discussed in more detail in paragraphs 8 to 10 of the Policy Memorandum.4 In summary, they are:
a “section 30” order under the Scotland Act 1998 – which could be used to alter the legislative competence of the Scottish Parliament
a “section 63” order under the Scotland Act 1998 – which could be used to transfer functions of UK Government Ministers to the Scottish Ministers. This could enable the Scottish Government to make regulations in currently reserved areas
a “section 104” order under the Scotland Act 1998 – which could be used by the UK Government to make consequential changes to reserved areas of law as a result of Scottish Parliament (or Scottish Government) legislation
use by the UK Government of existing powers – e.g. designating a particular substance as appropriate for using in assisted dying under existing medicines and poisons legislation.
Each of these options would require action by the Scottish or UK Governments - or both - to progress. Contributors to the Committee's scrutiny of the Bill have pointed out that this may result in delays to the Bill, if passed, while the necessary discussions take place. Some have further argued that, without the support of both governments, it may not be possible to put a system of assisted dying in place in practice.
Views on the impact of competence issues on the Bill
In oral evidence to the Committee, the Cabinet Secretary confirmed the Scottish Government’s view that the Bill in its current form is outwith the legislative competence of the Scottish Parliament.1 The reasons for this view are explained in the Scottish Government's Memorandum on the Bill.2
Dr Mary Neal, from the University of Strathclyde, highlighted what she considered to be the significant impacts of competence issues on the practical implementation of the Bill. She raised concerns about the designation of an approved substance to be used by those accessing assisted dying, which section 15(8) of the Bill would make provision for the Scottish Government to do via regulations:
The medicines issue—that the Scottish ministers are able to approve a substance—is fundamental to the whole bill. If that cannot happen, it is difficult to see how the bill, or a system of assisted dying in Scotland, can go ahead.3
Dr Neal also expressed competence-related concerns about section 18 of the Bill, which would make provision for conscientious objection by health professionals:
When the bill was published, it really concerned me that, although it contains the conscience clause—presumably to provide reassurance to the medical professions that there is a will to protect them—nothing is said in the policy memorandum or the explanatory notes to flag up that, as things stand, section 18 would be completely ineffective, additional permission would be needed, and section 22 would kill the conscience clause if the permission was not forthcoming.3
Liam McArthur also acknowledged competence-related issues which would need to be addressed for the Bill to take full effect:
Although the Presiding Officer has deemed the bill to be competent in the context of the Scottish Parliament’s powers, I have always acknowledged that putting in place a fully functioning process of assisted dying in Scotland will require matters that are the preserve of Westminster to be addressed, in particular in relation to medicines, the Misuse of Drugs Act 1971 and so on.
However, as the committee heard on numerous occasions last week from Mr Gray, those matters can be resolved only at the point at which the Scottish Parliament decides that a change in the law is required.5
He explained his thinking in developing the Bill in this way:
From the outset, I was very conscious that I did not want to use the bill as a mechanism to push the boundaries of constitutional arrangements, so... ...I have operated in that framework.5
Some witnesses argued that the competence issues identified could be dealt with provided there was a will from the relevant parties to do so. Lynda Towers from the Law Society of Scotland said:
If there was a desire and willingness to sort out those devolved/reserved issues, there is nothing to say that that could not be done. However, it would require the United Kingdom Government to be willing to give whatever consents were necessary in whatever form. My caveat is that those things take time, whether they would form part of a bigger package or be designed solely to deal with the bill. It would also require a degree of agreement with the Scottish Government in order to make whatever approaches were necessary.3
Liam McArthur also indicated he was "confident" that the necessary mechanisms were available to enable any competence issues to be resolved:
Given that a very similar bill is going through the Westminster Parliament, coincidentally at the same time as the bill that we are considering, I think that that enhances the opportunities to ensure that relatively speedy progress can be made in this area once the Scottish Parliament decides whether it is supportive of the general principles, in support of a change in the law.5
In his evidence to the Committee, the Cabinet Secretary said:
I recognise that Mr McArthur has sought to propose options. Should the bill pass stage 1, we would look at what options might work.1
The Committee notes the potentially significant impact the current boundaries of devolved competence could have on the practical implementation of the Bill should it progress to become law. It recognises that Liam McArthur has acknowledged these challenges and has proposed a number of potential solutions. It welcomes the commitment from the Scottish Government, should the Bill progress beyond Stage 1, to open dialogue with the UK Government with a view to resolving these competence-related issues. In this event, the Committee calls on the UK Government to take a similarly constructive approach, and on the Scottish Government to keep the Parliament regularly updated on progress.
Provision of information, reporting and review
Overview of the information, reporting and review requirements in the Bill
Sections 24 to 27 of the Bill make provision for the collection of information and set out reporting and review requirements.
Section 24 would place a requirement on Public Health Scotland to report annually to Scottish Ministers in relation to those accessing assisted dying. The report would include information on the number of people requesting access to each stage of the assisted dying process, as well as the number of people who were assessed as ineligible.
In addition, information about the reasons for progressing - or not progressing - with assisted dying would require to be reported. Finally, information about the individual characteristics of people requesting access to assisted dying, such as ethnicity, postcode district and type of terminal illness would also be collected. Scottish Ministers would be able to change the nature of the information collected via regulations.
Section 25 would give Scottish Ministers a regulation-making power to require information to be supplied to Public Health Scotland for the purpose of reporting on implementation of the Bill. This would include the power to create a criminal offence relating to wider disclosure of information in circumstances where this was prohibited.
Section 26 would require Scottish Ministers to lay before the Scottish Parliament an annual report on the provision of assisted dying under the Bill. This would be required to include the information collated by Public Health Scotland on access to assisted dying and could also include other information.
Section 27 would require Scottish Ministers to publish a review of the operation of the legislation after five years. The report would cover:
the extent to which the legislation had been successful in supporting assisted dying;
any concerns raised about the operation of the legislation; and
Scottish Ministers’ response to any concerns, including any recommendations for change.
Views on the information, reporting and review provisions
Respondents to the detailed call for views generally saw the information, reporting and review provisions as an important safeguard against abuse, as well as a tool for building public confidence in the process. Broadly, the view was that they should be as transparent and robust as possible.
Key themes in evidence included that there should be an independent body to oversee monitoring and implementation; that a five year period before undertaking a review of the legislation was too long; and that additional information, beyond what was stipulated in the Bill, should be collected. Suggestions for additional information to be collected included the following:
incidence of complications and adverse events;
impact on staff and relatives;
data on protected characteristics;
socio-demographic information;
data on who is involved in assisted dying and their qualifications;
cases involving psychiatric assessment; and
cost savings and expenses incurred.
Categories of data being collected
Marianne Scobie, representing Glasgow Centre for Inclusive Living, highlighted some of the concerns the disabled people her organisation represents had about data collection:
Under the bill as drafted, there would be no record of socioeconomic elements, such as whether someone had financial difficulties prior to when they sought support and services; similarly, social care or palliative care elements or what their main reason was in opting for assisted dying would not be recorded. Our main concern is that there would [be] no monitoring or reporting of whether the person had had a mental health assessment, or any counselling or support, before they made the decision to go ahead with the decision to end their life.1
However, Liam McArthur confirmed that Scottish Ministers would have the power under section 24 of the Bill to adjust what information was being collected but also emphasised the importance of being clear why any additional information was being collected given the associated resource implications:
...if the Government or stakeholders that are informing the Government feel that other elements need to be added, there is a mechanism for doing that. As with any data gathering, there needs to be an understanding of why something is being added to the list. Such processes are not without time and cost implications, so we need to understand the purpose for which we are gathering data.2
Processes for collecting information
Several respondents to the call for views argued that the forms provided in the schedules to the Bill (relating to making declarations, co-ordinating and independent doctors’ statements and final statements) appeared to them quite basic and, as such, did not provide the means to collect the information required in the monitoring provisions of the Bill. Although the Scottish Government would have regulation-making powers to put other systems in place to collect information for reporting and review, this could add additional bureaucracy to the process.
Lynda Towers from the Law Society of Scotland argued:
... given the nature of the evidence from the forms that are before us, it might be very difficult to see what additional factors are put into particular reports and what the deciding factors are.3
A lack of detail in the forms provided in the schedules prompted others to raise concerns that there was a lack of clarity regarding the steps any of the participants would have gone through to ensure the requirements of the assisted dying process had been properly met. In its response to the call for views, Edinburgh Napier University Centre for Mental Health Practice, Policy and Law Research stated:
The forms set out in the Schedules do not even rise to the standard of ‘box-ticking,’ in that all the relevant text is pre-completed, with only names, addresses, signatures and the name of the illness to be added. Given the gravity of the decision, we would wish to see a more individualised statement of how practitioners satisfied themselves as to the relevant issues in each individual case.4
The Law Society of Scotland expressed similar concerns in its response:
We also note that there is no requirement for the relevant practitioner to provide any reasoning or evidence on the form to justify their view that the requirements are met. It is accepted that there may be issues of patient confidentiality but there is no other way to be satisfied that the requirements are met if not included in the form, if there is any challenge to the process.5
Timeframe for review
As highlighted above, some contributors to the Committee's scrutiny expressed concern that the five-year timescale for reviewing the legislation once enacted was, in their view, too long. Marianne Scobie from the Glasgow Centre for Inclusive Living told the Committee:
There is no independent review body in relation to how the bill has been implemented from the beginning, so waiting for five years before anything is reviewed would seem to be rather a long time.1
The Law Society of Scotland also raised the possibility of introducing a 'sunset clause' to the Bill as a means of ensuring adequate scrutiny of its implementation and of developing practice if the Bill became law. This would mean that the legislation would automatically expire after a defined period of time, unless the Scottish Parliament were to vote for it to continue. Lynda Towers from the Law Society of Scotland explained:
…if you have a sunset clause, you will have to have a further debate in the Parliament. You will also have to take into account what has been happening, which would obviously involve looking at cases, how things have worked and all the rest of it.3
Liam McArthur explained his rationale for choosing five years as the time period for the operation of the legislation to be reviewed, arguing that the low numbers likely to take up assisted dying during the first years if the Bill were to become law would make producing sufficient meaningful data in a shorter review period challenging:
I understand why there may be a desire to ensure that any changes that might be needed can be taken account of as quickly as possible. However, if we do not have a detailed data set on which to draw, we, as parliamentarians, will find it more difficult to make a decision, informed by those in the field, about how the legislation is working and whether and where amendments might be required.
A five-year review seems to me to strike the right balance in order to give us the data set while ensuring that there is an annual reporting system in place that can pick up things in real time.2
The Committee has heard concerns that the forms provided in the schedules to the Bill lack sufficient detail regarding the categories of information to be collected to inform the five-year review of the legislation and, importantly, to be able to ascertain what steps have been taken by key participants to ensure the process set out in the Bill has been properly followed. It concludes that this is a matter that would merit further consideration, should the Bill progress beyond Stage 1, to determine what further detail should be included in those forms.
The Committee notes evidence advocating for a range of additional information beyond that provided by the Bill as introduced to be collected as part of the review process. If the Bill progresses beyond Stage 1, it recognises that, should a requirement for additional categories of information be added to the Bill, it will be important to be clear for what purpose this information is being sought and to ensure such additions are directly relevant to the review process.
The Committee has heard a range of evidence on the proposed review period for the legislation. As Liam McArthur has pointed out, it recognises the importance of allowing sufficient time for a useful volume of data to be collected to help reach an informed view as to how the legislation is operating in practice and any amendments that may subsequently be required. The Committee further notes that, although the Bill makes provision for a review to take place after five years after section 1 of the Bill comes into force, it would be possible for the review to be initiated at an earlier point in time if that was deemed necessary.
As an alternative approach, the Committee has also heard the case being made that the Bill could include a 'sunset clause', meaning that it could not continue to remain in force beyond a defined period of time without a further vote in Parliament. The Committee concludes that this may be an area that is subject to amendment and further debate should the Bill progress to Stage 2.
Concluding recommendations
The Committee recognises the thoughtful and considered way in which Liam McArthur has gone about preparing this Bill, given the complex issues it raises and the strength of feeling it provokes, on all sides of the debate.
The Committee acknowledges the equally considered and respectful way in which individuals and organisations have contributed to its scrutiny of the Bill at Stage 1, whether they are supportive of or opposed to the Bill - or take no position.
The Committee wishes to highlight the range of evidence it has heard, as set out in this report. It hopes this will be helpful to individual members in reaching their own decision on the general principles of the Bill and, should the Bill progress beyond Stage 1, informing further detailed scrutiny of the Bill at Stage 2.
In conclusion, given broad recognition across the Parliament that the proposed legalisation of assisted dying is a matter of conscience, the Committee has chosen to make no overall recommendation to the Parliament concerning the general principles of the Bill.
Annexe A: Extracts from Committee minutes
This annexe sets out relevant extracts from the minutes of the Health, Social Care and Sport Committee throughout the inquiry. Each main heading links to a web-page that gives access to:
the agenda and public papers for the meeting
the Official Report of the meeting (public business only), and
minutes of the meeting.
16th Meeting, 2024 (Session 6), Tuesday 21 May 2024
Assisted Dying for Terminally Ill Adults (Scotland) Bill (in private): The Committee considered its approach to the scrutiny of the Bill at Stage 1. The Committee agreed to issue a call for written evidence on the Bill, and to consider the draft Stage 1 report on the Bill in private.
25th Meeting, 2024 (Session 6), Tuesday, 24 September 2024
Assisted Dying for Terminally Ill Adults (Scotland) Bill (in private): The Committee considered its approach to the scrutiny of the Bill at Stage 1. The Committee agreed to consider a revised approach at its next meeting.
26th Meeting, 2024 (Session 6), Tuesday, 1 October 2024
Assisted Dying for Terminally Ill Adults (Scotland) Bill (in private): The Committee considered and agreed a revised approach to the scrutiny of the Bill at Stage 1.
29th Meeting, 2024 (Session 6), Tuesday, 5 November 2024
Assisted Dying for Terminally Ill Adults (Scotland) Bill: The Committee took evidence on the Bill at Stage 1 from -
Julian Gardner AM, Chairperson, Voluntary Assisted Dying Review Board, Victoria, Australia; Ben White, Professor of End-of-Life Law and Regulation, The Australian Centre for Health Law Research
30th Meeting, 2024 (Session 6), Monday, 11 November 2024
Assisted Dying for Terminally Ill Adults (Scotland) Bill: The Committee took evidence on the Bill at Stage 1 from—
Dr Stefanie Green, Founding President of the Canadian Association of MAiD Assessors and Providers and Adviser to the British Columbia Ministry of Health; Dr Ramona Coelho, Physician and Member of the Medical Assistance in Dying Death Review Committee of Ontario, Canada
31st Meeting, 2024 (Session 6), Tuesday, 12 November 2024
Assisted Dying for Terminally Ill Adults (Scotland) Bill: The Committee took evidence on the Bill at Stage 1 from—
Eleanor Deeming, Legal Officer, Scottish Human Rights Commission; Dr Murray Earle, Lecturer in Medical Law, Mason Institute for Medicine, Life Sciences and the Law, University of Edinburgh; Dr Mary Neal, Reader in Law, Strathclyde University; Lynda Towers, Public Policy Committee Member, Law Society of Scotland;
and then from—Dr Stephen Potts, Consultant in Liaison Psychiatry, NHS Lothian, representing the Royal College of Psychiatrists in Scotland; Professor Colin McKay, Professor, Centre for Mental Health Practice, Policy and Law Research, Edinburgh Napier University.
33rd Meeting, 2024 (Session 6), Tuesday, 19 November 2024
Assisted Dying for Terminally Ill Adults (Scotland) Bill: The Committee took evidence on the Bill at Stage 1 from—
Dr Iain Kennedy, Chair of Scottish Council, BMA Scotland; Fiona McIntyre, Policy and Practice Lead, Scotland, Royal Pharmaceutical Society; Colin Poolman, Executive Director, Royal College of Nursing Scotland; Dr Chris Provan, Chair, Royal College of General Practitioners Scotland;
and then from—Amy Dalrymple, Associate Director of Policy and Public Affairs, Marie Curie Scotland; Mark Hazelwood, Chief Executive, Scottish Partnership for Palliative Care; Dr Sarah Mills, Lecturer in Academic General Practice, University of St Andrews; Rami Okasha, Chief Executive Officer, Children's Hospices Across Scotland (CHAS).
1st Meeting, 2025 (Session 6), Tuesday, 14 January 2025
Assisted Dying for Terminally Ill Adults (Scotland) Bill: The Committee took evidence on the Bill at Stage 1 from—
Vicki Cahill, Policy and Public Affairs Lead, Alzheimer Scotland; Susan Webster, Head of Policy and Campaigns, MND Scotland; Stephanie Fraser, Chief Executive, Cerebral Palsy Scotland;
and then from—Tressa Burke, Chief Executive Officer, Glasgow Disability Alliance; Lyn Pornaro, Chief Executive Officer, Disability Equality Scotland; Marianne Scobie, representing the Glasgow Centre for Inclusive Living.
2nd Meeting, 2025 (Session 6), Tuesday, 21 January 2025
Assisted Dying for Terminally Ill Adults (Scotland) Bill: The Committee took evidence on the Bill at Stage 1 from—
Fraser Sutherland, Chief Executive Officer, Humanist Society of Scotland; Dr Gillian MacDougall, Trustee, Friends at the End; Professor Gareth Morgan, Convenor, Scottish Christian Forum on Assisted Dying; Alyson Thomson, Director, Dignity in Dying Scotland;
and then from—Dr Miro Griffiths, Disability Studies Scholar at the University of Leeds, representing Not Dead Yet UK; Gordon Macdonald, Chief Executive Officer, Care Not Killing; Michael Veitch, Scotland Policy Officer, CARE; Dr Gillian Wright, Director, Our Duty of Care.
3rd Meeting, 2025 (Session 6), Tuesday, 28 January 2025
Assisted Dying for Terminally Ill Adults (Scotland) Bill: The Committee took evidence on the Bill at Stage 1 from—
Laura Buchan, Policy and Engagement and Andy Shanks, Head of the Scottish Fatalities Investigation Unit, Crown Office and Procurator Fiscal Service; Steve Johnson, Assistant Chief Constable, Police Scotland;
and then from—Neil Gray, Cabinet Secretary for Health and Social Care, Ailsa Garland, Principal Legal Officer, Nicki Crossan, Assisted Dying Shadow Bill Team Leader, Neil Ritchie, Palliative Care Unit Head and Jo Swanson, Healthcare Quality and Improvement Divisional Head, Scottish Government.
4th Meeting, 2025 (Session 6), Tuesday, 4 February 2025
Assisted Dying for Terminally Ill Adults (Scotland) Bill: The Committee took evidence from—
Liam McArthur, Member in Charge of the Bill, Nick Hawthorne, Senior Clerk, Non-Government Bills Unit and Claudia Bennett, Senior Solicitor, Scottish Parliament; Dr Amanda Ward, Advisor to Liam McArthur.
10th Meeting, 2025 (Session 6), Tuesday, 25 March 2025
Assisted Dying for Terminally Ill Adults (Scotland) Bill: The Committee considered written testimonies on the Bill received from individuals living with a terminal illness.
12th Meeting, 2025 (Session 6), Tuesday, 22 April 2025
Assisted Dying for Terminally Ill Adults (Scotland) Bill (In Private): The Committee considered a draft Stage 1 Report report. Subject to one minor change, the report was agreed for publication. The Committee delegated to the Convener responsibility for finalising the change required.
Annexe B: Evidence and information gathered
This annexe provides links to:
oral evidence taken (links to the Official Report of relevant meetings), together with associated written submissions and follow-up correspondence;
other written submissions;
other correspondence;
notes of engagement; and
SPICe briefings and blogs.
Oral evidence (and associated submissions and correspondence)
Alzheimer Scotland
BMA Scotland
Care Not Killing
Centre for Mental Health Practice, Policy and Law Research (Edinburgh Napier University)
Cerebral Palsy Scotland
Children's Hospices Across Scotland
Christian Action Research And Education (CARE)
Coelho, Dr Ramona (Medical Assistance in Dying Death Review Committee of Ontario, Canada)
Crown Office and Procurator Fiscal Service
Dignity in Dying Scotland
Disability Equality Scotland
Friends at the End
Gardner AM, Julian (Voluntary Assisted Dying Review Board, Victoria, Australia)
Glasgow Centre for Inclusive Living
Glasgow Disability Alliance
Green, Dr Stefanie (Canadian Association of MAiD Assessors and Providers and Adviser to the British Columbia Ministry of Health)
Humanist Society Scotland
Law Society of Scotland
Liam McArthur MSP (Member in charge of the Bill and officials)
Marie Curie Scotland
Mason Institute for Medicine, Life Sciences and the Law (University of Edinburgh)
Mills, Dr Sarah (University of St Andrews)
MND Scotland
Neal, Dr Mary (University of Strathclyde)
Not Dead Yet UK
Our Duty of Care
Police Scotland
Royal College of General Practitioners Scotland
Royal College of Nursing Scotland
Royal College of Psychiatrists in Scotland
Royal Pharmaceutical Society
Scottish Christian Forum on Assisted Dying
Scottish Government (Cabinet Secretary for Health and Social Care and officials)
Scottish Human Rights Commission
Scottish Partnership for Palliative Care
The Australian Centre for Health Law Research
Other correspondence
Assisted dying and domestic abuse
Assisted dying and older people
Assisted dying and people with disabilities
Call for views
Assisted dying legislation in other jurisdictions
Evidence Programme
Financial Memorandum
Impact assessments
Insurance and insurers
The workforce and the role of nursing, social work and social care
Notes of fact-finding visits and engagement activity
On 7 January 2025, the Committee undertook informal engagement with members of The Assembly, a group comprising of people with a learning disability and autistic people, about the Assisted Dying for Terminally Ill Adults (Scotland) Bill.
As a further part of its scrutiny, the Committee engaged with a number of organisations to help identify individuals living with a terminal illness who would be willing to share testimonies of their lived experience and their views on the Bill. In response, the Committee received the following contributions: