Neurodevelopmental Pathways and Waiting Times in Scotland
The number of children and adults seeking assessments for conditions such as autism and ADHD has grown dramatically over the last decade. This has led to increased pressure on Scotland's neurodevelopmental services. This briefing examines the current provision for neurodevelopmental assessment in Scotland, with a focus on diagnostic pathways and waiting times across NHS boards.
Summary
It is estimated that 10-15% of the population in Scotland is neurodivergent, meaning that a person's selective neurocognitive functions (such as the ability to learn and use language, or regulate attention, emotions and impulses) fall outside the usual range. Examples of neurodevelopmental conditions include autism, a lifelong condition affecting around 3% of people1, and ADHD, which affects around 5% of children and 2.5 - 4% of adults. These conditions frequently co-occur with each other2.
While a range of support services, environmental modifications, medications and therapies are available for people with some neurodevelopmental conditions, neurodivergent people can experience significantly poorer health and social outcomes. These can include discrimination, stigma, worse mental health outcomes and shorter life expectancy. In addition, while autism and ADHD have historically been thought to affect predominantly males, evidence now suggests that neurodivergent womenare systematically under-diagnosed due to a lack of societal understanding of the range of autism and ADHD presentations. Neurodivergent people from minority ethnic groups, who may exhibit different symptoms of neurodivergence, also experience this additional disadvantage and stigma.
While neurodivergence is not a mental health condition, the barriers and difficulties faced by neurodivergent people often lead to mental health conditions3. Neurodivergent children and adults who meet the criteria for secondary mental health services due to co-occurring mental health conditions are diagnosed and treated for those conditions through those services. These services are either Child and Adolescent Mental Health Services (CAMHS), or adult mental health services. They will also receive assessment and support for neurodevelopmental conditions through those services.
The Scottish Government's National Neurodevelopmental Specification sets out standards of care for all children and young people with neurodevelopmental differences, regardless of whether they meet the CAMHS criteria. This has led to the implementation of children's neurodevelopmental pathways in many areas of Scotland, bringing together local services (such as health and social care, education and community support) within a whole-system approach. Much of this work focuses on the creation of multi-disciplinary teams to triage, diagnose and support children with neurodevelopmental conditions. This is in line with guidance from groups such as the National Autism Implementation Team. Successful implementation of these pathways also requires efficient collection and use of data to understand demand and capacity.
The provision of both support and assessment for neurodivergent people varies significantly across Scotland. Pathways for neurodivergent children to obtain a neurodevelopmental assessment have been implemented in every NHS board, although the mode of access and delivery can vary. In addition, NHS Tayside has recently stopped accepting new referrals for neurodevelopmental assessments for children and young people who do not meet the CAMHS referral criteria.
Data presented in this report shows that as of March 2025, over 42,000 children were waiting for a neurodevelopmental assessment, and that in some areas this figure has increased by over 500% since 2020. Across the health boards surveyed, on average, the longest waiting time for a child to receive an assessment was 196 weeks (nearly four years). This is due to the increase in demand for neurodevelopmental assessments massively outstripping the services' capacity to deliver them. However, support is available for neurodivergent children who don't have a diagnosis, most commonly through local authorities and their provision of Additional Support for Learning.
Increased awareness of neurodivergence in adults has also led to a surge in demand for adult neurodevelopmental assessments, and the data in this report suggests that there were over 23,000 adults waiting for a neurodevelopmental assessment in Scotland as of March 2025. In areas for which data is available, the number of adults waiting for an assessment has increased by over 2200% since 2020. Despite this demand, adult neurodevelopmental pathways are not available in many NHS boards across Scotland, and in some areas adult assessment services have been withdrawn in recent months. In areas for which data is available, the average longest waiting time to receive an assessment is 182 weeks (three and a half years).
Long waiting times have resulted in more people using the private sector to obtain a neurodevelopmental assessment, which may lead to financial hardship4. In some cases, patients who have received a private diagnosis enter a shared care agreement, whereby they receive their medication through an NHS prescription. However, in many areas GPs do not accept private diagnoses and do not enter such agreements, meaning that the patient may have to pay for medication themself.
Increased demand for support has also led to increased pressure on thethird sector, which provides a range of pre- and post-diagnostic support for neurodivergent people in Scotland. In areas such as Fife, third sector organisations are formally involved in neurodevelopmental pathways, where they provide support and services in tandem with local authorities. The Royal College of Psychiatrists in Scotland and the Child Heads of Psychology Services in Scotland have called for a restructuring of neurodevelopmental pathways in Scotland, in which the third sector would play a more formalised role nationally. This would build on schemes already funded by the Scottish Government, such as the National Autism Post-Diagnostic Support Service and the Autistic Adult Support Fund.
Neurodivergent people may also receive a range of support outside the NHS and third sector. This can include in employment, where they may be eligible for reasonable adjustments in the workplace under the Equality Act 2010, in education, where they may require additional support needs under Getting It Right For Every Child (GIRFEC) policy, and in social security mechanisms, where they may be eligible for disability payments.
Post-diagnostic support also plays an important role in helping a neurodivergent person to understand their needs and the strategies for addressing them. This should be part of the neurodevelopmental pathway, although it can take highly variable forms including clinical support, education programmes and peer-led support.
The National Neurodevelopmental Specification states that none of this support should be diagnosis-dependent; in all cases, services should provide support on a needs-based, case-by-case basis. However, many neurodivergent people have found that accessing these services can be difficult, particularly without a formal diagnosis.
This briefing presents up-to-date data on the current waiting lists and waiting times for neurodevelopmental assessments across Scotland. It sets out the current and future policy for neurodivergent people in Scotland and surveys the current provision of neurodevelopmental pathways across all fourteen territorial NHS boards. It also explores the issues outlined above, to provide a picture of the major challenges facing both policymakers and neurodivergent people themselves in Scotland.
Cover photo of Scottish Parliament
Neurodevelopmental pathways and waiting times
Neurodivergent children and adults in Scotland are waiting longer than ever to be assessed for neurodevelopmental conditions such as autism or ADHD, to the point that the situation has been labelled by some as a 'crisis'. There are significant bottlenecks in the pathway between referral and assessment, and in some cases this has led to health boards withdrawing diagnostic services altogether. This has created challenges accessing diagnosis and support for many people, and this briefing will explore these issues. It will first present up-to-date information on neurodevelopmental pathways and waiting times across Scotland. It will then examine the present and future policy provisions and the current neurodevelopmental pathways available for children and adults in Scotland. The last section explores other issues impacting neurodivergent people in Scotland, and the next steps to be taken in this area.
Overview
This section introduces neurodevelopmental pathways and waiting times. It begins by defining the key terminology used in this briefing and setting out the language used when discussing these topics. It then discusses the evidence surrounding the prevalence of neurodevelopmental conditions in Scotland.
Definitions and language
This section defines the terms used in this briefing. The meanings of these terms have changed over time, and are not universally agreed, but the definitions in this report align with those used in the Scottish Government's National Neurodevelopmental Specification.
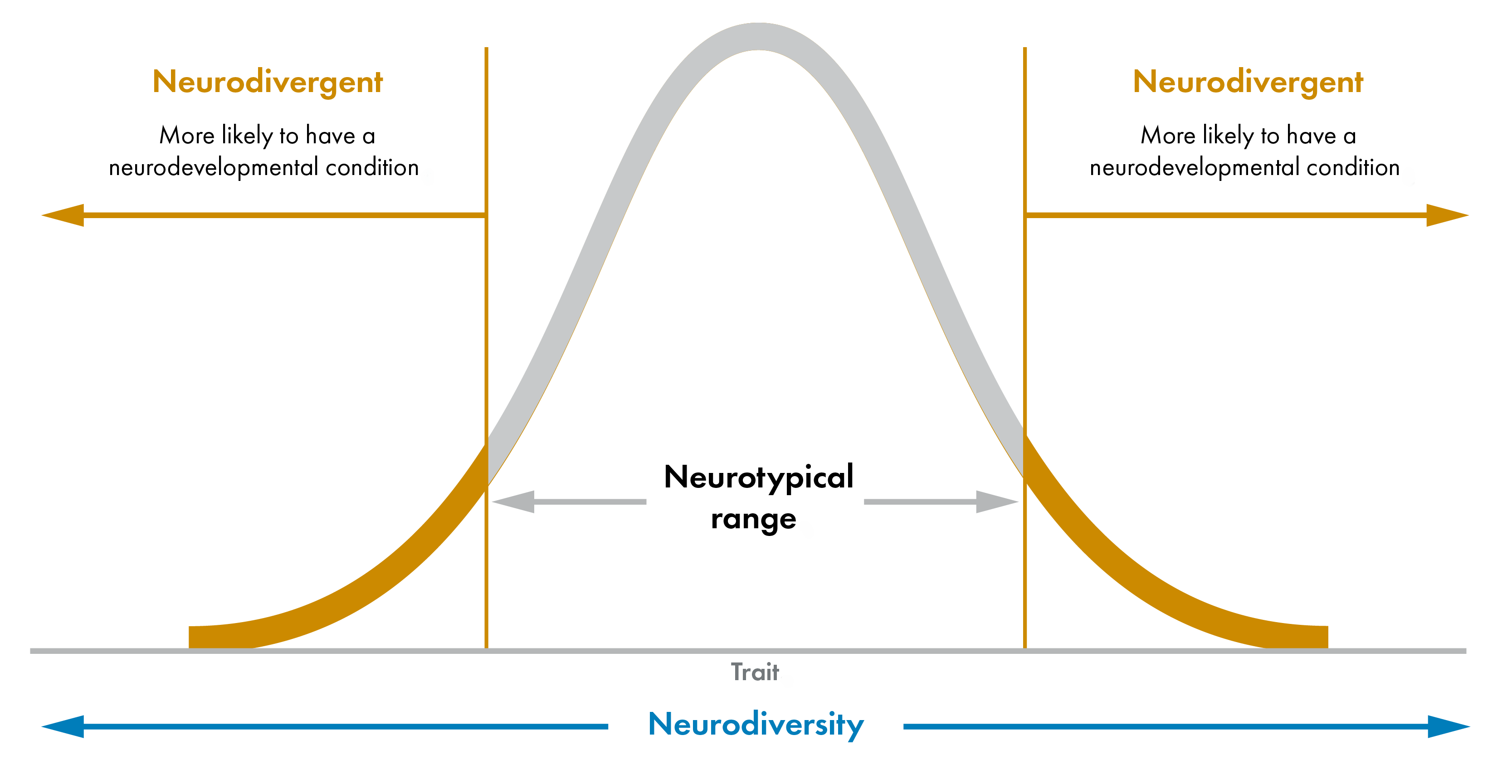
Neurodiversity: The natural variation in brain development in the population as a whole. This is a property of a group, rather than of a single individual, and a person cannot 'be neurodiverse' or 'have neurodiversity'. There is no formal definition of neurodiversity in Scottish law, but this definition aligns with that provided by the Scottish Deanery.
Neurocognitive functions: Selective aspects of brain functions, including:
the ability to learn and use language
the ability to regulate attention, emotions, impulses (including movements and spontaneous utterances)
social behaviours
processing sensory stimuli.
These traits may be significantly genetically influenced1, and are present from birth. The statistical normal range changes, dependant on age.
Neurodivergence: When an individual's selective neurocognitive functions fall outside the typical range. This includes, but is not limited to, conditions such as autism, attention deficit-hyperactivity disorder (ADHD), dyslexia, dyscalculia, developmental co-ordination disorder (DCD), developmental language disorder (DLD), Foetal Alcohol Syndrome Disorder (FASD) and Tourette's syndrome. These specific conditions are also referred to as neurodevelopmental conditions, although conditions such as dyslexia and dyscalculia are also termed learning difficulties by some people. Of the neurodevelopmental conditions listed above, this briefing will mostly focus on autism and ADHD (see below), although not all neurodivergent people have a specific neurodevelopmental condition. A neurotypical person is someone whose variation in brain development falls within the the typical range. This is shown in the figure below.
Autism: A lifelong developmental condition that affects the way a person communicates, interacts, and processes information. It is also known as autism spectrum disorder (ASD), reflecting the wide range of how autism presents in different individuals and the varying levels of support needed. Current estimates indicate about 1 in 34 people are autistic (just under 3% of the population)3. This would suggest there are approximately 160,000 autistic people in Scotland as of 20234. Current thinking advocates for a 'neuro-affirming' paradigm that would not seek to fix or cure autistic people, but rather to take a ‘difference not deficit’ approach5. This recognises different ways of being rather than a focus on impairment and disability, and focuses on adapting the physical and social environment around the autistic person to suit their needs.
Attention deficit-hyperactivity disorder (ADHD): A group of behavioural symptoms that include difficulty in concentrating, hyperactivity, and impulsiveness. Research indicates that ADHD affects around 1 in 20 school aged children (5% of the population), and between 1 in 25 and 1 in 40 adults (2.5-4%). This would suggest that there are between 150,000 and 220,000 people living with ADHD in Scotland as of 2023. While the cause is unknown, medication can help to relieve the symptoms and is often prescribed in combination with a neuro-affirming approach. However, less than 30% of children estimated to have ADHD (and less than 10% of adults) are prescribed medication in Scotland6.
Neurodevelopmental pathway: The framework for assessing a neurodivergent person for a range of conditions and providing support before, during and after this assessment. This briefing will focus on mainly the assessment stage, although the National Neurodevelopmental Specification for Children and Young People outlines the importance of support regardless of diagnosis. Neurodevelopmental pathways are different to single-condition assessments or pathways, such as autism or ADHD pathways, in that they consider the whole profile of the individual patient and may diagnose more than one neurodevelopmental condition. NHS Education for Scotland mentions "increasing support for taking a 'neurodevelopmental' approach to understanding the range of ways children, young people and adults present".
We recognise the importance of the terminology used in reference to the various groups discussed in this briefing. Following the responses to the Scottish Government's consultation on the Learning Disabilities, Autism and Neurodivergence Bill, we use identity-first language (i.e. 'autistic person', 'neurodivergent person') wherever possible when discussing neurodivergence. We also recognise that neurodivergence is not a mental health condition and should not be treated as such, although neurodivergent people are more likely to experience mental and physical health challenges in their lifetimes.
Prevalence of neurodivergence in Scotland
Recent evidence suggests that 10-15% of the population in Scotland are neurodivergent in some way1. This falls in line with estimates made for the UK as a whole2. This number also seems to be roughly consistent across adults and children, with one study suggesting a rate of neurodivergence of roughly 16% in primary school children in 20223.
The most common neurodevelopmental conditions are thought to be dyslexia and dyscalculia, affecting 10% and 6% of the population respectively45. ADHD is estimated to affect 5% of school aged children in Scotland6, while autism affects roughly 3% of this group3. Given the lifelong nature of such conditions, prevalence in adults is similar, with 2.5-4% of adults living with ADHD8 and approximately 2.2% having autism9. The differences are likely due to a lower rate of diagnosis of these conditions in adults.
A person with one neurodevelopmental condition has a much greater chance of also having another. Studies have estimated that nearly 40% of autistic people also have ADHD or other forms of neurodivergence and/or a learning disability, and others put the number even higher1011. As a result, it may be harder to diagnose both conditions accurately. Furthermore, the traits of one may exacerbate the other. Having both autism and ADHD has been found to increase the likelihood of developing conditions such as schizophrenia, bipolar disorder, depression and anxiety12.
Diagnosis of these neurodevelopmental conditions varies between sexes. According to the Scottish ADHD Coalition, men are three to four times more likely to be treated for ADHD than women, although this is more likely due to under-diagnosis of females rather than a difference in true prevalence13. This could be because the symptoms of ADHD in females frequently present differently to symptoms in males, and are noticed less often by families and teachers1415. While males are more likely to show impulsive and hyperactive symptoms, females tend to exhibit more inattentive and internal behaviours and are more likely to 'mask' their symptoms. Since these behaviours are less disruptive, they are often missed and can be misdiagnosed as symptoms of anxiety or depression.
Autism is also more prevalent in men than in women, although as with ADHD there is some debate as to whether this is due to a true difference in the underlying prevalence, or whether autism is simply under-diagnosed in women. Current estimates have the ratio of autistic males to females as 3:1. Some feel that autistic women and girls often present different characteristics to autistic men and boys, which don't fit the traditional profile of autism and are therefore missed by many assessments. In addition, autistic women and girls are more likely to successfully mask their symptoms than men and boys16. The difficulties facing autistic women and girls are discussed in more detail in the issues section.
Recent evidence also suggests that the prevalence of people diagnosed with a neurodevelopmental condition and those identifying as neurodivergent has increased over the last decade. One study found an increase of over 10% in neurodivergence - and over 30% in cases of autism - in Scottish primary schools between 2018 and 20223. In other statistics, the increase is far more dramatic. For example, the Salvesen Mindroom Centre in Edinburgh (a charity working with neurodivergent people) reported a 295% increase in the number of neurodivergent people it worked with between 2020 and 2024. In Glasgow, there was a 1000% increase in referrals for assessment of adult ADHD to Community Mental Health Teams between 2018 and 2021. These increases are almost certainly due to an increase in awareness of neurodivergence as a phenomenon, as opposed to an increase in the proportion of people who are neurodivergent, and this is discussed further in the issues section.
Waiting times for neurodevelopmental assessment in Scotland
This section begins by outlining previously available data about waiting times for neurodevelopmental assessment in Scotland, and in the United Kingdom more broadly. Historically, these data have only been available through one-off publications and Freedom of Information requests.
In March 2025, the Health, Social Care and Sport Committee wrote to each of the fourteen NHS territorial boards requesting information on neurodevelopmental pathways and waiting times. All boards responded, and the following sections summarise the responses received.
It is worth noting that data concerning waiting times and waiting lists for neurodevelopmental assessments, while informative in understanding the discrepancy between demand and capacity, does not give information about how long people are waiting for support in each area. The Scottish Government has stated that support should not be dependent on diagnosis, and should be available for those waiting for assessment or not seeking one. The National Neurodevelopmental Specification notes that:
understanding of support needs can be enhanced by diagnosis but should not wait for diagnosis.
Scottish Government, National Neurodevelopmental Specification for Children and Young People, 2021
Nonetheless, neurodivergent people report that the experience of waiting causes significant stress and anxiety, and so the following data is important in understanding and improving their experience1.
Previous data on waiting times for neurodevelopmental assessment in Scotland
Significant interest has surrounded the subject of waiting times for mental health diagnosis in Scotland. Public Health Scotland regularly publishes waiting times data for referrals to Children and Adolescent Mental Health Services (CAMHS). The national target is for 90% of patients to start treatment within 18 weeks of referral for all CAMHS treatment. In March 2025, the CAMHS data showed that this target had been met for the first time in the period September-December 2024. The target was met again in the following quarter, January-March 2025. This came after less than 70% of patients were being seen within 18 weeks as recently as 2022.
In the past, neurodevelopmental cases were included in CAMHS waiting time statistics. However, in recent years these have been separated out. This is done in recognitiono of the fact that neurodivergence is not a mental health condition and that, unless they meet the national referral criteria for treatment by CAMHS, neurodivergent children do not need to be 'treated' in a medical sense. As such, they are not recorded as patients requiring mental health support. The removal of neurodevelopmental cases led to some politicians commenting that:
The only way that ministers have been able to meet their target on waiting times for child and adolescent mental health services has been by removing from the waiting times figures young people and children who were waiting for attention deficit hyperactivity disorder and autism diagnoses.
Miles Briggs MSP, First Minister's Question Time, 3 April 2025
However, these accusations have been refuted, with the Minister for Social Care, Mental Wellbeing and Sport stating that:
CAMHS is not the correct service for children who are seeking a diagnosis for neurodevelopmental conditions such as ADHD, unless they have a co-existing mental health condition. For many young people, a neurodevelopmental pathway will ensure that the right help and support is provided.
Minister for Social Care, Mental Wellbeing and Sport (Maree Todd), Portfolio Question Time, 7 May 2025
Data concerning waiting times specifically for neurodevelopmental assessment has previously only been made available via Freedom of Information requests and one-off publications. For example, NHS Lothian disclosed the average waiting times for children and adults seeking a neurodevelopmental assessment in May 2024. In the year 2023/2024, adults and children were waiting an average of 101 and 68 weeks, respectively, for assessment. NHS Tayside reported an average waiting time of 37 weeks for the period September 2024-December 2024. These data show only snapshots of the situation at a single moment in time, and no data on the long-term trends in waiting times is routinely published.
One study looked at neurodevelopmental assessments (n:408) completed by ten of the fourteen NHS Scotland territorial boards between October 2021 and May 20221, and compared waiting times to the 36-week standard recommended by the National Autism Implementation Team. It found that the mean time for a patient to undergo the entire assessment process from referral was 52 weeks for adults and 82 weeks for children, both far greater than the recommended standard. While mean values can be skewed by long waiting times, the median wait time was 36 weeks for adults and 75 weeks for children, and only 47% of cases (20% for children) met the 36-week standard.
Elsewhere, NHS England routinely publishes autism assessment waiting times on its dashboard. The National Institute of Care Excellence (NICE) guideline is that patients should have their first appointment for assessment within 13 weeks of referral. In March 2025, less than 5% of both children and adults with a referral met this threshold, down from 12% in December 2019. The Children's Commissioner for England reported in 2024 that the median wait time for a neurodevelopmental assessment was 117 weeks. In October 2023, ADHD UK surveyed various UK NHS Foundation Trusts and found waiting times varying hugely, from 5 to 264 weeks for children, and 12 to 550 weeks for adults. Unlike in Scotland, patients in England may choose a private provider for autism and ADHD diagnosis under the Right to Choose scheme. Under this scheme, the NHS covers the cost of a private diagnosis. This is available to patients who are registered with a GP in England and have received a referral for an ADHD or autism diagnosis.
Number of children and adults on waiting lists
This section will summarise the data received by the Health, Social Care and Sport Committee regarding the number of children and adults waiting for a neurodevelopmental assessment as of 31st March 2025. For more details on the neurodevelopmental pathways in each NHS board, see the neurodevelopmental pathways section.
Children
As of 31st March 2025, all health boards (with the exception of NHS Tayside, who were not accepting new referrals) had neurodevelopmental pathways for children who didn't meet the criteria for referral to CAMHS. Thirteen of the fourteen health boards reported the number of patients waiting for this service (except for NHS Grampian, who could not provide this figure). The data show that there were 42,530 children waiting for a neurodevelopmental assessment. This amounts to approximately one in twenty-five children aged 0-18, based on 2023 population estimates1. Figure 2 shows the breakdown of these across health boards.
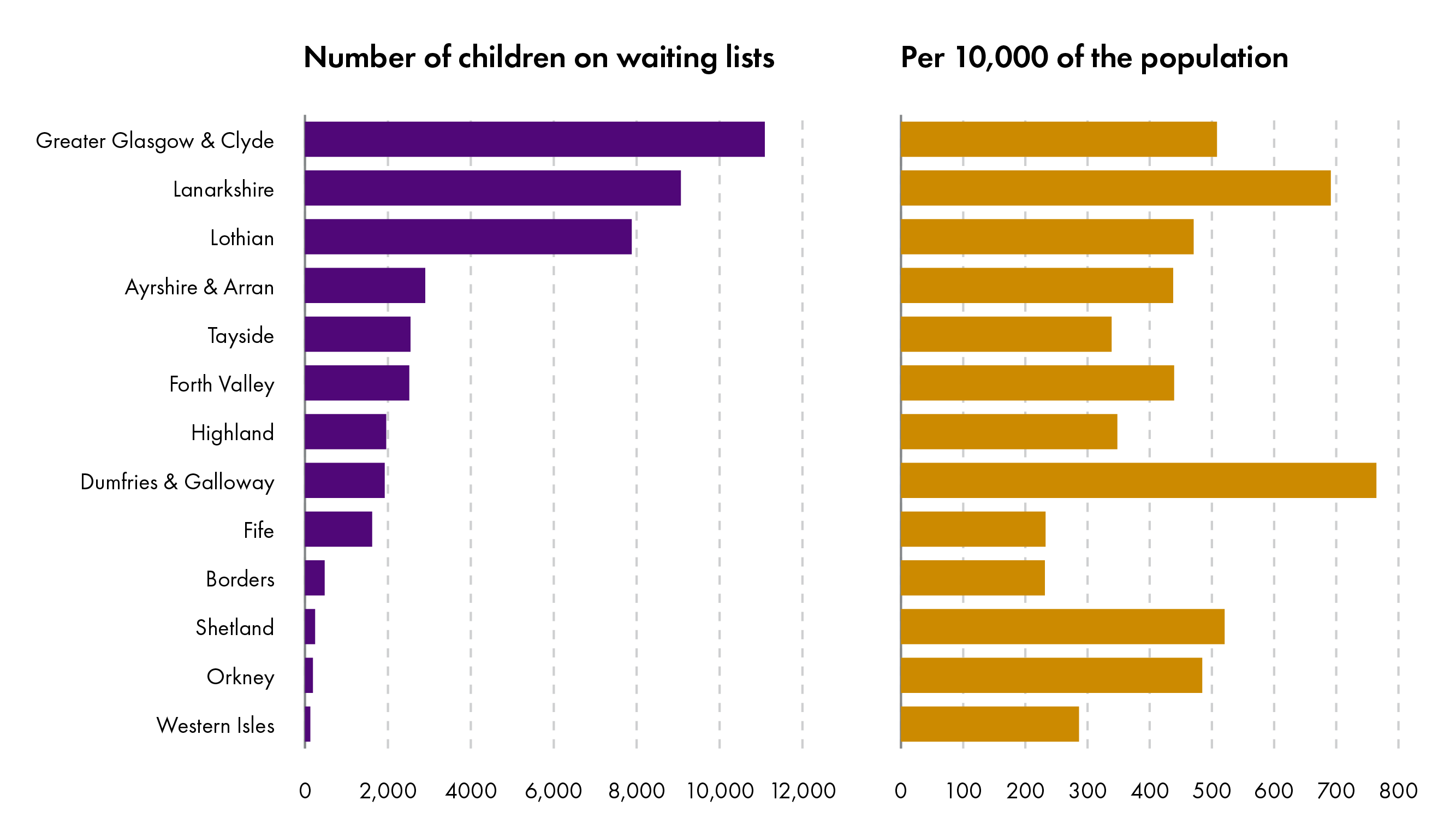
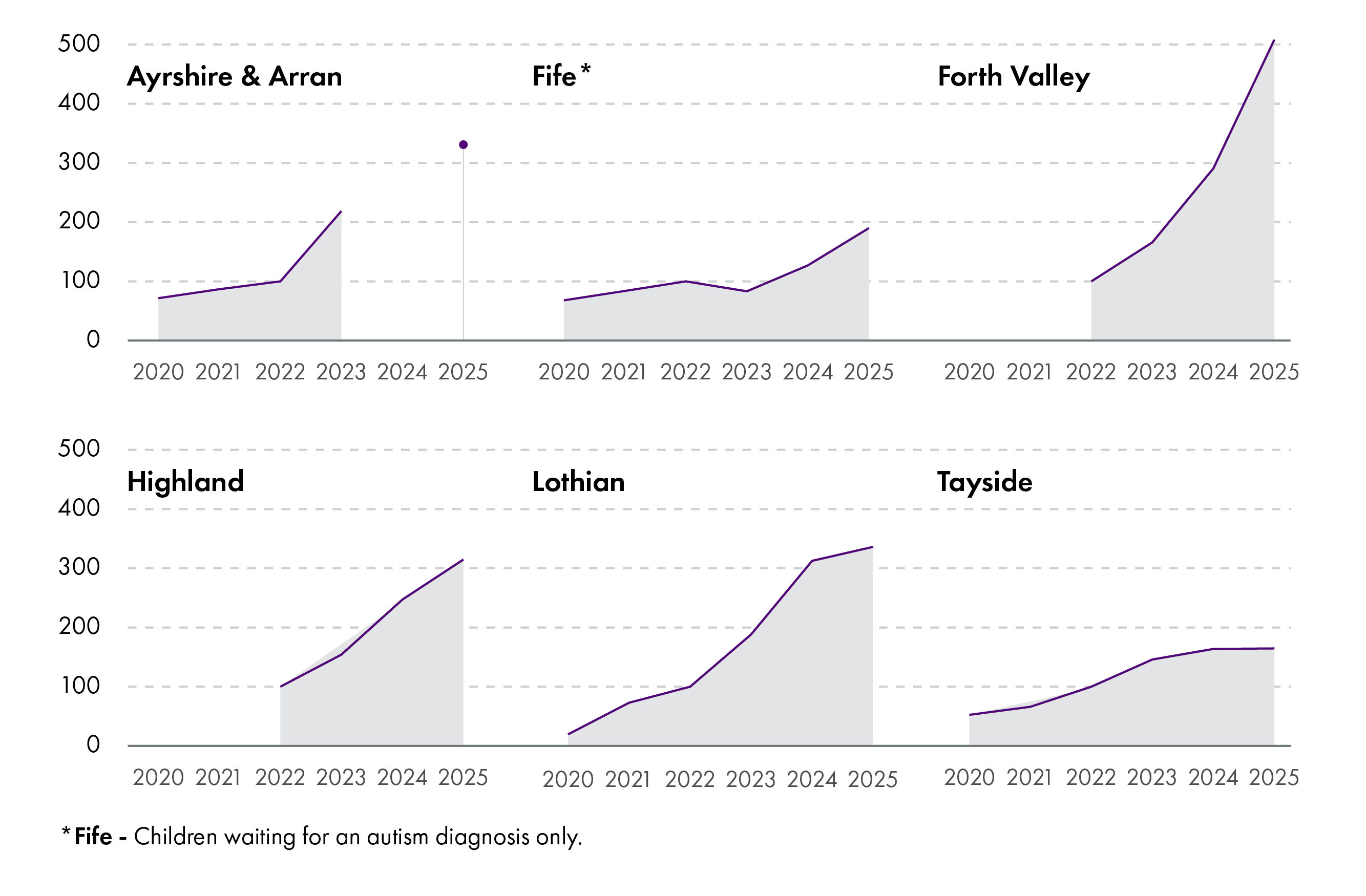
Eight health boards (Ayrshire and Arran, Fife, Lothian, Tayside, Borders, Forth Valley, Greater Glasgow and Clyde and Highland) were able to provide data on the length of waiting lists in previous years, although only the first four provided data going as far back as 2020. This data is shown in figure 3 below, which shows that the number of children waiting for a neurodevelopmental assessment in Ayrshire and Arran, Fife, Lothian and Tayside increased from 2,475 to 14,943 between 2020 and 2025 - an increase of over 500%. This is more likely due to a large increase in the number of people seeking assessments, as opposed to an increase in the number of people with neurodevelopmental conditions.
Adults
Health boards reported that a neurodevelopmental pathway was available to adults who did not meet the criteria for referral to secondary mental health services in six health boards (Greater Glasgow and Clyde, Lanarkshire, Lothian, Tayside, Highland and Western Isles), although in Tayside and Western Isles this was for autism only. In NHS Grampian, the provision was different across the three Health and Social Care Partnerships (HSCPs) since Aberdeenshire HSCP ceased its adult neurodevelopmental pathway in February 2025. This is summarised in figure 4.
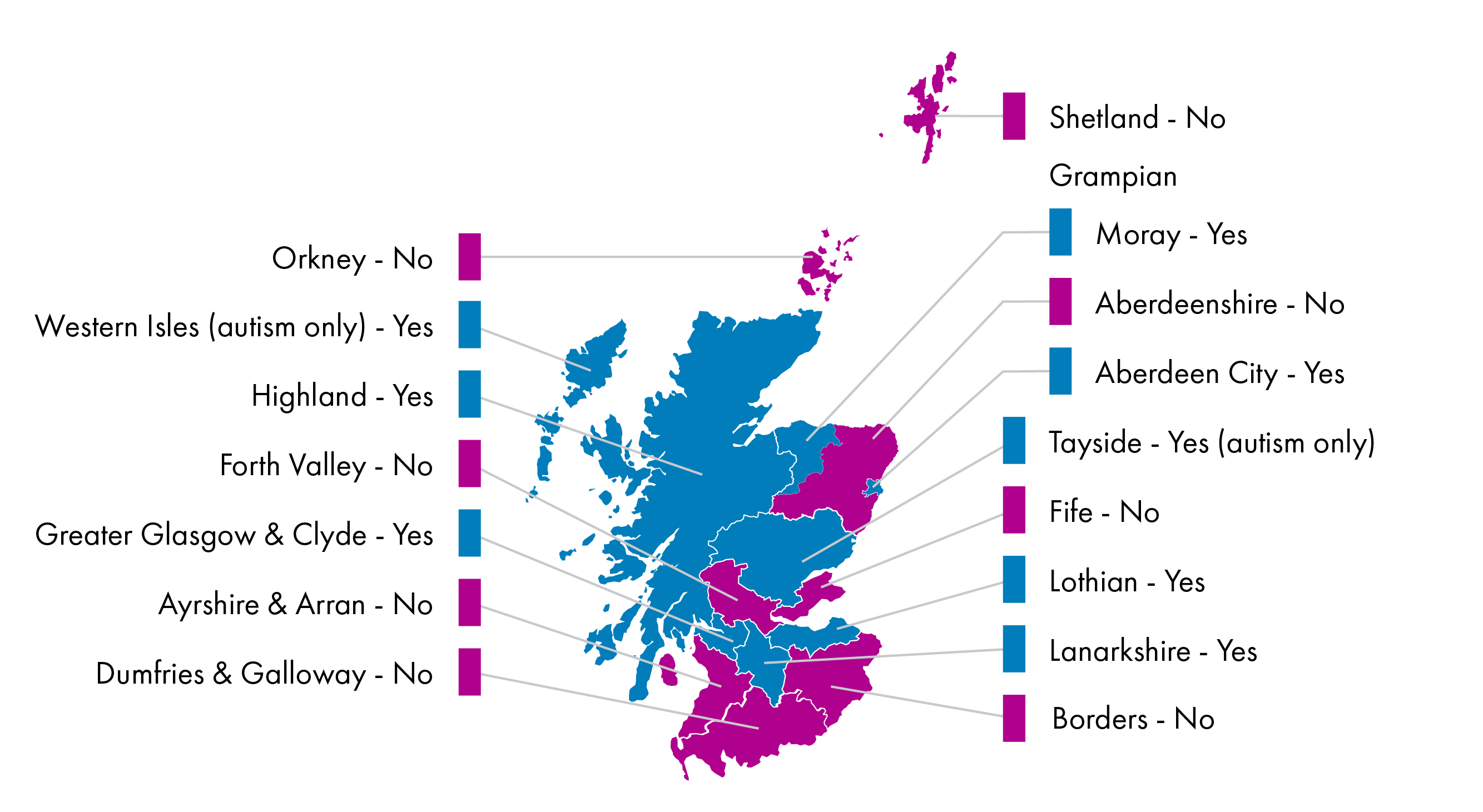
Nine health boards disclosed the number of adults waiting for a neurodevelopmental assessment in their areas. These were five of the health boards with adult neurodevelopmental pathways in place (Greater Glasgow and Clyde, Highland, Lothian, Tayside and Western Isles but not Lanarkshire) and four of the boards which offered neurodevelopmental assessments only to those who met the criteria for referral to secondary mental health services (Ayrshire and Arran, Fife, Orkney and Shetland).
There were 23,339 adults reported as waiting for a neurodevelopmental assessment as of March 2025, and over 97% of these were in areas where adults did not have to meet the criteria for referral to secondary mental health services to access the services. The breakdown by health board is shown in figure 5.
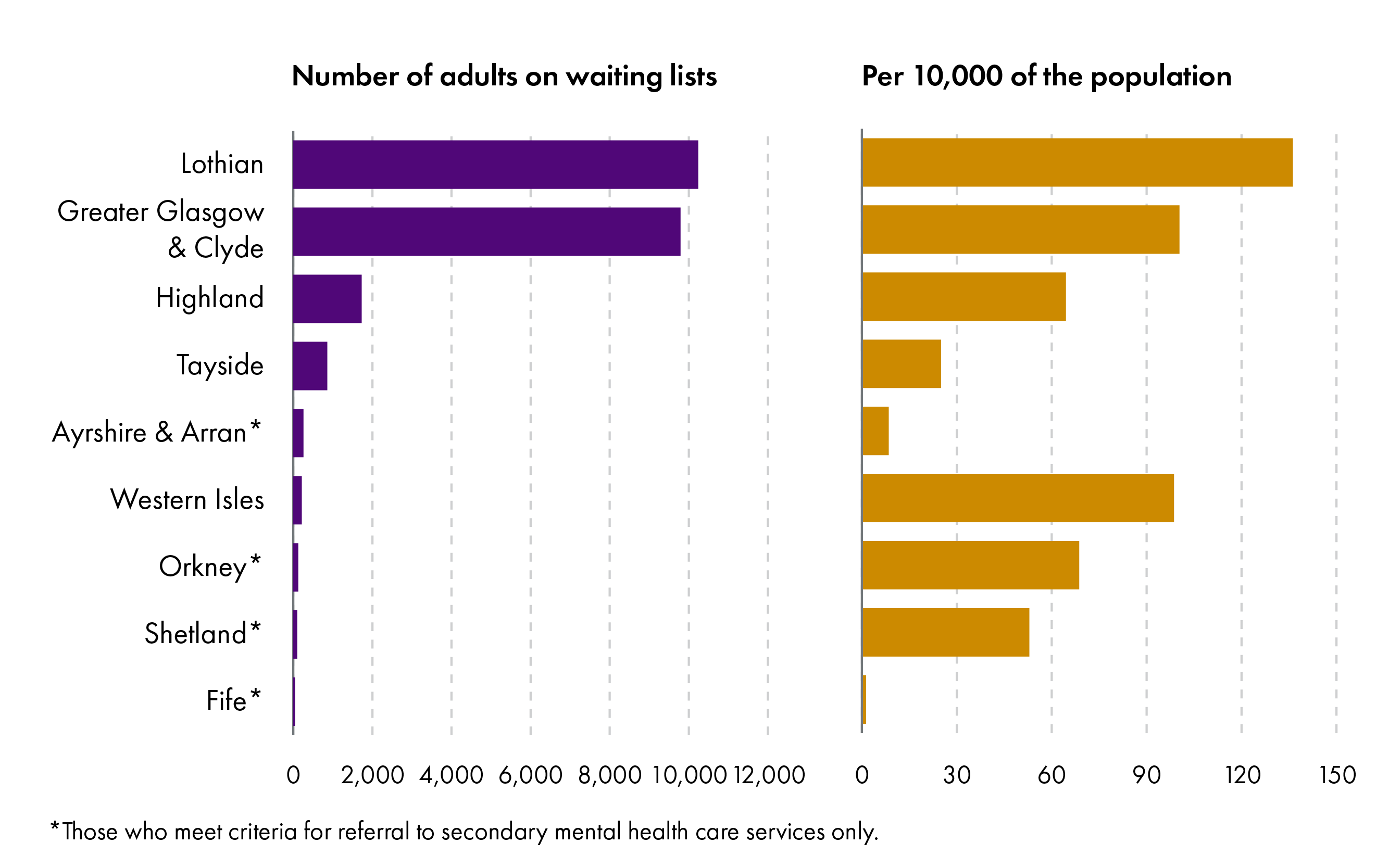
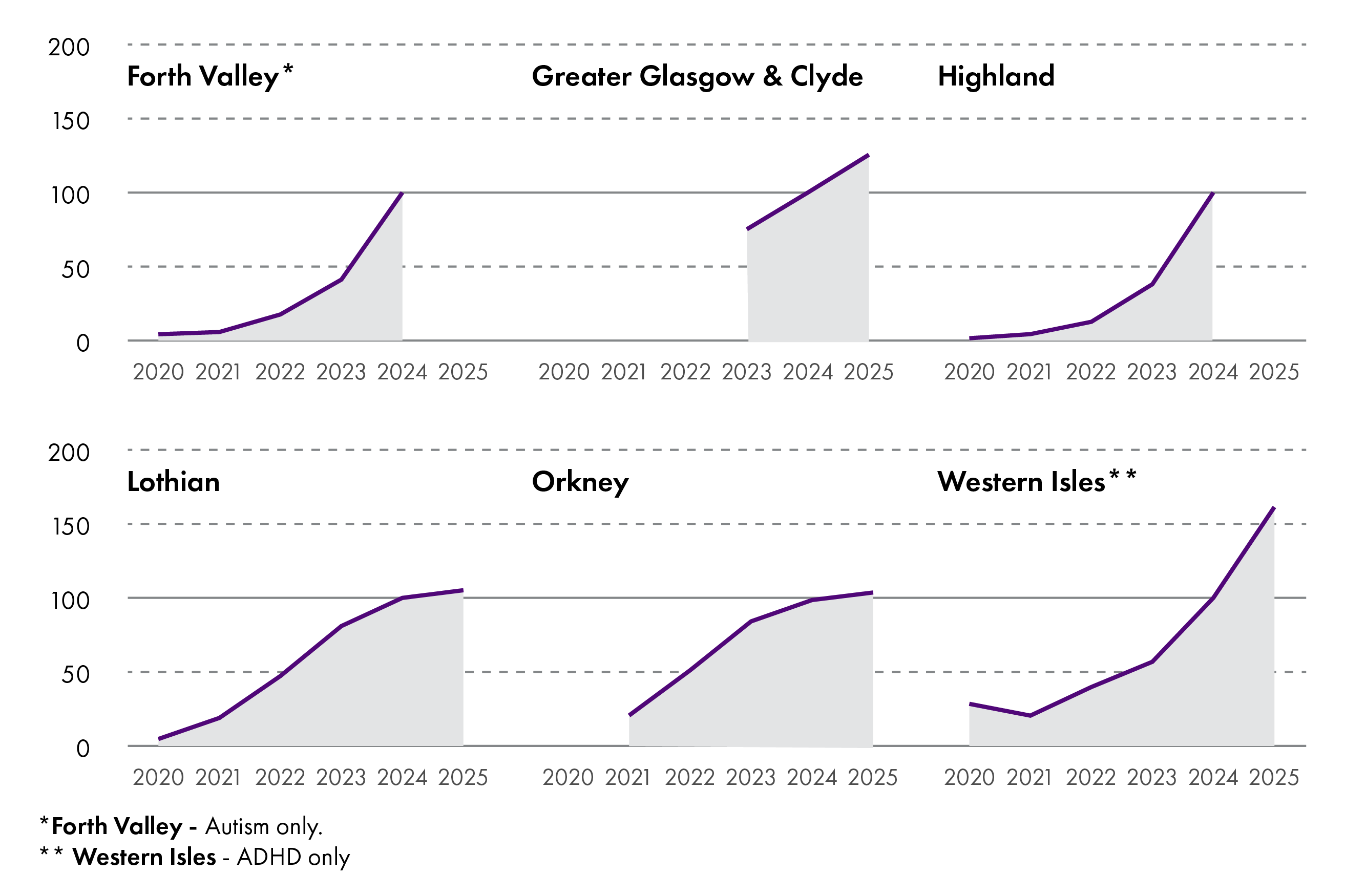
Six health boards (Forth Valley, Highland, Lothian, Western Isles, Greater Glasgow and Clyde and Orkney) were able to provide data on waiting lists lengths for previous years, although only the first four provided data going back to 2020. The figures from Forth Valley include autism assessments only, while those for Western Isles are for ADHD only. These data are shown in figure 6 below, which shows that the number of adults waiting for a neurodevelopmental assessment in Forth Valley, Highland, Lothian and the Western Isles increased from 543 to 12,974 between 2020 and 2025 - a total increase of over 2200%. As with the data for children, this is unlikely to be due to such an increase in the number of people with neurodevelopmental conditions, but is likely to reflect an increased awareness of these conditions and the ways they can present.
Waiting times for children and adults
Children
All health boards reported the median and longest current waiting times for children seeking a neurodevelopmental assessment, except for NHS Grampian (which could not provide data specific to neurodevelopmental cases) and NHS Dumfries and Galloway (which provided a longest waiting time only). These are shown in figure 7 below. Median waiting times ranged between 22 weeks (NHS Western Isles) and 141 weeks (NHS Ayrshire and Arran), with an average median waiting time of 76 weeks. Longest waiting times ranged between 69 weeks (NHS Fife) and 342 weeks (NHS Ayrshire and Arran), with an average longest waiting time of 196 weeks.

In some cases, it is claimed that children are waiting on these lists for long enough that by the time they are seen, they are no longer eligible for neurodevelopmental support through these pathways by virtue of having turned 18.
Adults
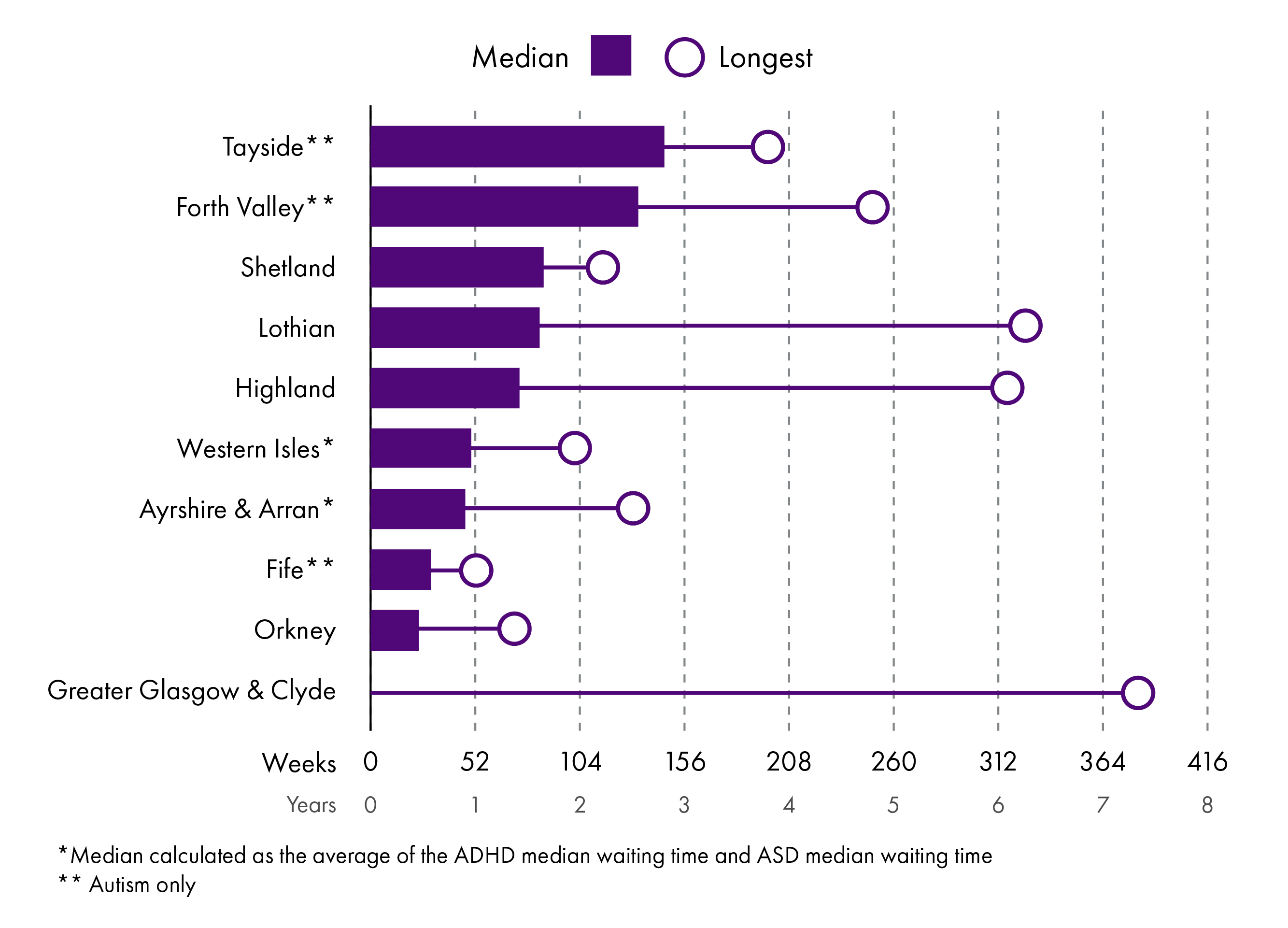
Nine health boards (Lothian, Ayrshire and Arran, Tayside, Forth Valley, Highland, Fife, Shetland, Orkney and Western Isles) reported both the median and longest waiting time for an adult seeking a neurodevelopmental assessment, while Greater Glasgow and Clyde reported the longest waiting time only. Forth Valley, Tayside and Fife reported waiting times for autism assessment only, while the median waiting time for Ayrshire and Arran and Western Isles is the average of the medians for autism and ADHD individually. These are shown in figure 8. Median waiting times ranged between 24 weeks (NHS Orkney) and 146 weeks (NHS Tayside), with an average median waiting time of 76 weeks. Longest waiting times ranged between 61 weeks (NHS Fife) and 390 weeks (NHS Greater Glasgow and Clyde), with an average longest waiting time of 182 weeks.
Waiting lists for ADHD medication
If a patient is diagnosed with ADHD, they may be prescribed medication. Six health boards (Ayrshire and Arran, Borders, Forth Valley, Grampian, Lothian and Tayside) operate waiting lists for ADHD medication for children. Five of these (all except for Forth Valley) reported the number of children on the waiting list, and the median and longest waiting times. This is shown in table 1 below.
| Board | Number of children on waiting list | Median waiting time | Longest waiting time |
|---|---|---|---|
| Ayrshire and Arran | 114 | 32 weeks | 62 weeks |
| Borders | 4 | 3 weeks | 6 weeks |
| Grampian | 75 | 15 weeks | 22 weeks |
| Lothian | 722 | 72 weeks | 205 weeks |
| Tayside | 257 | Not provided | 148 weeks |
For adults, four health boards reported operating waiting lists for medication, although these were not in operation in all Health and Social Care Partnerships (HSCPs) in some cases. Forth Valley operated a waiting list in Clackmannanshire and Stirling, but not in Falkirk, while Lothian operated waiting lists in East Lothian, Midlothian and Edinburgh City but not in West Lothian. NHS Highland and NHS Orkney operated waiting lists across the whole health board. Waiting list lengths, and median and longest waiting times (where available) are shown in table 2 below:
| Board | Number of adults on waiting list | Median waiting time | Longest waiting time |
|---|---|---|---|
| Forth Valley | 24 (Clackmannanshire and Stirling only) | Not provided | Not provided |
| Highland | 174 | 30 weeks | Not provided |
| Lothian | 410 (East Lothian, Midlothian and Edinburgh City only) | 41 weeks | 222 weeks |
| Orkney | 71 | 48 weeks | 112 weeks |
In areas where a waiting list system is not in operation, medication can be prescribed as part of the post-diagnostic service.
Current Policy
This section will start by outlining the current policy provisions for neurodivergent people in Scotland, including a summary of current funding mechanisms to support organisations that work with neurodivergent people. It will then discuss the future of this area in relation to the Scottish Government's proposed Learning Disabilities, Autism and Neurodivergence Bill.
Present and past policy provisions
A number of policy areas have influenced the provision of assessment and support for neurodivergent people in Scotland. This section will outline the key legislative and policy developments relating to neurodivergent people since 1999.
The Equality Act 2010
Equal opportunities is a matter reserved to the UK Parliament, which includes the Equality Act 2010. The Equality Act applies to England, Scotland and Wales.
The Equality Act prohibits discrimination because of a 'protected characteristic' in areas such as employment, education and housing. Disability is one of the nine protected characteristics. It is defined as 'a physical or mental impairment which has a substantial and long-term adverse effect on that person's ability to carry out normal day-to-day activities'. While the Equality Act does not mention autism or neurodivergence explicitly, such conditions may meet the requirements to qualify as a disability under the Act, if they can align their presentations with the definition above. As a result, many autistic and neurodivergent people:
are protected from discrimination, harassment and victimisation
are entitled to 'reasonable adjustments' if they feel they are at a substantial disadvantage compared to someone who is not disabled. This can be in the workplace, in education or when accessing services. Reasonable adjustments may take the form of accessible environments, flexible working hours or additional support during interviews. The employer or service provider must pay for these adjustments.
The public sector equality duty also requires public bodies and organisations carrying out public functions to consider the need to:
eliminate 'discrimination, harassment, victimisation and any other conduct that is prohibited by or under this Act’
‘advance equality of opportunity' and 'foster good relations' between those who have a protected characteristic and those who do not.
This duty applies to public bodies in their role as an employer and as a service provider.
Mental health law and strategies
The Mental Health (Care and Treatment) (Scotland) Act 2003, subsequently amended by the Mental Health (Scotland) Act 2015, set out the legal obligation for councils to provide care and support for people with mental disorders. In particular, it established the right of medical professionals to detain and treat patients if they show signs of such mental disorders, but only when the patient poses a significant risk to their own welfare or the welfare of others. Under the Act, mental disorder is defined to include those with learning disabilities, and autism is also included under this definition in practice. However, there is a range of views as to whether mental health law should apply to neurodivergent people, and many neurodivergent people find the classification of autism and other neurodevelopmental conditions as mental health conditions to be stigmatising and offensive.
A number of mental health strategies have also been published by the Scottish Government. The Mental Health Strategy 2017-2027 did not have specific reference to neurodivergent people. Rather, it commissioned a review of whether the 2003 Act adequately fulfilled the needs of autistic people and people with with learning disabilities. This review was scoped in 2017 and addressed in two separate reports.
The Independent Review of Learning Disability and Autism in the Mental Health Act, also known as the Rome Review, was published in December 2019, and addressed the treatment of people with learning disabilities and autism in the Mental Health Act specifically. Among the recommendations of this report were that 'learning disability and autism be removed from the definition of mental disorder in the Mental Health Act' and that 'a new law be created to support access to positive rights'.
The Scottish Mental Health Law Review, published in 2022, carried out a more general review of Mental Health Law in Scotland. Its conclusion was that the framework of any future Mental Health Law 'should apply to all forms of mental or intellectual disability', which includes learning disabilities and autism.
The two reports therefore conflicted on whether mental health law should include autism and learning disabilities. However, the Scottish Mental Health Law Review acknowledged that at the time of its publication, the Scottish Government had committed to taking forward a Learning Disability, Autism and Neurodiversity Bill. This would provide for neurodivergent people specifically, and so follow the recommendation of the Rome Review. However, the Scottish Government broadly agreed with many of the recommendations made by the Scottish Mental Health Law Review as well, and established a new Mental Health and Capacity Reform Programme to implement some of these recommendations.
The updated Mental Health and Wellbeing Strategy, published by Scottish Government in 2023, set out an explicit priority to:
strengthen support and care pathways for people requiring neurodevelopmental support, working in partnership with health, social care, education, the third sector and other delivery partners.
Scottish Government, Mental Health and Wellbeing Strategy, 2023
The Scottish Strategy for Autism
In 2009, the UK Parliament passed the Autism Act 2009. This requires the UK Government to develop and maintain an Autism Strategy for England. The first of these was published in 2011, with the vision that:
...all adults with autism are able to live fulfilling and rewarding lives within a society that accepts and understands them. They can get a diagnosis and access support if they need it, and they can depend on mainstream public services to treat them fairly as individuals, helping them make the most of their talents.
HM Government, 'Fulfilling and Rewarding Lives': The strategy for adults with autism in England, 2011
The implementation of the Act is being looked at by a House of Lords Select Committee.
Corresponding legislation does not exist in Scotland, but the Scottish Government published a similar Scottish Strategy for Autism in 2011. This was a ten-year plan, with the vision that by 2021:
individuals on the autism spectrum are respected, accepted and valued by their communities and have confidence in services to treat them fairly so that they are able to have meaningful and satisfying lives.
Scottish Government, Scottish Strategy for Autism, 2011
Across the first four years of the plan, £13.4 million was committed by the Scottish Government with the goal of improving the lives of autistic people and their families and carers, and ensuring access to support nationally.
The Strategy was composed of three stages.
The Foundations stage, covering the first two years of the programme. This stage had goals centred around ensuring access. This included access to post-diagnostic services, autism-specific services, and mainstream services where appropriate.
The Whole Life Journey stage, covering the first five years of the programme. This stage considered integrated service provision across a longer timespan to address the multidimensional aspects of autism (such as transition planning, education, health and social care and mainstream services).
The Holistic Personalised Approaches stage, covering the entirety of the ten years. This stage focused on meaningful national-local partnerships, creative use of budgets, and the extension of care and support into older age.
There was a specific focus on the need for local autism strategies, acknowledging that 'the needs of people with autism spectrum disorder and carers [should be] reflected and incorporated within local policies and plans.' Of the £13.4 million pledged between 2011 and 2014, £4.89 million was allocated to individual projects via the Autism Development Fund, and a further £1.12 million was committed to support the development of action plans in local authorities. The Strategy emphasised the need for these strategies to be hosted across multiple agencies (including health, social care, and education), and for those working on them to have the requisite training and knowledge to work with autistic people.
The Strategy was refreshed in 2015 and again in 2018, with additional funding from the Scottish Government of approximately £2.5 million between 2015 and 2021 allocated to individual projects via the Autism Innovation and Development Fund, and the Understanding Autism Fund. The focus was reframed onto four key outcomes.
A Healthy Life: 'Autistic people enjoy the highest attainable standard of living, health and family life and have timely access to diagnostic assessment and integrated support services.'
Choice and Control: 'Autistic people are treated with dignity and respect and services are able to identify their needs and are responsive to meet those needs.'
Independence: 'Autistic people are able to live independently in the community with equal access to all aspects of society. Services have the capacity and awareness to ensure that people are met with recognition and understanding.'
Active Citizenship: 'Autistic people are able to participate in all aspects of community and society by successfully transitioning from school into meaningful educational or employment opportunities.'
Initiatives funded under the Healthy Life strategic outcome included the creation of the National Autism Implementation Team, and the National Post Diagnostic Support Programme. Similarly, the Scottish Women's Autistic Network was established using funding from the Choice and Control strategic outcome.
A review of this phase of the Strategy was conducted in 2021, to mark the end of the ten year programme. It found that:
'most of the commitments in the strategy have been actioned to some extent, some have gained more traction than others and some still need much more focus and investment for real progress to be realised.'
Scottish Government, Scottish Strategy for Autism: evaluation, 2021
However, the review also noted that:
'real change for many autistic people, both in how they engage with services and in how they are supported to live productive lives, is not as evident'.
Scottish Government, Scottish Strategy for Autism: evaluation, 2021
Another review of the Strategy, published by the Cross-Party Group on Autism, also found that there was:
widespread frustration that the aims of the strategy have often not been put into practice or realised at a local level
Cross-Party Group on Autism, The Accountability Gap, 2020
In March 2021, the Scottish Government published a learning/intellectual disability and autism transformation plan, covering 2021-2023. The grouping of autism with learning/intellectual disabilities reflects the high rate of co-occurrence of these conditions, with the plan estimating that over 30% of autistic people also have a learning/intellectual disability. One of the motivators of the new strategy was the impact of the Covid-19 pandemic on autistic people and people with learning/intellectual disabilities, particularly in relation to:
mental health
health and social care services
employment
education
digital exclusion
communication.
The plan sets out thirty-two actions to help improve the lives of autistic people and people with learning/intellectual disabilities in these areas. It led to the development of the Learning Disabilities, Autism and Neurodivergence (LDAN) Bill.
National Autism Implementation Team
One of the key outcomes from the final phase of the Scottish Strategy for Autism was the creation of the National Autism Implementation Team (NAIT), a partnership between practitioners and researchers hosted at Queen Margaret University, Edinburgh. The team works to implement evidence-informed practice in the assessment of autism and other neurodevelopmental conditions, and carries out peer-reviewed research in this field. Much of their work involves working with health boards and Health and Social Care Partnerships across Scotland to implement neurodevelopmental services for children and adults. They have also produced an array of resources to assist in the areas of education, inclusive practice, assessment and diagnosis, employment and implementing neurodevelopmental pathways.
One of NAIT's first pieces of work was their National Clinical ADHD Pathway Feasibility Study. This study was commissioned by Scottish Government in order to determine how best to implement a national ADHD pathway. Among its conclusions was the recommendation that:
Scottish Government should endorse the development of adult neurodevelopmental approaches (which would complement children and young people's neurodevelopmental approaches for a coherent national approach to this lifelong condition).
National Autism Implementation Team, National Clinical ADHD Pathway Feasibility Study, 2021
Another key recommendation was that the Scottish Government should endorse a whole-system approach to improving the outcomes for neurodivergent people, including education, employment and the third sector as well as primary, secondary and tertiary care. They also supported the implementation of:
a programme of education, training and research for a) secondary mental health services, b) the multi sector workforce in support of the whole system approach.
National Autism Implementation Team, National Clinical ADHD Pathway Feasibility Study, 2021
NAIT's further work has included the establishment of a children's neurodevelopmental pathway network, set up in 2021. In 2024, they published a guide to the implementation of these pathways across Scotland. They also published an Adult Neurodevelopmental Pathways report in March 2023. This surveyed the provision of neurodevelopmental pathways across the fourteen territorial health boards in Scotland. In this study, NAIT also worked with four 'pathfinder' health board areas (NHS Borders, NHS Lanarkshire, NHS Highland and NHS Fife) and used funding from the Mental Health Recovery and Renewal Fund allocated to those areas to understand the major requirements and barriers to developing adult neurodevelopmental pathways nationally.
The major conclusions drawn from this work are listed below.
Diagnosis is extremely valuable to neurodivergent people. The Adult Pathways report concluded that 'living as a neurodivergent adult without a diagnosis often has a negative impact on mental health and wellbeing and participation in daily life'. However, fundamentally, support should be provided according to need and not diagnosis.
Co-occurrence of neurodevelopmental conditions (such as autism and ADHD) is common, and single condition pathways can lead to wasted resources and longer waiting times for diagnosis and support.
Current provision of adult neurodevelopmental pathways is inadequate. The report found that in 2021, only one of the fourteen Scottish territorial health boards provided both autism and ADHD assessments for adults.
All territorial health boards had child autism and ADHD pathways as of 2021, and either had or were developing overarching neurodevelopmental pathways for children. However, only seven health boards had implemented these pathways as of 2024, and the other seven were still in the process of developing such pathways.
In addition, the report made a set of ten recommendations to improve the provisions for neurodivergent adults in Scotland.
Recommendation 1: An adult neurodevelopmental pathway strategy and planning group to be hosted in all Health and Social Care Partnerships.
Recommendation 2: Support to develop local Neurodevelopmental Pathway action plans.
Recommendation 3: Establish a Neurodiversity Affirming Community of Practice.
Recommendation 4: A focus on ‘Post Diagnostic Support’ or ‘Support before, during and after diagnosis’.
Recommendation 5: Build a Neurodevelopmentally Informed workforce in Scotland.
Recommendation 6: Development of Adult Neurodevelopmental Pathway standards and guidelines for assessment, diagnosis and support.
Recommendation 7: Understand demand and capacity within the system, to meet the needs of neurodivergent adults.
Recommendation 8: Neuroinclusive Further Education and Employment environments.
Recommendation 9: Build a shared expectation that support should be available at any stage for people who identify as neurodivergent.
Recommendation 10: Seek to understand the changes needed to effectively meet the mental health needs of neurodivergent people.
The Scottish Government has since stated that
...we are funding and working with...NAIT to take forward the recommendations of its 2023 report. Support from NAIT is being given directly to health and social care partnerships to develop action plans, introduce adult neurodevelopmental pathways and provide professional learning workshops. We are funding a new neuro-affirming community of practice, which was launched in October 2023, and there has been positive engagement across health boards with that
Minister for Social Care, Mental Wellbeing and Sport, Portfolio Questions, 8 May 2024
NAIT has also published a range of resources for practitioners, which are available on their website.
National Neurodevelopmental Specification for Children and Young People
In 2021, as recommended by the Children and Young Person's Mental Wellbeing Taskforce the Scottish Government published the National Neurodevelopmental Specification for Children and Young People. This document set out the standards of care and service that children and young people with neurodevelopmental requirements should expect to receive in Scotland. This is not limited to health services, and applies to education and community services as well. It also sets out that no diagnosis should be required to access such support. This policy sits alongside the Child and Adolescent Mental Health Services (CAMHS) NHS Scotland National Service Specification, and aims to enhance the provision for neurodivergent children above and beyond what is set out in the CAMHS specification.
The National Neurodevelopmental Specification lays out seven broad standards of care. These are:
Neurodevelopmental services in Scotland will provide high quality care and support that is right for the patient.
The patient is fully involved in decisions about the patient's care.
The patient will receive high quality assessment, formulation and recommendations that are right for the patient.
The patient's rights are acknowledged, respected and delivered.
The patient is fully involved in planning and agreeing the patient's transitions.
Children, young people and their families and carers are fully involved.
The patient has confidence in the staff that support the patient.
The Specification further breaks down each of these standards into specific sections. No such document exists for adults, although the NAIT have recommended the creation of a corresponding adult neurodevelopmental specification. A review of the implementation of the Specification has been carried out by Scottish Government, and is due to be published in June 2025.
Funding summary
There are a number of funding mechanisms to support neurodivergent people in Scotland.
The Scottish Budget for 2025-26 allocated an additional £270.5 million to mental health services, which will be in addition to spending by individual health boards on mental health services. In 2023-24, a total of £1.5 billion was spent on mental health services, equivalent to 9% of total NHS expenditure.
In the Programme for Government 2025-26, the Scottish Government reiterated a pledge of £123.5 million of recurring funding to improve mental health support for young people, including clearing CAMHS backlogs.
This funding is directed in the first instance to NHS boards, but the mode of delivery of neurodevelopmental pathways varies by area. In some cases, the pathways are hosted within Health and Social Care Partnerships (HSCPs), which are commissioned by the Integrated Joint Boards. This is the case in areas where adult neurodevelopmental pathways are hosted within Community Mental Health Teams (CMHTs), which themselves are part of the HSCPs. On the other hand, in areas where a health board-wide neurodevelopmental pathway exists, this is delivered by the health board directly.
Following the publication of the national neurodevelopmental specification, over £1 million was allocated to five regions (Aberdeen City, East Lothian, Fife, Highland and Stirling) to carry out 'tests of change' designed to explore elements of the specification. A report on this project will be published in the summer of 2025.
In addition, more recent funding totalling almost £250,000 was provided to a number of individual projects aimed at improving support and assessment, including testing of digital assessment tools, and to the Fife and East Lothian 'test of change' sites.
For neurodivergent adults, the Autistic Adult Support Fund allocated £1.5 million from 2023-2025 to fifteen organisations that work with autistic adults in Scotland, and will provide a further £2.5 million in the period 2025-2028. This was a continuation of the National Post-Diagnostic Support Programme that ran from 2020-2023.
The Scottish Government continues to fund the National Autism Implementation Team.
NHS Education for Scotland will receive £648.9 million of funding in 2025-26 and delivers education and training for all people working in NHS Scotland. This includes training of health professionals to diagnose and support people with neurodevelopmental conditions.
Proposed and future policy developments
In addition to existing policies, the Scottish Government has consulted on a new bill to improve the lives of neurodivergent people and people with learning disabilities. This section sets out detail on the proposed Learning Disabilities, Autism and Neurodivergence Bill.
Learning Disabilities, Autism and Neurodivergence Bill
In March 2021, the Scottish Government and Convention of Scottish Local Authorities published the learning/intellectual disability and autism transformation plan. This was in response to the end of the Scottish Strategy for Autism and the Keys to Life strategy, the Scottish Government's strategy to improve the quality of life of people with learning disabilities. The timing of the transformation plan's publication also coincided with increased awareness of the heightened challenges faced by autistic people and people with learning disabilities since the pandemic. These challenges included:
barriers to access to health and social care brought about by the pandemic
deteriorating mental health brought about by isolation due to national lockdowns
digital exclusion
fears of unemployment
lack of support for transitions in education.
The transformation plan set out a list of thirty-two actions, including the consideration of a Commission or Commissioner to help protect people's rights. In response to these proposed actions and extensive campaigning by third sector organisations, the Scottish Government conducted scoping work for the Learning Disabilities, Autism and Neurodivergence (LDAN) Bill in 2022. It was anticipated that this Bill would provide a broad approach to covering learning disabilities and neurodivergence, following on from previous strategies on a national level. It was also the intention of this Bill to broaden these provisions to cover all neurodivergent people, on both a local and national scale. Following the scoping paper, further goals were set out, including to improve awareness and understanding of these conditions, deliver better training, increase the use of inclusive communication, better collect and report data on these groups, and promote independent advocacy.
The scoping phase for this proposed Bill engaged with 18 different organisations across 30 events, and the findings were published in 2023. The key takeaways included the following:
Participants felt that such a bill was needed to primarily address the discrimination facing people with learning disabilities, autism and neurodivergent presentations, and protect them from such discrimination. This should be done through education and training, both for public bodies and for neurodivergent people themselves.
They also felt that the bill should cover a wide range of people, and the definition of what makes a person neurodivergent needed to be made more clear and formal.
There was consensus that any bill should cover people without a formal diagnosis of learning difficulties, autism, or any other neurodevelopmental condition, and that the bill should cover the full range of neurodivergent presentations. However, some participants were concerned that too broad a scope would not effectively target the needs of any individual or group.
The length of waiting times for diagnosis was an issue of major importance.
The next stage in the development of the Bill was consultation, which took place in December 2023-April 2024. The Lived Experience Advisory Panel (LEAP), a group of approximately twenty-five people with conditions such as learning disabilities, autism, ADHD, dyslexia and Down's syndrome, helped to co-design the consultation. Feedback from the consultation was collected and analysed in order to inform the next stages of the Bill's progression. The issue of diagnosis was not included in the consultation.
However, in September 2024, the Minister for Social Care, Mental Wellbeing and Sport announced that the Scottish Government was not planning introduce the LDAN Bill in the parliamentary year 2024-2025. Instead, it intended to develop and publish draft bill provisions, taking on board the feedback from the consultation analysis. The announcement cited three reasons for this delay.
There were 'strong and diverse views' expressed in the consultation analysis on many of the key issues, which the Scottish Government would need to work through before going forward.
There was a need to wait for the results of the Scottish Parliament's inquiry into the Commissioner Landscape in Scotland before proceeding. The report on this inquiry was published in September 2024, and called for a pause on creating any new Commissioner roles until a 'root and branch review' of the existing Commissioner structure is carried out. This would include the creation of any Commissioner via the LDAN Bill. A dedicated committee was subsequently set up to explore the issue further and reported in June 2025. This Committee recommended that no new advocacy-type SPCB supported bodies should be created and set out new criteria for the creation of any new Commissioners.
The legislative landscape in this areas was fast-changing, with the National Care Service (Scotland) Bill (now the Care Reform (Scotland) Bill) and Human Rights Bill both under consideration. However, the National Care Service Bill encountered delays in the parliamentary year 2024-2025 and the scope changed considerably during scrutiny before its approval in June 2025. The Human Rights Bill has also been pushed back a number of times and will no longer be taken forward in the current parliamentary session.
The Equalities, Human Rights and Civil Justice Committee held two evidence sessions on the delay, on 26 November 2024 and 3 December 2024, and also undertook engagement with six autistic disabled people's organisations on 25 March 2025.
Current provision of neurodevelopmental pathways in Scotland
This section outlines the current neurodevelopmental pathways available to adults and children in Scotland. It begins by outlining the key stages of the pathway, from the point of initial contact to the sharing of the diagnosis with the patient. It then goes into the detail of how the process works in each NHS board, and what support and services are available in each area. It finishes with a summary of other support and provision for neurodivergent people, including in social security, social care, education, employment and through the third sector.
Neurodevelopmental pathways for children and adults by health board
The delivery of neurodevelopmental pathways in Scotland is managed by the NHS territorial health boards and the Health and Social Care Partnerships (HSCPs). In particular, the pathways for children should be embedded within the Getting It Right For Every Child (GIRFEC) framework. The exact mode of delivery varies by health board, but the pathways can be divided broadly into the following stages, according to the National Autism Implementation Team (NAIT) and Scottish Intercollegiate Guidelines Network (SIGN) guidelines.
Identification of needs. Once a family member, teacher, GP or the neurodivergent person themself decides that a neurodevelopmental assessment might be useful, they should be offered a first, pre-referral appointment as soon as possible. The National Neurodevelopmental Specification states that this should be within four weeks at most for a child or young person.
Pre-referral appointment. This is usually done by schools, health visitors, allied health professionals or GPs, and determines whether a formal neurodevelopmental assessment is necessary. In these appointments, patients may be screened using questionnaires about their behaviour and family history. NAIT has compiled a list of suitable questionnaires and tools, which include the ESSENCE-Q and DAWBA, that can be administered by a range of people including parents and carers. One pilot study in Lanarkshire suggested that moving towards a model in which these tools are used more widely and earlier in the neurodevelopmental pathway could significantly reduce waiting times and pressures on assessment teams. If the team carrying out this appointment decides that a neurodevelopmental assessment is necessary, they refer the patient to the assessment service. However, if the patient meets the criteria for referral to Child and Adolescent Mental Health Services (CAMHS) or adult mental health services due to a co-occurring mental health condition, they are referred to these services instead. In some areas (such as NHS Highland, where the children's neurodevelopmental service operates on an open referral system) not all patients are offered a pre-referral appointment.
Triage and allocation. Once the assessment team receives a referral, they check that the referral meets the criteria and put the patient on the waiting list for an appointment. NAIT propose that the time between referral and first appointment should be no longer than 84 days/12 weeks. NAIT also makes a distinction between 'core' cases, for which the local multi-disciplinary team can complete the assessment in 1-2 appointments, and 'complex' cases which require the attention of a specialist team and may take longer to complete. NAIT have published a guide to complexity in neurodevelopmental assessments that covers this issue in more detail.
Assessment appointment(s). The formal assessment process can take many appointments, depending on the complexity of the case. In general, these consist of two key components. The first is information gathering through interview-style discussions with the patient and their family. The second is direct observation of the patient and their behaviours, sometimes in a range of environments. For example, where a child presents differently at school as opposed to at home, it can be appropriate to arrange in-school and at-home observations. Specialist multi-disciplinary assessment teams carry out these observations and discussions.
Diagnosis. Once the multi-disciplinary team has gathered the relevant information, the assessment team will reach a judgement as to the diagnosis of the patient. This is done against a standard set of criteria, such as the DSM-5 or ICD-11. Patients may be diagnosed with one or more neurodevelopmental conditions, or none at all. The team making the assessment may also diagnose co-occurring mental health conditions.
Sharing the diagnosis. Finally, the team shared the diagnosis with the patient, their family and other groups (such as the school, GP, or social care services). The patient may be signposted to further post-diagnostic support, either within the NHS or via the third sector.
More information about the various methods and tools used in the pathway can be found in NAIT's Children's Neurodevelopmental Pathway Practice Framework and Adult Neurodevelopmental Assessment Workbook.
The provision of these services varies between the NHS Scotland territorial health boards. Services such as Child and Adolescent Mental Health Services (CAMHS) and Community Mental Health Teams (CMHTs) may be involved, but some health boards have separate neurodevelopmental assessment teams. Table 3 below summarises the information available about neurodevelopmental pathways online, as well as the responses to the Health, Social Care and Sport Committee's letter of March 2025. This may not reflect the full range of services available in each health board. Detailed information about the neurodevelopmental pathways for children and adults in each health board is provided in Annex A.
| Health Board | Child Neurodevelopmental Pathway | Adult Neurodevelopmental Pathway |
|---|---|---|
| NHS Grampian | Neurodevelopmental assessments available through CAMHS (for those meeting criteria) or Community Child Health (Paediatrics). | Adult Autism Assessment team in operation in Moray and Aberdeen City HSCP, but no longer in Aberdeenshire HSCP. This is an autism assessment service only, with plans to move to a broader neurodevelopmental service. A small ADHD assessment team exists in Aberdeen City HSCP. |
| NHS Tayside | As of March 2025, was not accepting new referrals for neurodevelopmental assessments unless the patient had a co-occurring mental health condition and met the criteria for referral to CAMHS. | ADHD referrals made to Community Mental Health Teams but must meet the criteria for referral to secondary mental health services. Tayside Adult Autism Consultancy Team carries out adult autism assessments. |
| NHS Highland | Neurodevelopmental assessments carried out by a Neurodevelopmental Assessment Service (NDAS). | There are separate adult autism and ADHD pathways. Adults do not need to meet the criteria for referral to secondary mental health services to access these. ADHD pathway was not taking new referrals as of October 2023 unless the patient met the criteria for referral to secondary mental health services. |
| NHS Orkney | Neurodevelopmental service exists outside CAMHS, although no information is available about how the pathway works. | Assessments outsourced to a private healthcare provider, although a neurodevelopmental service is under development. |
| NHS Shetland | Assessments available through CAMHS, Community Paediatrics and Speech and Language Therapy services. Patients do not need to meet the criteria for referral to CAMHS to access these services. | Adult Autism Assessment Pathway is managed by Speech and Language Therapy services, currently paused due to funding issues. |
| NHS Western Isles | Overarching neurodevelopmental assessment is available. | Neurodevelopmental service is available, although ADHD assessment not yet incorporated. |
| NHS Lothian | Neurodevelopmental pathway exists in all HSCPs, although mode of delivery varies between individual HSCPs. | Overarching neurodevelopmental pathway within the Community Mental Health Teams. Patients do not need to meet criteria for referral to secondary mental health services to access this. |
| NHS Forth Valley | Neurodevelopmental assessments available through CAMHS or Paediatric Neurodevelopmental Services. | The Adult Autism Assessment Team, which carried out assessments for those who do not meet the criteria for referral to secondary mental health services, was disbanded in March 2025. |
| NHS Borders | There is an overarching neurodevelopmental assessment service (Borders Autism Team) hosted within CAMHS that is available even if patients do not meet the national criteria for referral to CAMHS. | No service available for those seeking diagnosis who do not meet the criteria for referral to secondary mental health services. |
| NHS Fife | Overarching neurodevelopmental assessment is available through the Fife Neurodevelopmental Pathway. | Neurodevelopmental assessments are only available for those that meet the criteria for secondary mental health services. |
| NHS Greater Glasgow and Clyde | Overarching neurodevelopmental assessment is available for children who do not meet the criteria for referral to CAMHS. | The Adult Autism Team (AAT) operates within the Community Mental Health Teams, and provides autism assessments for adults who do not meet the criteria for referral to secondary mental health services. ADHD assessments are carried out within each of the six HSCPs. |
| NHS Lanarkshire | Neurodevelopmental assessments come through the NHS Lanarkshire Neurodevelopmental Service, or through CAMHS if the patient meets the referral criteria. | There is a recently established Adult Neurodevelopmental Service, which provides autism assessments to all adults. Unclear whether an adult ADHD pathway exists. |
| NHS Dumfries and Galloway | NHS Dumfries and Galloway operate a Neurodevelopmental Assessment Service for Children and Young People (NDAS) with an open referral system. | No adult neurodevelopmental pathway for those who do not meet the criteria for referral to secondary mental health services. |
| NHS Ayrshire and Arran | Neurodevelopmental assessments are available to those meeting CAMHS or community paediatrics referral criteria only. | No operational pathway for adult neurodevelopmental assessments, and no longer accept referrals. |
Referral to CAMHS or adult mental health services
Specialist neurodevelopmental pathways are not the only route for neurodivergent people to be assessed for neurodevelopmental conditions. If a child meets the criteria for referral to Child and Adolescent Mental Health Services (CAMHS), they should be accepted into this service rather than be referred to a neurodevelopmental pathway. CAMHS are for
children and young people age 0 – 18th birthday with clear symptoms of mental ill health which place them or others at risk and/or are having a significant and persistent impact on day-to-day functioning.
Scottish Government, Child And Adolescent Mental Health Services: National Service Specification, 2020
These criteria mean that neurodivergent children with co-occurring mental health conditions should be seen within CAMHS. Specialist CAMHS units routinely carry out neurodevelopmental assessments, and these assessments form part of the broader mental health care services the patient receives. However, these services are not accessible to the majority of children seeking a neurodevelopmental assessment. The children's neurodevelopmental pathways surveyed in the following sections are specifically for children who do not meet the CAMHS referral criteria, and mostly exist outside CAMHS. There is very limited data about the number of children referred within CAMHS, and how long they wait for an assessment.
Similarly, adults with co-occurring mental health conditions will often meet the conditions for referral to secondary mental health care services. In most areas, Community Mental Health Teams (CMHTs) deliver these services. There is no nationally standardised set of criteria for referral to CMHTs. Instead, these are set locally within each NHS board. For example, in NHS Highland the Adult CMHT will consider referrals from primary, secondary and tertiary care of
people presenting with mental disorder of significant clinical severity and complexity associated with significant risk and/or significant functional impairment.
NHS Highland, Community Mental Health Team (CMHT) (Guidelines), 2025
As with the CAMHS criteria, this excludes many of the people seeking a neurodevelopmental assessment, who do not have a co-occurring mental health condition. NHS Highland note explicitly that:
The Adult CMHT cannot provide assessment for new diagnosis of Autistic Spectrum Disorder in the absence of comorbid moderate to severe mental illness / disorder.
NHS Highland, Community Mental Health Team (CMHT) (Guidelines), 2025
As a result, the adult neurodevelopmental pathways surveyed in the following sections are specifically for adults who do not meet the CMHT referral criteria, and mostly exist outside the CMHTs.
Private neurodevelopmental assessment
Due to the long waiting times for neurodevelopmental assessments, there is an increasing demand for private neurodevelopmental assessments for both adults and children. The closure of assessment services in some health boards has led to even more neurodivergent people seeking a private assessment. These are available through a number of organisations in Scotland, and are regulated through Healthcare Improvement Scotland. The main advantage of such assessments is that waiting times are often much shorter. Quantitative data on waiting times is scarce, but one clinic in England that provides both private assessments and assessments on behalf of the NHS suggests waiting times for private assessment can be as little as 8 weeks, while those funded by the NHS take 9-18 months.
Private neurodevelopmental assessments in Scotland cost in the range £1500-£450012345, although costs are slightly lower for condition-specific assessments (e.g. those assessing for ADHD or autism only)6. Many neurodivergent people report that the cost of private assessment causes them to incur significant financial hardship5.
If they meet NHS gold standards, private diagnoses for neurodevelopmental conditions may be accepted as equivalent to an NHS diagnosis. However, the decision to accept such diagnoses lies with the GP. In the case of ADHD, where diagnosis may lead to the prescription of medicines, the patient may wish to enter a shared care agreement, under which the medication may be prescribed by the NHS GP, rather than the private specialist. Whether or not the GP agrees to this arrangement depends on a number of factors including specific health board guidance, quality of diagnosis, the nature of any other medication the patient may be taking, and the GP's own workload. Guidance for such agreements has been issued by the General Medical Council, the Scottish Government and some health boards.Shared care agreements are discussed in more detail in the issues section.
Other support available
A crucial aspect of the experience of neurodivergent people is the support available outside the NHS. A range of support is available for those who have not yet obtained a diagnosis (or are not seeking one), although the provision of this support is highly variable across Scotland. Given the increasing demand for neurodevelopmental support, this is more important than ever. Even for those who have received a diagnosis, support outside the NHS is critical, as post-diagnostic support from NHS services is minimal in some areas. In this section, we will look at support that does not require a formal diagnosis to access.
Therapies
One of the services that does not always require a formal diagnosis to access is therapy. This can include occupational therapy, speech and language therapy and cognitive-behavioural therapy.
Occupational Therapists (OTs) help people overcome physical and mental challenges related to completing everyday tasks. These tasks could be learning activities, leisure activities, or simply the day-to-day process of looking after oneself. They also have an important role in implementing and supporting environmental modifications to make the neurodivergent person more comfortable across a range of settings. This can be at home, in education or in employment. OTs also support the people around a neurodivergent person to understand and adapt to their communication and sensory preferences.
This sort of therapy can be invaluable in helping neurodivergent children and adults. One study found that occupational therapy 'significantly improves sensory skills, relationship-building abilities, body and object usage, language skills and social and self-care skills' in autistic children1, and another concluded that 'occupational therapists have much to offer in providing interventions for adults with ADHD'2. All fourteen NHS boards in Scotland have occupational therapy services for both children and adults, and occupational therapists in Scotland are supported by organisation such as the Royal College of Occupational Therapists.
Speech and Language Therapists (SLTs) work with neurodivergent people in a similar way to improve their verbal, non-verbal and social communication. Autistic people in particular often struggle with speech, and evidence has shown that speech and language therapy is a highly effective method of helping autistic children to improve their communication3. As with occupational therapy, speech and language therapy is available from all NHS boards in Scotland, and private services are also available4.
Guidance suggests that OTs and SLTs should also be core members of the multi-disciplinary teams that carry out neurodevelopmental assessments, and there have been calls for this role to be expanded.
Cognitive Behaviour Therapy (CBT) is another tool that can help neurodivergent people learn how their feelings, emotions and thoughts influence each other. It teaches coping skills to deal with difficult and unfamiliar thoughts that neurodivergent people may have. If successful, it can improve the focus and social skills of neurodivergent people in various situations56. However, other research suggests that some neurodivergent people see CBT as unhelpful and damaging7, as it encourages masking of behaviours and doesn't fall within the neuro-affirming paradigm. CBT is less widely available through the NHS in Scotland than SLT and OT, but there are many third sector and private organisations offering these services.
As with neurodevelopmental assessment services, there is a high demand for these services in Scotland. While advice and support is available over the phone in some health boards, waiting times for accessing specialised individual support can be months or years in some cases. Referrals can be made by GPs, schools and health visitors, but self-referrals are also accepted.
Third sector support
The third sector - encompassing charities, social enterprises and community groups - plays an important role in supporting neurodivergent people. While most third sector organisations cannot provide clinical support such as neurodevelopmental assessments, they are able to provide important services for people who are not seeking a diagnosis, people on waiting lists and people who have already received a diagnosis. Some of the national third sector organisations in Scotland are listed below.
Charities such as National Autistic Society Scotland and Scottish Autism provide 'a range of services and support for Scotland's 56,000 autistic people and their families, and campaign at a national and local level to help create a society that works for autistic people'. These services include support in employment and the workplace, social care/supported living, specialist education services, social programmes, outreach work, peer support, parent education programmes and information services across Scotland.
Autism Initiatives runs programmes for adults diagnosed with autism in Scotland, funded by the Scottish Government's Autistic Adult Support Fund. Following the success of the first round of funding to 15 organisations in 2023, a further £2.5 million was allocated to this fund in April 2025.
Scottish Women's Autistic Network (SWAN) is a charity delivering 'services, information and support for and by autistic women, girls and non-binary people across Scotland'. It runs training to increase awareness and understanding of autism in women, girls and non-binary people, as well as in-person and online social activities for these groups.
DIFFERabled, Mindroom, Barnardo's and The Donaldson Trust are examples of charities that offer services, wellbeing therapies and learning opportunities to promote understanding and inclusion of neurodivergent people in Scotland.
The Scottish ADHD Coalition coordinates local organisations providing support to children and adults with ADHD in Scotland.
In addition to these national charities, there are numerous local organisations offering similar support and services. These are generally signposted on the NHS board and HSCP websites1, on NHS inform2, and on the websites of the larger third sector organisations3.
For autistic people specifically, there exist a number Autistic People's Organisations that work with people in Scotland. These include SWAN, Autistic Mutual Aid Society Edinburgh (AMASE), Autism Rights Group Highland (ARGH), Scottish Ethnic Minority Autistics (SEMA), Diversified and Autistic Knowledge Development (AKD). These organisations are led and run by autistic people, and are particularly important in empowering and advocating for autistic people.
Local organisations are often connected to the local Health and Social Care Partnerships (HSCPs), and in areas such as Fife receive funding from the HSCPs4. Mechanisms like these are generally regarded as examples of good practice. Neurodivergent people often report better experiences when working with third sector organisations, as they do not agree with the clinical understanding of autism as a medical problem. This reasoning has prompted suggestions that the third sector should play a larger and more formalised role in redesigned neurodevelopmental pathways.
Local authorities and education
The role of local authorities in supporting neurodivergent children falls under the umbrella of the Getting It Right For Every Child (GIRFEC) policy. GIRFEC was enshrined in law by the Children and Young People (Scotland) Act 2014, and is the Scottish Government's programme for promoting, supporting and safeguarding the wellbeing of children and young people in Scotland.
While the GIRFEC policy does not make specific reference to neurodivergent people, their wellbeing falls under the umbrella of this policy, and so the neurodiversity pathways should work in tandem with GIRFEC policy. This is also set out in the Children's Neurodevelopmental Pathway Practice Framework document published by the National Autism Implementation Team. In this document, it is proposed that local authorities have an important role in the pre-referral stage of the neurodiversity pathway, as this often occurs in an educational setting. The GIRFEC framework also specifies that any support a child receives should not be dependent on diagnosis.
Within an educational environment, local authorities have legal obligations in relation to identifying and meeting additional needs under the Education (Additional Support for Learning) (Scotland) Act 2004. If a child has complex needs that require coordination and support from other public services such as social work or healthcare services, then a coordinated support plan must be made. No formal diagnosis is required for such a plan to be made.
In addition, under the Scottish Strategy for Autism, best practice in the provision of effective services for autistic people includes a local autism strategy. Under the Public Bodies (Joint Working) (Scotland) Act 2014, the local Health and Social Care Partnerships (HSCPs) have a duty to produce a strategic plan to address the needs of the local population. While neurodivergent people fall under this strategy, a survey found that, as of 2024, specific plans for autistic people and people with ADHD were not universally implemented. These plans include social care, education, housing, employment, and community-based services.
Support for neurodivergent people in further and higher education settings can also be very important. Given that neurodivergence often goes undiagnosed in childhood, some neurodivergent people may only realise that they might have a neurodevelopmental condition when they leave the supportive environment of home and school. Some universities in Scotland are actively taking steps to support neurodivergent students at this important transition point. In England, some universities host specialist neurodevelopmental assessment services for students, although this has not yet been implemented in any Scottish institutions.
Employment
Neurodivergent people face significant challenges in entering employment and in the workplace. The Buckland Review of Autism Employment highlighted some of the challenges facing autistic people in particular.
Autistic people have a lower employment rate (roughly three in ten people) than disabled people generally (five in ten), and the largest pay gap among all disabled groups.
Autistic people experience barriers to obtaining and succeeding in work. These include poor preparation by employers, unfair hiring practices, unclear work processes, outdated attitudes, and lack of access to work experience or careers advice.
Autistic people have a very negative experience in both the hiring process and in maintaining long-term employment.
More broadly, during the consultation on the LDAN Bill some members of the Lived Experience Advisory Panel claimed that workplaces are often
not neurodivergent and disability-conscious, or adaptive to people's needs...there is a lack of clarity on what reasonable adjustments are and look like in individual circumstances.
Scottish Government, Learning Disabilities, Autism and Neurodivergence Bill: Consultation, 2023
Similarly, a study by the National Autism Implementation Team found significant stereotyping of autistic people in the workplace, leading to many autistic people not disclosing their diagnosis. They concluded that
Autistic professionals face inequalities and unsupportive environments...there is a need for culture change within public sector education and health workplaces to improve accessibility
National Autism Implementation Team, Learning from the Experiences of Autistic Professionals Working in Health and Education, 2025
It also found that acceptance and inclusion are important to autistic people in the workplace, and even minor changes to the environment and communication in the workplace could lead to better outcomes.
Social care
Neurodivergent people with more acute needs may rely on social care to support their day-to-day life and wellbeing. Health and Social Care Partnerships (HSCPs) supply and manage social care locally. The assessment of whether an individual requires social care is carried out on a case-by-case basis, and no formal diagnosis of a neurodevelopmental condition is required. If it is decided that a neurodivergent person is eligible for social care, they have four options under the Social Care (Self Directed Support) (Scotland) Act 2013.
Option 1: The local authority makes a direct support payment to the neurodivergent person, or a third-party who is providing support.
Option 2: The neurodivergent person decides what support they would like, and the local authority arranges the support.
Option 3: The local authority arranges the support, after discussion with the supported person.
Option 4: A mixture of the above.
The Act also provides that the person receiving support has the right to be included in decisions about the support they receive and ask about or challenge any aspect of the support as well. It is felt in the neurodivergent community, however, that there needs to be better signposting of these opportunities to neurodivergent people. Neurodivergent people also feel that many of the services available to them before the Covid-19 pandemic have not returned since, which has led to increased loneliness and isolation. In some cases, neurodivergent people may require more intensive services, in the form of residential care or supported living services. A number of these are operated by third sector organisations such as Scottish Autism and the National Autistic Society.
The National Care Service (Scotland) Bill proposed the creation of a National Care Service, following recommendations coming from the Independent Review of Adult Social Care in Scotland in 2021. The Bill has encountered many delays and changes, and in February 2025 it was announced that many of the substantive sections on structural reform and accountability would be removed. The Bill was much reduced in scope and renamed as the Care Reform (Scotland) Bill, and was passed on 10 June 2025 and is currently waiting Royal Assent.
Social security
Neurodivergent children and adults in Scotland may be eligible to receive social security payments under the Child Disability Payment (CDP) and Adult Disability Payment (ADP) schemes respectively. These schemes, which provide financial support for the extra costs that disabilities may incur, are replacing the UK Government's Disability Living Allowance (DLA) and Personal Independence Payment (PIP). The Scottish Government is moving people who have previously received DLA and PIP payments from these schemes to ADP and CDP in 2025. The value of the payment is dependent on the level of support required, and consists of two parts:
a mobility part, paid at either a lower/standard rate (£29.20 per week) or higher/enhanced rate (£77.05 per week)
a care part, known as the daily living part under the ADP scheme. Under the CDP scheme, this is paid at either a lowest, middle or highest rate (£29.20, £73.90 or £110.40 per week respectively). Adults receive the payment at either a standard or an enhanced rate (£73.90 or £110.40 per week).
Some neurodivergent people are eligible to receive payment under these schemes. A formal diagnosis is not required to receive support. Instead, eligibility depends on the level of support assessed against set criteria. In addition to the application form, an applicant must submit at least one piece of supporting information from a professional confirming the needs and disability of the person claiming payment. Autism (55%) and ADHD (12%) were listed as the two most common primary disability conditions for children receiving CDP in March 2025.
People seeking support can submit such an application at any time, and payments continue as long as the person has the same needs. ADP is available from age 18, but children in receipt of CDP can apply for ADP between the ages of 16 and 18. Payments of ADP are made to the applicant unless there is an appointee to receive payments on their behalf. If someone gets the daily living component of ADP or the higher rate of care element of CDP, their carer may be eligible for Carer Support Payment. More details on application and eligibility can be found online.
The CDP and ADP schemes are not means-tested, meaning they can be paid regardless of financial position or employment status. However, given the rates of underemployment in this group, an increasing number of neurodivergent people are relying on payments from the UK Government such as the health element of Universal Credit (UC). Despite not needing a formal diagnosis to access these schemes, neurodivergent people do need to explain how their disability affects them and impacts their ability to work.
Many neurodivergent people find the rules and processes confusing, and there is uncertainty as to whether or not a diagnosis is needed to access social security benefits. In addition, there is concern surrounding the impact of the UK Government's plans for welfare reform, and how these will impact neurodivergent people. The proposed changes to the health element of UC will impact people in Scotland since UC is administered at the UK level. However, the proposed changes to the Personal Independent Payment (PIP) scheme will not affect people in Scotland as the equivalent social security payments are devolved.
Post-diagnostic support
In an effort to improve the provision of support for people diagnosed with autism, the Scottish Government funded a 6 month pilot programme of post-diagnostic support. This ran from December 2020 to May 2021, and was subsequently extended through to March 2023. The programme initially provided funding to seven different third sector organisations to provide a range of in-person and online support services. The groups were:
Autism Rights Group Highland (ARGH)
Autism Understanding Scotland (which has since shut down)
Services were available for adults and children who had received an autism diagnosis in the previous two years, as well as the families and carers of these people. In-person and online sessions aimed to improve understanding of autism and provide support when coping with crisis. The sessions also worked towards enhancing communication between autistic people, their carers and healthcare professionals.
The Scottish Government commissioned an evaluation of the pilot programme, which was published in March 2022. This found that, although obtaining a diagnosis had often been challenging and protracted, many autistic people felt that the diagnosis had been helpful in many ways. This included 'navigating future directions, connections, health and wellbeing, identity, education, and work'. In addition, these respondents reported a positive experience on the programme, boosting self-confidence and self-esteem, increasing connections with other autistic people, and reducing social isolation and anxiety.
On the basis of the success of the pilot programme, the Autistic Adult Support Fund was established in 2023, and allocated £1.5 million from 2023-2025 to fifteen organisations that work with autistic adults in Scotland. A further £2.5 million will be provided in the period 2025-2028. No equivalent funding has been made available for children, although the Scottish Government has continued to fund the National Autism Implementation Team and allocated funding to support the implementation of the National Neurodevelopmental Specification.
NAIT has also published a review of what support for neurodivergent adults is available across Health and Social Care Partnerships (HSCPs) in Scotland, before, during and after diagnosis, in addition to the support provided by the third sector. It found that:
access to support across Scotland for all neurodivergent adults before, during and after diagnosis is variable and often contingent on local agreements with third sector providers or is only available for individuals meeting a threshold for a particular service. Many neurodivergent people will not meet these thresholds or will fall between services.
National Autism Implementation Team, Support for Neurodivergent Adults in Scotland Before, During and After Diagnosis: A Scoping Review of Provision in Health and Social Care Partnerships, 2024
Similarly, autistic disabled people's organisations reported to the Equalities, Human Rights and Civil Justice Committee that:
the lack of good autistic-led pre- and post-assessment support continues to hamper our community...it must be acknowledged that this - like access to a good, neuroaffirming assessment - is a postcode lottery
Equalities, Human Rights and Civil Justice Committee, Learning Disabilities, Autism and Neurodivergence (LDAN) Bill: Engagement with Autistic Disabled People's Organisations, 25 March 2025
Proposal for alternative pathway
In January 2025, the Royal College of Psychiatrists in Scotland (RCPsychiS) published a proposal for the future of provision for people with neurodevelopmental conditions. This was in response to the dramatic increase in referrals for neurodevelopmental assessments in recent years, and the pressures this increase has put on mental health services (and on psychiatry in particular). In the proposal, RCPsychiS reports that:
Without a nationally agreed pathway in place for [neurodevelopmental conditions], the rapidly rising scale of need has had a critical impact on service capacity within secondary care mental health services. This has led to unprecedented pressures in the mental health sector and lengthy waits for assessment and treatment across all health board areas in Scotland - which is posing an existential threat to the mental health system.
Royal College of Psychiatrists in Scotland, The Future of Provision for Neurodevelopmental Conditions: Our Proposal, 2025
These pressures are reported to have a number of impacts.
Mental health services are overwhelmed, and waiting lists and times continue to rise.
General mental health and psychiatric services are suffering, as more resources are diverted to neurodevelopmental cases.
Undiagnosed and untreated neurodevelopmental conditions are having significant economic impacts, through loss of productivity and increased healthcare costs associated with untreated symptoms.
As a result, RCPsychiS proposed a new four-level neurodiversity pathway structure.
Level 1: National public health approach. The first stage of the proposal would be a national campaign to promote awareness and understanding of neurodiversity, with an emphasis on self-management. This would describe reasonable adjustments in education and in the workplace, provide educational resources for the public, and foster inclusivity and understanding.
Level 2: National self-help resources. This would create a 'centralised, national digital platform to provide comprehensive self-help resources for individuals with neurodevelopmental conditions'. These resources would be available for anyone who self-identifies as neurodivergent, and include psychoeducational materials, pre-recorded sessions and online information about neurodevelopmental conditions and how to mange them.
Level 3: Specialist third sector commissioning. This would be a national approach to commissioning third sector support and services to support at all stages of the diagnostic journey. This support should also be available for those who do not meet diagnostic thresholds, or do not wish to receive a diagnosis. Support would include establishing and maintaining peer support networks, and employability training.
Level 4: Neurodevelopmental teams. The final level of this new pathway would be referral to a specialised, multi-disciplinary neurodevelopmental team. These teams would include clinicians, to provide formal diagnosis and prescribe medication, as well as Allied Health Professionals such as therapists and nurses to support the day-to-day functioning of individuals with acute needs.
RCPsychiS suggest that such a pathway would significantly reduce the burden on clinicians and have modelled and costed their proposed structure. The total investment is estimated to be roughly £10 million per year to establish three or four 'regional hubs' in Scotland, with the majority of funding allocated to levels 2 and 3 in the pathway. According to RCPyschiS, further consideration should be given to the treatment of ADHD, as evidence suggests1 that patients with more complex ADHD presentations (e.g. those exacerbated by co-occurring conditions) respond less well to medication. This implies that a stepped care approach may not be appropriate in all cases. Further complications with ADHD arise due to the need for professionals with competency in medical evaluation to prescribe medication.
In addition, a letter was sent to the Health, Social Care and Sport Committee on behalf of the Child Heads of Psychology Services (CHOPS) (including CAMHS) in Scotland in April 2025. In this letter, CHOPS set out the need for a restructuring of neurodevelopmental pathways:
Without whole system consideration and radical systemic change, individual’s social, emotional, cognitive and developmental needs are not being adequately met, with associated systemic risks to these individuals, their families and carers, and to wider education, health and social care service provision.
Child Heads of Psychology Services in Scotland, Letter to the Health, Sport and Social Care Committee, 2025
They set out a list of recommendations for a new way forward, highlighting the work of NHS Fife's Neurodevelopmental model. Many of these recommendations are in line with RCPsychiS's recommendations for adult neurodevelopmental pathways. The key steps forward would involve:
a paradigm shift away from the historical medical model, to a needs-based, stepped and matched care approach within a public health lens
a multi-disciplinary and multi-agency model, led by psychology and allied health professionals (AHPs) and with a strong focus on whole systems ownership (community-based, education, applied psychology, health and social care)
increased use of digital resources, including a national platform with psychoeducational materials and increased use of digital assessment
a clear, national, competency-based framework for a stepped provision of services, with a specialist assessment pathway forming an important part of this framework but not at the heart of it
recognition of the importance of the AHP and educational psychology workforce
development of peer support systems for parents, carers, young people, and professionals
adhering to NAIT principles, particularly with regards to building a neurodevelopmental profile of the child.
Other recommendations made included:
a review and refresh of the National Neurodevelopmental Service Specification
any additional funding to be considered across agencies, as the issue does not only sit with Health and the solution is not to add more clinical capacity but to support the whole system in shifting to support neurodivergence.
a review of SIGN and NICE guidelines for assessment services
evaluation of community-based supports and equitable roll out of such supports where necessary
a national approach to developing digital resources for those waiting to be seen
consideration of a national electronic recording system, which adequately records relevant data across health boards.
Issues
In this section we will discuss other issues surrounding neurodevelopmental pathways and waiting times in Scotland.
Recent Scottish Parliament consideration
There has been significant recent interest in the issue of neurodevelopmental pathways and waiting times in Scottish Parliament. During the parliamentary year 2024-2025, this has included the following.
Petitions
PE2141: Support the neurodiverse community by providing funding for psychoeducation. This petition calls on the Scottish Government to 'improve the support available to the neurodiverse community, by providing fully-funded pyschoeducation and sensory aids'. Psychoeducation provides the information neurodivergent people, their families and friends need to understand their condition. At present, some psychoeducation resources are available in some neurodevelopmental pathways, both at the pre- and post-diagnosis stages, but this petition calls on wider availability and implementation. The petition suggests this would allow for greater community integration at both the pre- and post-diagnosis stage in existing neurodevelopmental pathways.
PE2148: Improve Child and Adolescent Mental Health Services to Adult Mental Health Services transition. This petition calls for a better transition between the two mental health services in Scotland, noting that 'not addressing this issue risks creating a lost generation that will cost more in the long term'. Transition between child and adult services is a key part to any neurodevelopmental pathway, and principles for this are outlined in the Transition Care Planning guidance published by the Scottish Government.
PE2156: Improve access to ADHD diagnosis and treatment across Scotland. This petition calls on the Scottish Government to a) develop a funded national ADHD strategy, b) standardise ADHD diagnostic pathways, reducing waiting times and c) ensure equitable access to ADHD diagnosis, treatment and support across Scotland. It references the halting of ADHD in some territorial health boards, and highlights the adverse impacts undiagnosed ADHD can have on patients.
Motions
Motion S6M-16644 was submitted by Daniel Johnson MSP. The motion expressed disappointment at the failure to announce the Learning Disabilities, Autism and Neurodivergence Bill in the 2024/25 Programme for Government, and called on the Scottish Government to 'provide clarity on its commitment to legislating in this area'. The motion was supported by four other MSPs.
Motion S6M-17670 was submitted by Alex Cole-Hamilton MSP. The motion called on Parliament to 'recognise the scale of the mental health emergency in Scotland', and touched on issues including the rise in demand for neurodevelopmental assessments, shortage of ADHD medication, pressures on health care services and funding for CAMHS and mental health services more generally. The vote was passed with a majority of 96 votes for, and 18 against.
Questions
A number of questions have been posed regarding waiting times (S6W-35533, S6F-03944, S6W-32900, S6W-31769, S6W-30907, S6O-04562, S6O-04617, S6W-37651, S6W-37316, S6W-37318,S6W-37317, S6W-38286), private diagnosis (S6W-36382, S6W-36384,S6W-32895, S6W-31032, S6O-04561, S6W-36383), and neurodevelopmental pathways (S6W-35334, S6W-35333, S6O-004400, S6W-31770, S6O-04018, S6W-29513, S6O-04620, S6W-36240, S6W-37319, S6W-37320, S6W-38025, S6O-04857).
In its answers, the Scottish Government has referred to the £123 million allocated to Health Boards in 2025 to improve the delivery of mental health services for both children and adults, including neurodevelopmental pathways.
The Scottish Government also highlighted continuing efforts to implement the National Neurodevelopmental Specification for children and young people, and the work of the National Autism Implementation Team to 'develop, enhance and redesign' adult neurodevelopmental services.
Cross-Party Groups
The Cross-Party Group in the Scottish Parliament on Autism consists of MSPs from across the political spectrum, organisations that work with autistic people in Scotland, and other individuals. It meets multiple times a year, and is organised in partnership with the National Autistic Society Scotland.
Drivers of increasing demand for neurodevelopmental assessments
There has been a continuous increase in the number of people seeking an assessment for a neurodevelopmental condition over the past decade. This is evident in the data received from NHS boards, which show a dramatic rise in referrals since 2020. More granular data on this rise - for example, a breakdown of referrals by suspected condition, or data on how many patients are refused a referral - is not available.
This increase is also observed in other parts of the UK. In England, annual referrals for autism assessment doubled from 55,000 to 111,000 in the three year period 2019/20 to 2022/23. Although data on the number of referrals is not readily available before this, one study found that the number of autism diagnoses in the UK increased by 787% between 1998 and 2018. This corresponded to an increase of roughly 7% per year. The data also show a significant increase in the number of people seeking or receiving treatment for other neurodevelopmental conditions. Data from NHS England shows a 50% increase in the number of patients being prescribed medicine for ADHD in the period 2019-2023.
While the best estimates of the prevalence of neurodevelopmental conditions have changed through time1, there is no evidence to suggest that the prevalence itself is changing. Instead, it appears there is an increasing awareness of neurodiversity within the public, and as a result more people (who may not have thought of themselves as neurodivergent in the past) - are seeking neurodevelopmental assessments. It has been suggested that this heightened awareness is driven by improved education surrounding mental health and neurodiversity2, particularly with regards to women and girls. The work of third sector organisations, coupled with initiatives such as Neurodiversity Celebration Week, has led to significant progress in the way neurodivergent people are treated within society, and appears to have made people more likely to seek neurodevelopmental assessments.
Another factor contributing to the increased demand for these services is the improved provision for neurodivergent people. Prior to 2020, many health boards did not provide neurodevelopmental pathways at all, meaning neurodivergent people had no way obtain an assessment. Often, these people were known to mental health services but neurodevelopmental assessments were not available to them. The increased provision of neurodevelopmental pathways across Scotland has therefore provided an avenue for these people to express their need, and the statistics reflect this. However, while the provision and availability of neurodevelopmental assessments has increased, it has not kept pace with the surging demand, which has led to the long waiting times for assessments.
Adverse health outcomes facing neurodivergent people
Neurodivergent people are more likely to encounter mental and physical health issues in their lives. Alongside the co-occurrence of other neurodevelopmental conditions, neurodivergent people are likely to encounter further mental health conditions such as anxiety, depression, and insomnia. Much of this is likely to stem from the stigma and discrimination they experience in society. The NAIT Adult Neurodevelopmental Pathways report stated that up to 70% of people with neurodevelopmental conditions seek mental health support at some point in their lives. One study found that over half of autistic adults met the criteria for a psychiatric disorder, with anxiety the most common co-occurring condition1. People with ADHD encounter a similar range of disorders, and while a broad neurodevelopmental assessment may be able to diagnose some of these co-occurring conditions, many will be undiagnosed.
As a result, neurodivergent people are likely to face even greater difficulties. Those with mental health needs are at a further disadvantage in education and the workplace, and are at an increased risk of living in poverty. Such issues are heavily linked, and can reinforce each other, leading to adverse outcomes in all aspects of a neurodivergent person's life. Indeed, autistic people and people with ADHD have been shown to be nine and five times more likely to commit suicide than the general population, respectively23.
In addition to mental health challenges connected to and exacerbated by neurodevelopmental conditions, neurodivergent people are also at increased risk of a number of physical health issues45.
Epilepsy. Approximately 30% of autistic people also have epilepsy, a neurological condition characterized by recurring seizures.
Ehlers-Danlos Syndrome and Joint Hypermobility Syndrome. These are two closely related conditions that can affect connective tissues and the autonomous nervous system. Symptoms include tiredness, persistent and widespread pain, and fragile skin and joints.
Chronic Pain. It has been suggested that this is due to a co-occurring genetic disposition towards pain, increased sensitivity or an increased likelihood of injury due to underdeveloped motor skills - or a combination of these effects4. Females are particularly susceptible to chronic pain7.
Gastro-intestinal problems. These are particularly common, with one study finding at least one gastro-intestinal problem in over 90% of autistic children8. Specific problems include Coeliac's disease, constipation, diarrhoea, and vomiting, although this may also link to other behaviours associated with neurodivergence such as food selectivity.
As with the mental health discussions above, the consequences of these physical health issues are wide-ranging. Neurodivergent people face high rates of misdiagnosis for these conditions, often due to a lack of belief in the severity of the symptoms9. This can lead to more significant consequences in later life. Physical health issues also cause neurodivergent people to miss out on educational and social opportunities, as well as impacting life in the workplace. Most starkly, studies have shown that the life expectancy of autistic people is significantly less than the general population. One study estimated that autistic people (with no learning disability) live six years less than the general population on average10, although another put this figure at 16 years. This is shown in figure 9 below. The increased prevalence of epilepsy drives some of this discrepancy, as does suicide - which is the leading cause of early death in autistic adults with no additional learning disability. A similar picture is seen in the life expectancy of people with ADHD, which is seven and nine years less than the general population for males and females respectively11. In ADHD, it is the increase in prevalence of smoking, substance use and risk-taking behaviours that is believed to drive this difference.
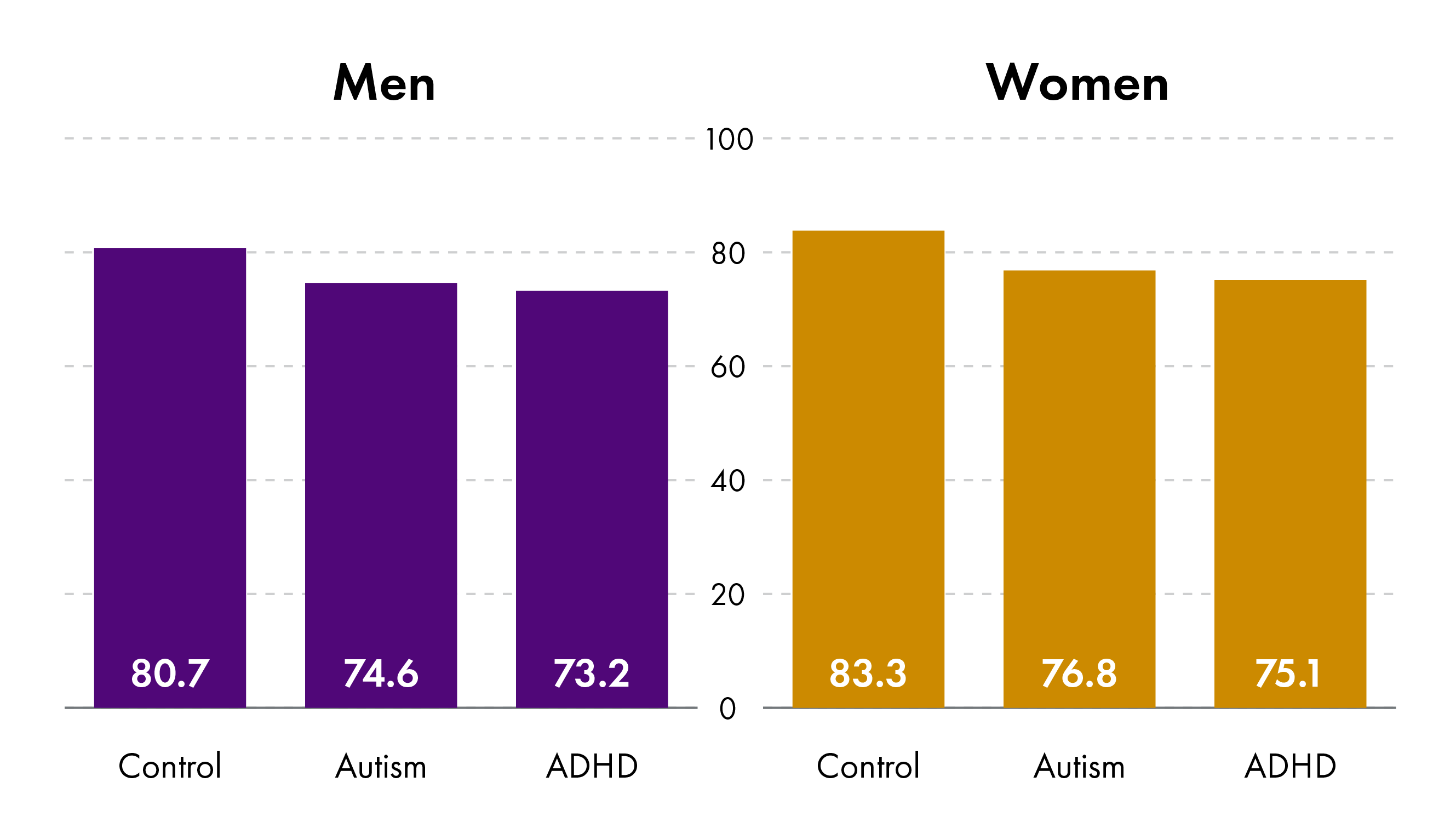
The management and mitigation of such health issues is clearly a key step in ensuring the physical and mental wellbeing of neurodivergent people in Scotland.
Difficulties facing neurodivergent women and girls
Historically, far more men and boys have been diagnosed with autism and other neurodevelopmental conditions than women and girls. One study estimates that over 80% of autism diagnoses over the period 1998-2018 in the UK were of males. While previously it was thought that males are far more likely to develop neurodevelopmental conditions than women, this view has changed. It is now thought that the male-to-female ratio in autism conditions is smaller, and that autism in females tend to be substantially under-diagnosed12. The same is true for other neurodevelopmental conditions; while the National Institute for Health and Care Excellence (NICE) estimates there are roughly three times as many males with ADHD than females, females are far less likely to be diagnosed than males, especially in childhood3.
A few reasons have been suggested as to why autism and other neurodevelopmental conditions in women and girls tends to be under-diagnosed.
Gender bias within diagnostic criteria: The criteria used to diagnose ADHD are based on a field study that included only 21% women, suggesting that ADHD assessments are likely to be more appropriate for males3. It has been suggested that the autism assessment criteria show a similar gender bias5.
Different symptoms of neurodevelopmental conditions in females: Autistic women and girls can appear to have fewer social difficulties than autistic men and boys, have better conversation skills, and a higher likelihood of sharing interests with others. Similarly, NICE suggests that females with ADHD are more likely to have the 'inattentive' subtype as opposed to the 'hyperactive-impulsive' subtype, which makes diagnosis more difficult. As a result, females are commonly misdiagnosed with anxiety, depression and other psychiatric disorders6.
Masking: Studies have shown that females are far more likely to hide or camouflage their symptoms of neurodivergence in social contexts, a behaviour known as 'masking'7. Techniques for masking include forcing eye contact, imitating expressions and gestures and following 'scripts' for social situations. This can make recognising and diagnosing these conditions much harder and may also lead to additional mental health difficulties.
There are a number of consequences of this diagnostic gap. One is that women are often misdiagnosed and receive inadequate or unsuitable support in managing their behaviours. Another is that those women and girls who are diagnosed with a neurodevelopmental condition tend to receive their diagnosis later in life than their male counterparts. One study suggests up to 80% of autistic females are undiagnosed at the age of eighteen6. Autistic women experience worse mental health outcomes and are more likely to commit suicide than autistic men9, who are already at a higher risk of suicide than the neurotypical community.
There is clearly a need to improve the understanding and diagnosis of neurodivergence in women. Third sector organisations such as the Scottish Women's Autistic Network (SWAN) work to provide services, information and support for autistic women, girls and non-binary people at both the pre- and post-diagnostic stages. Outside the third sector, however, many people feel there is a significant lack of policy and pathways for neurodivergent women and girls in Scotland.
Neurodivergence in minority ethnic groups
On top of the many barriers to support faced by the neurodivergent population as a whole, additional challenges present themselves to neurodivergent people from minority ethnic groups. Often, people assessing an ethnic minority patient for autism will interpret communication difficulties as simply being due to cultural differences or the language barrier. Evidence suggests1 that the diagnostic criteria for autism are better at detecting autistic traits in white people than in ethnic minorities. In addition, ethnic minority autistic people are less likely to be able to produce evidence of historic developmental difficulties, or family members who may have had a neurodevelopmental condition2. This is borne out by data from England, where one report found that Asian and black children were diagnosed with ADHD at a significantly lower rate than the general population.
Studies have shown that minority ethnic neurodivergent people face extra discrimination and stereotyping in education3 and in the workplace4. They are also less likely to be diagnosed with autism and ADHD, and more likely to be incorrectly diagnosed with other mental health conditions56. When neurodivergent people from minority ethnic groups are diagnosed with ADHD, they are less likely to be prescribed medication and receive adequate follow-up7.
Within Scotland, the Scottish Ethnic Minority Autistics (SEMA) work to support this group of individuals and foster a better understanding of neurodivergence within the ethnic minority community. However, no policy provision or healthcare guidelines exist for this group specifically.
Stigma and discrimination towards neurodivergent people
There is a societal stigma surrounding neurodivergent people, and this group experiences significant discrimination as a result1. This is mostly driven by people's lack of understanding of autism, and particularly its negative traits. As a result, there is evidence that neurotypical people are less likely to want to socialise with, and be in romantic relationships with, neurodivergent people23. This is a driver of the high rates of loneliness experienced by the neurodivergent population. Stigma of this sort is not limited to the neurodivergent person themself, but can affect those around them including family and carers45.
In the workplace, discrimination against a person because of disability is unlawful under The Equality Act 2010. A survey found that one in five neurodivergent people experience harassment or discrimination at work because of their neurodivergence. The survey found that this may be because 3 in 10 neurodivergent employees don't disclose their neurodivergence to their employer, and nearly half feel as though though their organisation does not provide a supportive climate in which employees are comfortable talking about neurodiversity.
The way that neurodivergent people are viewed within society is damaging to the mental health of such groups6, and meaningful change is required to improve the outcomes for these people. In response to the consultation on the Learning Disabilities, Autism and Neurodivergence Bill, neurodivergent people frequently mentioned the need for greater awareness, understanding and training on neurodivergence. One of the goals of that Bill was for
public sector staff who work directly with members of the public [to] have confidence and skills in being able to understand the needs of neurodivergent people and people with learning disabilities, resulting in improved services and communication and reduced health inequalities.
Scottish Government, Learning Disabilities, Autism and Neurodivergence Bill: Consultation, 2023
The proposal for the Bill suggested mandatory training for public sector services. This would initially include just healthcare services, but could be expanded to education, and justice systems. However, it would require broadening of such training into the private sector to tackle these challenges universally.
ADHD medication and shared care agreements
Medication can treat the symptoms of ADHD. Medicines commonly prescribed include stimulants such as methylphenidate, and sleep treatments like melatonin. Stimulants enable the patient to focus better and improve attention. This often improves the experience of people with ADHD, although medication does not work in every case. More medication is typically prescribed to children, although the rate of prescription to both children and adults has increased in recent years12.
In Scotland, ADHD medication can cost in the range £500-£2000 per year if prescribed privately. As a result, in some areas patients who receive a private diagnosis for ADHD may enter a shared care agreement. Under such an agreement, the GP prescribes the medication and the NHS covers the cost, but the private consultant administers and manages the treatment. There is no NHS Scotland policy surrounding shared care agreements, and it is often up to individual GPs as to whether such an agreement is appropriate. This has resulted in calls for clearer national policy on shared care agreements, and Scottish Government is working with the Royal College of General Practitioners to develop this.
NAIT has already published guidance on this matter, as have some health boards (such as NHS Greater Glasgow and Clyde and NHS Lothian). Previous work has described the factors at play in this decision:
[GPs] may have concerns about issues such as the quality and accuracy of private diagnoses, particularly when a private diagnostic service is only assessing patients for one condition, and may therefore miss other potential conditions that could be causing or exacerbating the patient’s symptoms. They may also wish to confirm with a specialist that the recommended medication would not interact with any other medications the patient is receiving. The medication monitoring processes followed by private diagnostic service providers may also differ from NHS recommendations, potentially creating a difficult professional situation for a GP.
Sarah Swift (SPICe), Attention Deficit Hyperactivity Disorder (ADHD) in Scotland – Prevalence, treatment, and private care, 2024
As shown in table 4 below, it is impossible to ascertain how many shared care agreements are in place across Scotland. Only two of the fourteen health boards (NHS Tayside and NHS Western Isles) reported the number of patients in shared care agreements, and many health boards had no such agreements in place as of March 2025.
| Health Board | Number of GP practices offering shared care for any medication | Number of GP practices offering shared care for medication for a neurodevelopmental condition. |
|---|---|---|
| NHS Grampian | No answer | No answer |
| NHS Tayside | No answer | As of December 2024, 1666 adults were prescribed ADHD medication in NHS Tayside, and all 'should be treated under the Shared Care Agreement'. |
| NHS Highland | All practices involved in ongoing management of medications. | All practices involved in ongoing management of medications. |
| NHS Orkney | None | None |
| NHS Shetland | No answer | No answer |
| NHS Western Isles | All practices | 9 |
| NHS Lothian | Not recorded | |
| NHS Forth Valley | Not recorded | Not recorded |
| NHS Borders | None | None |
| NHS Fife | None for adults, not recorded for children | None for adults, not recorded for children |
| NHS Greater Clyde andGlasgow | None | None |
| NHS Lanarkshire | No answer | No answer |
| NHS Dumfries and Galloway | No answer | No answer |
| NHS Ayrshire and Arran | None | None |
In addition to the difficulty in entering shared care agreements, patients may also encounter delays in obtaining the medication itself. Many health boards operate separate waiting lists for medication, partly due to the ongoing global shortage of ADHD medication.
Transitions to adulthood
Neurodivergent people in Scotland experience transitions in a range of areas, especially as they approach adulthood. Transitions is any change from one stage of life to another, and can include:
in healthcare, transitions between Child and Adolescent Mental Health Services (CAMHS) and Adult Mental Health Services (AMHS) or similar.
in education, transitions between primary and secondary schools, college, and university.
in employment, transitions between different jobs or into/out of employment.
in social security, transition between different support mechanisms such as Child Disability Payment and Adult Disability Payment.
These transitions form a key part of a neurodivergent person's life and can be very challenging to navigate. Current policy includes a Principles of Transition document published by the Scottish Government setting out guidance for young people moving between CAMHS and Adult Mental Health Services. In addition, the GIRFEC policy and guidance touch on the importance of well-planned and supported transitions. Despite this, neurodivergent people still report experiencing difficulties in many aspects of transitions, especially between mental health services and educational institutions. On the other hand the national neurodevelopmental specification addresses transitions as one of its key standards, and this has been well-received by the neurodivergent community.
Data collection
NAIT's Children's Neurodevelopmental Pathway Practice Framework report states that:
Data is essential for quality assurance and quality improvement in a neurodevelopmental pathway and it informs service delivery. With better data, local teams are better placed to understand improvement or change required to local neurodevelopmental pathways. In order to monitor the implementation of evidence based guidelines and pathways, services should establish good quality and efficient processes for data collection, linked to standards for the service and local electronic patient record systems.
National Autism Implementation Team, Children's Neurodevelopmental Pathway Practice Framework, 2024
Despite this, there is a significant lack of data surrounding neurodevelopmental pathways in Scotland. On 28 May 2025, the Minister for Social Care, Mental Wellbeing and Sport stated that:
Figures on the number of people seeking a diagnosis for a neurodevelopmental condition are not currently nationally reported or published. We are working with health boards and local authorities to improve our understanding of how many people are seeking support and how that data can be used to deliver improvements.
The Minister for Social Care, Mental Wellbeing and Sport (Maree Todd), Debate on Motion S6M-17670 (Neurodevelopmental Conditions), 28 May 2025
As evidenced in the data in this report, some health boards do not hold records of the number of people on waiting lists for neurodevelopmental assessment over time. One board (NHS Grampian) does not even have the ability to separate out neurodevelopmental cases from their CAMHS data at present, and so could not provide the current length of their waiting list. Many other boards were not able to separate out autism and ADHD referrals (in the case that the two conditions were assessed separately) or could provide data on one but not the other. Only two Boards hold information on the number of people with ADHD who have been prescribed medication, the status of waiting lists for such medication and the prevalence of shared care agreements to manage this medication.
This has led to calls for better data collection. Some MSPs have called for:
a step change in how the Scottish Government collects its data so that the statistics reflect the experience on the ground
Paul Sweeney MSP, Debate on Motion S6M-17670 (Neurodevelopmental Conditions), 28 May 2025
In addition to waiting times data, more detailed information about the neurodevelopmental pathways would be crucial in understanding demand and capacity. In the vast majority of cases, this is not available. Where such data has been collected, it is only from a small sample of the whole population, and does not capture information about long-term trends in demand and capacity. NAIT set out the following factors as examples of data that health boards could collect routinely to help understand the demand for a neurodevelopmental service.
Number of requests for assessment made and accepted per month (referral rate).
Number of contacts/appointments offered and attended.
Characteristics of the individuals referred and individuals diagnosed (such as age, gender, and risk factors present).
Quality and usefulness of accompanying information received with referrals.
Triage effectiveness and outcomes and which factors lead to referrals being accepted or not.
Wait from referral to first appointment.
Wait from first appointment to last appointment.
Wait from referral accepted to diagnosis shared.
Diagnostic rate (of those assessed, how many receive a diagnosis of a neurodevelopmental condition).
Outcomes from assessments and co-occurrence of different conditions.
They also list the following areas as important understanding capacity to deliver services.
Whole time equivalent staff time and number of staff in the neurodevelopmental service.
The contribution of community teams and universal services across health and education to recognise and assess need and to plan to meet needs.
The inclusion of all services directly involved in neurodevelopmental assessment and diagnosis.
Workforce information (e.g., number of staff allocated from different professional groups, training and skills needs, gaps within the service and how these are compensated for).
Number of appointments offered per week (taking account of annual leave and absence).
Time taken by professionals and families to complete the assessment.
Availability of accommodation and resources to deliver the service.
Public Health Scotland has developed a Neurodevelopmental Disorders Trajectory Tool to determine the staffing and financial costs of carrying out neurodevelopmental assessments, and therefore estimate the current and future capacity. However, this is not publicly accessible.
NHS Education for Scotland also provide an eLearning module on demand and capacity. Some health boards, such as in NHS Fife and NHS Lanarkshire, are using these tools to develop their neurodevelopmental pathways.
Workforce
Historically, specialist teams of clinical psychologists and psychiatrists have carried out neurodevelopmental assessments. However, as health services take a broader approach to neurodevelopmental assessment, it has been accepted that these assessments should be carried out by multi-disciplinary and multi-agency teams. These can include therapists (e.g. Speech and Language Therapists or Occupational Therapists), nurses, clinical and educational psychologists and GPs. Some health boards, such as NHS Fife, have adopted such a model. The National Autism Implementation Team (NAIT) endorses this approach and has published guidance on who can diagnose autism and ADHD. More consideration is needed for ADHD, since medication is commonly prescribed and this requires the input of a clinician with competency in medical evaluation. Additionally, when the patient presents with possible co-occurring conditions, a team with more competencies in medical evaluations may also be required. Nonetheless, NAIT conclude that ADHD (and autism) can be diagnosed by a range of professionals, and that:
Neurodevelopmental assessment is often best carried out within multidisciplinary teams to enable robust person centred clinical assessment and decision making.
National Autism Implementation Team, NAIT Guidance on Who Can Diagnose ADHD, 2023
Professionals involved in neurodevelopmental assessment require the relevant skills, training, and experience to successfully deliver these assessments, as well as access to peer support and review. NHS Education for Scotland (NES) has funded a number of training initiatives, including the Enhanced Psychological Practice programme, an Autism Training Framework, and a range of resources that cover neurodivergence across the lifespan. The NES 'Assessing ADHD' and 'Understanding ADHD in Girls and Women' webinars were attended by 321 and 922 staff respectively in 2024. NAIT provide further resources for professional training and development on their website.
Leadership
Different bodies are responsible for the delivery of neurodevelopmental services in different areas. Some neurodevelopmental pathways are operated by health boards, while others are delivered by Health and Social Care Partnerships. Within some health boards (such as NHS Grampian and NHS Greater Glasgow and Clyde) the availability or mode of delivery of assessment services can be dependent on which HSCP the patient resides in. This division of responsibility and lack of national pathway has resulted in different services being available in different areas, which some have called a 'postcode lottery'. This is also seen in the many tests-of-change and pilot projects that the Scottish Government have funded to support the implementation of neurodevelopmental pathways. This funding is allocated to specific health boards and HSCPs, leading to further variation in which services are available in which areas.
There have been calls for strong national leadership, and the development of national neurodevelopmental pathways for children and adults to replace the current regional approach. In a debate in Parliament on neurodevelopmental conditions, there were calls for 'the creation of a national stepped pathway for autism and ADHD diagnosis'. The Royal College of Psychiatrists in Scotland also listed national leadership as a key priority in their proposal for a new approach to neurodevelopmental pathways. The National Autism Implementation Team highlights the need for buy-in from local leadership in developing a successful neurodevelopmental pathway, but also states in its Adult Neurodevelopmental Pathways report that:
National and local leadership is required to build on the work of 2022 in the years ahead.
National Autism Implementation Team, Adult Neurodevelopmental Pathways Report, 2023
Next steps
In a debate on neurodevelopmental conditions in Parliament on 28 May 2025, a motion was agreed to that:
calls on the Scottish Government to convene a crossparty summit on addressing waits for neurodevelopmental support and mental health capacity to avert a crisis for individuals and families waiting too long.
Motion S6M-17670, Addressing the Inadequate Provision for Neurodevelopmental Conditions, 28 May 2025
In addition, on 17 June 2025 the Health, Social Care and Sport Committee agreed that its next major inquiry would be into ADHD and autism pathways and support. The Committee agreed to write to the Scottish Government to request a policy update related to its planned inquiry. The Equalties, Human Rights and Civil Justice Committee also agreed at its meeting on 13 May 2025 to undertake an inquiry into neurodivergence in Scotland.
Finally, on 26 June 2025 the Minister for Social Care, Mental Wellbeing and Sport will make a statement on 'Ensuring the Right Support for Young People's Neurodivergence, Mental Health and Wellbeing'. This will accompany the release of the review of the implementation of the National Neurodevelopmental Specification.
Annex A: Detailed information on neurodevelopmental pathways available in each NHS board
The following section outlines the provision of neurodevelopmental pathways for adults and children in each of the fourteen NHS Scotland territorial health boards, combining information online with the responses to the Health, Social Care and Sport Committee's letter of March 2025. The information in this section represents information available at the time of writing, but it should be noted that many of these pathways are under development and provision of services may change.
NHS Grampian
Neurodevelopmental assessments for children in NHS Grampian are carried out either by CAMHS (when patients meet the referral criteria), or by Paediatric Community Child Health (CCH) services. Children are generally referred to CCH services through schools. Neither service offers specific support to children while they wait for an assessment, although national third sector support is available.
Between 2022 and 2024, Aberdeen City HSCP received Scottish Government funding to host a test-of-change program whereby a multidisciplinary neurodevelopmental assessment team was embedded within a primary school to provide direct assessment and intervention support to children, their families and the school. This was highly successful and led to "potentially significant benefits to the young person, the family, the school and the multidisciplinary [assessment] team". The funding was non-recurring, however, and the program did not continue.
Neurodivergent adults in NHS Grampian who meet the criteria for referral to secondary mental health services are assessed through the Community Mental Health Teams. Until March 2025, neurodivergent adults who did not meet these criteria were assessed by the Grampian-wide Adult Autism Assessment Team (AAAT). This was jointly funded by the three HSCPs in NHS Grampian (Moray, Aberdeenshire and Aberdeen City), and provided assessments for autism only, with plans in place to move to an overarching neurodevelopmental assessment. However, in February 2025, Aberdeenshire HSCP announced that due to the end of its non-recurring funding for the service from the Scottish Government, it would no longer be a part of this program. The AAAT continues to operate in Moray and Aberdeen City. GPs and CMHTs can refer patients to the AAAT, but the team also take self-referrals. Those waiting for assessment are signposted to a range of third sector support and can attend pre-assessment drop-in information sessions. For patients seeking an ADHD assessment, Aberdeen City HSCP currently has a small multidisciplinary ADHD assessment service that has been running since 2024. Aberdeenshire HSCP also had an ADHD pathway, but this also ceased due to lack of funding in March 2025.
NHS Tayside
Historically, all children seeking a neurodevelopmental assessment in NHS Tayside were referred to CAMHS, which had two pathways of care. The first of these was to assess children and young people presenting with mental health conditions (i.e. meeting CAMHS referral criteria), and the second was to carry out neurodevelopmental assessments for children who did not meet the CAMHS referral criteria. Some of these assessments were carried out by Healios, a private, online neurodevelopmental assesssment service commissioned by NHS Tayside. However, in March 2025, NHS Tayside announced that it was not taking any new referrals for the second of these pathways, so that only children with were co-existing mental health conditions would be able to obtain a neurodevelopmental assessment. This would free up resources for the highest-risk cases, and children with no co-occurring mental health condition would be directed towards online support (such as the NHS Tayside Neurodevelopmental Portal) and in-person, peer-to-peer support sessions. NHS Tayside is currently working with the local authority partners to develop a new pathway that aligns with the National Neurodevelpomental Specification.
The Dundee HSCP oversees the provision of services of neurodivergent adults in Tayside, and there is no overarching neurodevelopmental pathway for adults in this region. Instead, adults are seen by different teams, depending on whether they require an assessment for ADHD or autism. ADHD referrals are made to Community Mental Health Teams (CMHTs), although for such a referral to be made, the patient must meet the criteria for referral to secondary mental health services. The CMHTs can also carry out autism assessments, but the majority of autism assessments are carried out by the Tayside Adult Autism Consultancy Team (TAACT). Patients on the TAACT waiting list have access to local community support such as Dundee Connections.
NHS Highland
For children and young people, NHS Highland (through the Highland HSCP) operates a Neurodevelopmental Assessment Service (NDAS). This service is based at The Pines in Inverness, and provides an overarching neurodevelopmental assessment service. NDAS operates an open referral system, although it does a preliminary screening of referrals before the child is added to the waiting list. While waiting for an assessment, children have access to diagnosis-independent support from The Pines and other third sector organisations such as Thriving Families.
Neurodivergent adults in NHS Highland have access to separate autism and ADHD pathways. The pilot adult ADHD pathway was developed as part of NAIT's Adult Neurodevelopmental Pathways pathfinder study in 2022, and there was no provision for adult ADHD before this. As of October 2023, the pathway was not taking any new referrals due to the backlog of existing referrals, and any new patients seeking an ADHD assessment had to meet the criteria for referral to secondary mental health services in order to obtain an assessment. Further plans were underway to develop the pathway further in 2024. The adult autism pathway is independent of the CMHTs and therefore does not require a co-occurring mental health condition to access, but no information is available about this pathway online. A revised pathway is under development. Adults waiting for assessment have access to a range of third sector support, including from the Highland One Stop Shop. Autism Rights Group Highland also works to promote better services for autistic people in the Highland region and beyond.
NHS Orkney
NHS Orkney provides neurodevelopmental assessments for children, both within CAMHS (for those who meet the criteria for referral) and through a separate service. However, no details of this service are available online. Support for people waiting for a diagnosis is available through the GIRFEC framework and national/online resources, but no specific support for neurodivergent children is available in Orkney.
Historically, NHS Orkney had an agreement with NHS Grampian to allow their patients access to adult neurodevelopmental services on the mainland. While a neurodevelopmental pathway for adults is under development in Orkney at present, adult neurodevelopmental assessments are currently outsourced to an external specialist service (Connect to Autism). There is no formal support pathway for adults waiting for these assessments.
NHS Shetland
In Shetland, children can be assessed for neurodevelopmental conditions through CAMHS (autism only), Community Paediatrics, and Speech and Language Therapy (SLT) services, although there exists limited information about these three pathways. The SLT pathway accepts referrals for those without a co-existing mental health condition. The SLT service also provides support for those waiting for a diagnosis.
Historically, NHS Shetland had an agreement with NHS Grampian to allow their patients access to adult neurodevelopmental services on the mainland. At present, there is an Adult Autism Assessment Pathway in Shetland, to which GPs and other Mental Health Professionals can refer patients. The SLT service manage this pathway, although due to the temporary nature of the funding, assessments are currently on hold. Community Mental Health Teams can also carry out assessments, where patients meet the criteria for referral to secondary mental health services.
NHS Western Isles
NHS Western Isles established an overarching neurodevelopmental service for children in August 2024. This replaced condition-specific pathways. No additional support is available for children waiting for a neurodevelopmental assessment outside the GIRFEC framework, although they may access third sector support from charities such as Autism Eileanan Siar in Stornoway.
Historically, NHS Western Isles had an agreement with NHS Highland to allow their patients access to adult neurodevelopmental services on the mainland. At present, it operates an adult neurodevelopmental assessment service, although currently ADHD assessment has not been incorporated into this service.
NHS Lothian
The child neurodevelopmental pathways in NHS Lothian are broadly hosted within CAMHS (for those that meet the referral criteria) and Community Paediatrics. Access to these pathways varies between the HSCPs. For example, East Lothian HSCP operates a pathway with a Single Point of Access scheme. Schools are encouraged to make these referrals, although GPs and health visitors can make referrals as well. Patients are also directed to a range of further support while waiting for assessment, both by CAMHS and by their local HSCP. Work is currently underway to implement a Lothian-wide pathway, which will be located in the women and children's directorate rather than CAMHS.
For adults, there is an overarching neurodevelopmental pathway within the Community Mental Health Team, although the four HSCPs have different modes of delivery. Patients are referred to this by their GPs, who use a diagnostic questionnaire as an initial screening test before passing the referral on to the CMHT. The CMHTs provide neurodevelopmental assessments even if the patient does not meet the criteria for referral to secondary mental health services. As with the pathway for children, a large selection of additional support is signposted on the website, including post-diagnostic support.
NHS Forth Valley
NHS Forth Valley offers an overarching neurodevelopmental assessment service for children and young people, either through CAMHS (when the child meets the referral criteria), or through the Paediatric Neurodevelopmental Service (PNDS). While waiting for assessment, children and young people are signposted to a range of community support.
The Adult Autism Assessment Team (AAAT), which delivered neurodevelopmental assessments to adults who do not meet the criteria for referral to secondary mental health services in NHS Forth Valley, was halted in March 2025. The team consisted of just one nurse and one part-time (10%) psychiatrist, and both left their posts in late 2024. Rather than re-appointing those roles, NHS Forth Valley has paused the assessment service and is currently exploring ways to re-allocate this funding in a more efficient way. As a result, neurodevelopmental assessments are only currently available to to adults if they meet the criteria for secondary care mental health services, through CMHTs. Adults who were waiting for assessment by the AAAT have been signposted to a range of third sector support.
NHS Borders
For children and young people in NHS Borders, neurodevelopmental assessments are carried out within the Child and Adolescent Mental Health Service (CAMHS), regardless of whether the patient meets the referral criteria. While it is stated on the NHS Borders website that autism assessments are carried out by the multi-agency Borders Autism Team within CAMHS, it appears that as of 2023 there was an overarching neurodevelopmental assessment pathway that assessed for multiple neurodevelopmental conditions including autism, ADHD and learning disabilities.
While waiting for a neurodevelopmental assessment, young people are signposted to a range of local and national third sector services. As of 2024, the Scottish Borders HSCP were considering a proposal to review neurodevelopmental pathways for children, and particularly the integration of health, social care and educational services.
Adults with co-existing mental health conditions can be referred by their GP for a neurodevelopmental assessment, which is carried out by Community Mental Health Teams. However, this service is only accessible to adults who meet the criteria for referral to secondary mental health services. Adults who do not meet this criteria are given a self-help resource pack and discharged without referral.
NHS Fife
In Fife, neurodivergent children who meet the criteria are referred to CAMHS, while other cases are referred to the NHS Fife Neurodevelopmental Pathway (NDP). This launched in August 2024, and operates within NAIT's guidelines on stepped care, with support available at a number of tiers. These tiers range from Tier 1 (peer-to-peer and third sector support) through to neurodevelopmentally informed support at Tier 4. Higher level support is generally only accessible for those who have first accessed third sector support. Triage to determine the level of support required is aided by the Fife Neurodevelopmental Questionnaire (F-NDQ), a developmental history survey filled out by parents. In addition, Fife has commissioned neurodevelopmental assessments from an online provider, Healios, to support the work of the NDP team. Patients are well-signposted to support while waiting for diagnosis, including the Neurodevelopmental Hub and the Fife One Stop Shop (funded by the Fife HSCP). They may also self-refer to Access Therapies Fife, which provides online and in-person mental health support. NHS Fife's neurodevelopmental pathway has been cited as an example of good practice, due to its stepped care and multi-disciplinary approach.
NHS Fife does not have a specific adult neurodevelopmental pathway. The Community Mental Health Team triage referrals on an individual basis, although assessments are only available for those that meet the criteria for referral to secondary mental health services. These are carried out by the CMHT Adult Psychiatry and Adult Psychology groups for ADHD and autism respectively. Adults waiting for assessment have access to the Neurodevelopmental Hub, the Fife One Stop Shop and Access Therapies Fife.
NHS Greater Glasgow and Clyde
NHS Greater Glasgow and Clyde operates an overarching neurodevelopmental pathway, which takes referrals for assessment from children who do not meet the criteria for referral to CAMHS. The pathway was set up in 2023-2024, bringing together previous services from CAMHS and and Community Paediatrics. Patients waiting for assessment have access to a broad range of further support, including access to a neurodevelopmental hub in some HSCPs.
The Adult Autism Team (AAT) operates within the Community Mental Health Teams, and provides autism assessments for adults who do not meet the criteria for referral to secondary mental health services. ADHD assessments are carried out within the HSCPs, rather than through a centralised service, and a different screening process and waiting list is operated in each of the six HSCPs in the Greater Glasgow and Clyde region.
NHS Lanarkshire
The neurodevelopmental pathway for children in NHS Lanarkshire is well-established, with over 50 clinical and administrative full-time staff as of 2024. . Neurodivergent people seeking an assessment are referred to either CAMHS (if they meet the referral criteria), or to the overarching Neurodevelopmental Service for Children and Young People (NDS). This is a specialist neurodevelopmental assessment service that has existed for many years within NHS Lanarkshire. A referral to the NDS can be made by a school, health visitors, allied health professionals, or GPs, and is available for children aged 3-18. Such a referral must meet the criterion that condition leads to an impact on the function of the child, and significantly and persistently affects day-to-day life. Children less than three years old are referred to the community paediatrics team in the first instance, who may then further refer to the NDS.
A range of resources is available for children and their families on neurodevelopmental assessment waiting lists in NHS Lanarkshire. This includes parent workshops that cover common challenges faced by neurodivergent young people, and support from a number of third sector organisations in Lanarkshire and nationally.
Adults in NHS Lanarkshire have access to the Adult Neurodevelopmental Service (ANDS), established in April 2024. Adults seeking a neurodevelopmental assessment can be referred to this service by their GP, but also by Community Mental Health Teams and Pyschological Therapy Teams. Despite its name, this service focuses mostly on autism assessment, and patients must have 'evidence of lifelong autistic characteristics affecting daily functioning' in order to access the service. Adults with learning disabilities who co-present with autism follow a different pathway. It is unclear whether a patient who does not meet the criteria for referral to secondary mental health services can be referred for an ADHD diagnosis in NHS Lanarkshire.
NHS Dumfries and Galloway
NHS Dumfries and Galloway operate a Neurodevelopmental Assessment Service for Children and Young People (NDAS), specifically aligned to the National Neurodevelopmental Service Specification. This service operates an open referral system, and so referrals can come from young people and their families, as well as from schools and GPs. Patients who are concerned about ADHD only are advised to contact CAMHS, rather than the NDAS team. Children waiting for a diagnosis through this service have access to support from health visitors, speech and language therapists, occupational therapists, although no specific support for neurodivergence is available.
NHS Dumfries and Galloway does not provide neurodevelopmental assessments for adults unless they meet the criteria for referral to secondary mental health services.
NHS Ayrshire and Arran
For children in Ayrshire and Arran, neurodevelopmental assessments are available to those meeting CAMHS or community paediatrics referral criteria only. Patients not meeting these criteria are unable to access neurodevelopmental assessments. In 2022, NHS Ayrshire and Arran announced that they were commissioning the Purple House Clinic to deliver some of their neurodevelopmental assessments for children.
NHS Ayrshire and Arran have no functioning operational pathway for adult neurodevelopmental assessments, and no longer accept referrals.
Both adults and children who are seeking a diagnosis are signposted to the Neurodevelopmental Empowerment and Strategy Team (NEST). This is an Ayrshire-wide service providing advice and support for neurodivergent people and their families, regardless of whether they have a diagnosis.