Health and Sport Committee
More than 50% of the Scottish Budget - What are the expected outcomes from the Health and Social Care 2021/22 Budget?
Introduction
The Health and Sport Committee of the Scottish Parliament scrutinises the spending of a significant proportion of the Scottish budget. With the additional Covid-related spending in 2020-21, health and social care spending accounts for more than 50% of the Scottish resource budget. We have agreed to undertake pre-budget scrutiny of the 2021-22 budget while also considering the impact of Covid-19 on the Health and Social Care 20/21 settlement.
At the start of the Parliamentary Session, the Committee agreed to adopt a full year budgeting approach, building an element of budget scrutiny into all aspects of our work, as detailed in its 2nd report, 2016 (Session 5) Health and Social Care Integration Budgets.
Throughout this session the primary focus of our budget scrutiny has been on Integration Authorities (IAs). The Public Bodies (Joint Working) (Scotland) Act 2014 required local authorities and NHS boards to form partnerships called integration authorities by 1 April 2016. The aim being:
To improve the quality and consistency of services for patients, carers, service users and their families; to provide seamless, joined up quality health and social care services in order to care for people in their homes or a homely setting where it is safe to do so; and to ensure resources are used effectively and efficiently to deliver services that meet the increasing number of people with longer term and often complex needs, many of whom are older.i
IA budgets totalled £9.3 billion in 2019-20, of which £6.5 billion was delegated from the NHS budget. IAs therefore direct over half of the total health and sport budget. We agreed a continued focus on IA budgets in the pre-budget scrutiny for 2020-21, particularly in light of the ongoing concerns raised by us in respect of the progress of integration.
This report also looks back at areas covered by our previous budget reports to identify progress and improvements that have been made.
The arrival in Scotland of the Covid-19 pandemic and in particular the nationwide lockdown which took effect on 23 March has had a significant impact on NHS and social care services with extraordinary budgetary implications. More specifically, on the 17 March, NHS Scotland was placed in emergency measures and Boards were asked to suspend all non-urgent elective treatment.
We have taken a close interest in the impact of both addressing the health implications of Covid-19 and the wider societal impacts on the delivery of health and social care services. The additional costs faced by health and social care impact heavily on budget and financial considerations and introduce a large degree of uncertainty in relation to budgeting both for current and future years.
Accordingly this budget report also looks at the impacts to health budgets as a result of the pandemic and the additional costs which have been identified to date. We also consider the wider health impacts, the unintended consequences, caused by the actions taken to address the virus by health and social care and reflect the monetary and time impacts of these in our report.
The timing and purpose of this report, in advance of the publication of the Scottish Government’s draft budget, is to provide the Scottish Government with time to consider the implementation of our recommendations in its forthcoming budget 2021-22.
Approach to scrutiny
To inform our work, we held an evidence session with the Director-General of Health and Social Care from the Scottish Government and her officials. We also issued a questionnaire to all Health Boards and IA’s to ascertain the impact of Covid-19 on their delivery and financial performance in the first quarter of 2020-21.
Given the significant impact on the delivery of social care we took evidence from the Care Inspectorate. We wished to understand their statutory role, their responsibilities powers and duties, and obtain an independent viewpoint on the impact and implications arising from Covid-19. We were also interested in their views on the support to and performance of the wider care sector during the first months of the pandemic.
We heard from Ayrshire and Arran Health Board on the direct and indirect impact on the delivery of health services. And later from the two largest territorial Boards, Greater Glasgow and Clyde and NHS Lothian on similar subjects including specifically cost impacts and plans for remobilisation of services.
We then heard from chief officers of integration joint boards on their role, the challenges they face and how the experience of the pandemic had affected them and changed the way they were able to operate more widely.
All oral evidence sessions were followed up by further written questions to clarify and develop areas that arose. We received significant amounts of follow up material and are grateful to all for their co-operation during what we recognise are challenging times across the whole of health and social care.
Finally, and unusually in our budget scrutiny process, we heard from the Minister for Public Health, Sport and Wellbeing and then the Cabinet Secretary for Health and Sport. Given the significant impacts on services and budgets we wanted to understand the role of Government during the pandemic and how the financial impacts was being and was going to be addressed.
We thank all of our witnesses, both those who appeared “in person” and those who provided written submissions.
We intend to hold a further evidence session with the Cabinet Secretary for Health and Sport following the publication of the Scottish budget.
Our report looks at the budget generally then considers the impact of Covid-19 on budgets before considering the progress made with the integration agenda. We also consider the extent to which areas covered in our budget reports throughout this session have been addressed.
Budget setting process
Integration authorities (IAs) direct a proportion of health board and local authority funding. Their budgets consist of two elements, which vary in size and scope depending on the functions delegated to them:
Health care (including primary and community health, as well as some hospital services); and
Social care.
To set IA budgets, the IAs, the NHS and local authority partners work together to determine how much is required to deliver the delegated services and how much each partner will contribute to these identified costs. This budget is then directed to the control of the IA.
An issue we have pursued vigorously over recent years is access to comprehensive and timely information on IA budgets. In response to our earlier recommendations, the Scottish Government is now providing quarterly financial updates. While this is welcome, there remains a significant time lag in reporting. In previous years, this has meant that when we are beginning our pre-budget scrutiny, no information is available on the budgets agreed for the current financial year. Through the normal IA reporting timescales, this information would not become available until September – six months into the financial year to which the budget relates. Therefore, whilst some progress has been made and welcomed, there remains a considerable delay in accessing information on budgets agreed at the start of the financial year.
This year, it was helpful to receive notification of agreed budgets from the Cabinet Secretary at the beginning of June, which helped inform our pre-budget scrutiny and we would welcome a commitment to provision of similar information in future years as early as is possible.
While we recognise each IA has its own governance arrangements for the reporting of financial information, given the size of their combined budgets, £9.3 billion for 2019/20, we do not consider it is appropriate for Parliament to be scrutinising the delivery of services and performance of public bodies without basic financial information.
We have previously been informed the reason for delays in IAs agreeing budgets was due to the difference in financial planning timeframes in local authorities and health boards which impacted on the agreement of budgets in advance of the start of the financial year. In response to this the MSG report recommended budgets be agreed by the end of March 2019 and, the Cabinet Secretary subsequently indicated she expected this timetable to be met.
While we understand that budgets are now being agreed more timeously we have no information as to their quantum and this information is very difficult to collate in a consistent and comparable way from published papers, such as Board papers. We also note at least one authority, Shetland, indicated their budget agreement was delayed because the local NHS budget setting was significantly delayed.
We recognise the need for governance arrangements on spend but cannot accept the reasons behind delays in publishing agreed income levels for such considerable periods.
We again request that arrangements be put in place to publish IA budgets by the end of April each year.
Link between budgets and outcomes
Integrated Authorities have a statutory duty to report against nine national health and wellbeing outcomes. In our budget report of 2016, we first raised concerns over the IAs’ awareness of these reporting requirements and the apparent lack of progress towards publishing budget information of this nature. Our 2018 report highlighted continued challenges with IAs adopting this approach. We concluded:
The Scottish Government must, in advance of the publication of the budget, provide reassurance that developing budget information against outcomes is a top priority, advise when this information will be available and provide further information on the work that is being undertaken with the deadlines set for delivery.
And in our 2019 report we said we expect this statutory duty to be met by all IAs and welcome an update from the Scottish Government as to when this will happen and how details of it will be reported. We also sought details of the support being provided by the Scottish Government in this area.
In its Response the Scottish Government stated it has established a framework for linking budgets and outcomes. Noting that IAs must publish:
Annual audited accounts;
Their budgets for the year, as part of an Annual Financial Statement;
Financial performance reports during the course of the year; and
An Annual Finance Report, as part of the Annual Performance Report which is published within three months of the end of the financial year.
Adding:
The legislation requires sufficient information on the budget and financial performance of each Integration Authority to be in the public domain. It should be noted that the processes for planning and reporting under integration – strategic commissioning plans that span three years, annual financial plans, and annual performance reports and financial statements – all provide important mechanisms to set out local expectations and experience of the relationship between spending, outputs and outcomes.
Notwithstanding the above we continue to struggle to identify any coherent link between spend and outcome. Given the billions of pounds under the control of the Integration Authorities and the statutory duty to report outcomes we expect the Scottish Government to provide the Scottish Parliament with a clear linkage to show in every Authority the relationship between spending, outputs and outcomes.
Put simply, we want to understand the benefits, outcomes and improvements £9 billion of taxpayers money has delivered to the health of the people of Scotland. We also want to be able to compare performance across Boards. We look forward to receiving that information for 2019/2020 and would seek a commitment for regular publication of such information on an annual basis.
Covid-19 Funding and Barnett consequentials
We have taken a close interest in the impact of addressing both the health implications of Covid-19 and the direct impact on wider health and social care services. Equally the additional costs faced by health and social care impact heavily on budget and financial considerations. They also introduce a large degree of uncertainty in relation to budgeting both for the current and future years.
This part of our report summarises some of the financial information we have obtained along with relevant data. The next section looks at the wider health impacts that might arise as a consequence of the cessation of services.
The Scottish Government’s 2020-21 summer budget revision allocated £620 million of health consequentials and the 2020-21 Autumn budget revision allocated a further £1.84 billion making an overall total of £2.5 billion additional health consequentials specifically to meet Covid-19 related costs.
The summer revision provided a detailed breakdown of allocation across areas of spend, but no equivalent breakdown was supplied with the autumn revision, making it impossible for the Committee to scrutinise the additional spend in any meaningful way.
At our meeting on 29 September the Cabinet Secretary confirmed a total of £2.5 billion of health Barnett consequentials had been received by the Scottish Government with some £1.1 billion allocated, with a promise of a further look at costs in January. Indicating that “Every penny of the Barnett consequentials will be used for health and social care”iAlthough we assume the promise relates only to the £2.5 billion health consequentials and we note funding has been held back by the Cabinet Secretary for potential further allocation in January.
The funding will be allocated to NHS Boards and Health and Social Care Partnerships across Scotland to help them meet Covid-19 related costs such as additional staffing or sickness expenditure, enhanced infection prevention and control measures, and the purchase of PPE.ii We note the allocation of this additional funding was based on a modified version of the NHS Scotland resource allocation formula (NRAC), in order to address disproportionate impacts on some areas and takes account of spending incurred and to be incurred. In some cases Boards have received additional sums over and above what would have been calculated using NRAC.
We would welcome further clarification on the methodology used for allocating funds and on any implications for longer term funding plans.
The Scottish Government provided funding to IAs to support resilience in social care provision and ensure any increasing need for care as a result of the pandemic is met. The funding was designed to “help address immediate challenges faced in the social care sector and support ongoing provision of social care” and was distributed across all partnerships.iii Two tranches of £50 million were provided. In total, to 28 September, the Scottish Government advised £245 million additional funding had been provided to HSCPs to support additional Covid-19 pressures in 2020-21 and ensure that frontline care services continue to receive the support required throughout the pandemic.iv [see also later in this part re third sector funding].
Additional Expenditure
Our initial questionnaire to all Health Boards and IAs sought detail of additional funds for Covid-19 and how they had been used. Although most recognised the need for additional expenditure our timing was such that for many it was too early to specify the detail beyond general headings.
The general information we received covered additional staff for ICU while some noted the use of deployed staff from elsewhere;
Costs were incurred from ICU equipment as additional beds were created;
The costs of test and trace including laboratories;
PPE was mentioned by a few although we understand that is a central cost for Boards, although not IAs;
Infection control measures more generally;
IT costs for equipment and software allowing staff to work from home as well as the roll out of Near Me and other digital services to engage patients; and
Overtime and other staff payments were also mentioned.
Some also referred to additional prescribing costs by GPs with a number indicating this was to allow patients to stockpile some medicines, some anticipated that cost being “recouped” with lower subsequent prescribing costs. Other GP costs referred to payments allowing them to open on holiday weekends.
Greater Glasgow and Clyde advised us the additional costs it was facing amounted to just over £60 million for the first quarter of the financial yeari, and on 29 September the Cabinet Secretary provided detailed figures totalling £844 million with a further £245 million to IAs. NHS Greater Glasgow and Clyde was allocated £102 million and the IAs within the NHS Greater Glasgow and Clyde region received £67 million.
We also learned about significant amounts of sustainability payments to support hospices and care homes given lower numbers of residents as a consequence of the pandemic.
Savings
We asked about any savings that had occurred including through the cessation of services. In general, Boards suggested these were marginal as most costs were fixed, covering premises or staff. There were no reported savings in staff costs as a result of reduced or ceased services although some staff were relocated to different roles assisting with Covid-19 related illnesses. We also heard about staff being relocated to support social care services, including an example from one integration authority where librarians were redeployed to undertake clerical duties.
In the survey of IAs and health boards that formed part of the Committee’s pre-budget evidence, IAs and health boards were asked about the main areas of reduced spending during the pandemic. Of those responding to this question, more than half mentioned travel costs having reduced – including both staff travel and patient travel.
The Scottish Government told us there were no formal estimates of any savings madei although later indicating there may be some offsetting savings principally in relation to variable costs associated with the delivery of services not delivered.i The whole area of savings was being looked at as part of the review of health boards expenditure.
We earlier pursued these areas of savings with Ayrshire and Arran Health Board who advised 633 staff were redeployed including secretaries, nurses, AHPs and dental staff. They also provided some more detail on savings including £5 million underspend on supplies and staff redeployment. NHS Lothian advised offset savings amounting to £15 million.
Given the large number of services which ceased operating during lockdown we are surprised at the lack of information available on “savings” or, at the very least, deferred expenditure. We ask the Scottish Government for information on the total amount of savings or delayed expenditure reported to them in their negotiations on additional funding, including the nature of these savings e.g. supplies, travel costs etc.
We also seek detail of how much has been paid to hospices and care homes as sustainability payments across the country and for how long it is envisaged such payments will be made and at what levels?
In relation to staff whose areas were not operating and who were not redeployed, we ask for detail covering the duties undertaking by these staff during lockdown.
Passing on payments to third sector
The Scottish Government has allocated a total of £100million to HSCPs for the Local Mobilisation Funding to support the sustainability of social care providers, who are providing essential frontline support services. This is to enable them to deal with the additional costs they are facing (additional staffing costs, PPE, payment on plan/full commissioned hours) even where that support service has been cancelled'.
However, we were advised of difficulties and delays in funding getting through to providers. The CCPS indicated their members had been having and continued to have difficulties in accessing funding for additional costs for Covid-19 with large amounts of evidence being required before payment. They were facing ongoing delays and non-payment of sustainability payments for care providers and delays in receiving funding from partnerships and local authorities to address emergency action during lockdown and beyond.
We were told some, but perhaps not much, Covid-19 funding has been passed on and where it has there is often vouching and audit requirements which are excessive and impacting on a focus on delivery of support. We were told claims were processed slowly, and monies were not being distributed promptly.
We asked the IAs for comment on the slow payment problems expressed by CCPS and they acknowledged there are challenges which have caused delay in the release of funds.
Capacity issues, both for providers and the HSCPs, has meant providers had struggled to submit claims or quickly respond to requests for the evidence required. HSCPs have had to also respond to the pandemic while taking on this additional workflow all of which have caused delays.
The Chief Officers in a full response on this issue stated:
The governance procedures have been streamlined as much as possible and the IJB Chief Finance Officer Network continue to work closely with Scottish Government colleagues, COSLA and provider representatives to ensure any issues are identified and resolved as quickly as possible. However successful release of funds relies on a number of successful steps and governance procedures while streamlined do require sufficient evidence in order to release funds. Where claims are submitted with sufficient evidence and a signed declaration from the provider these payments are released in a timely manner.i
They also added they continue to work together to resolve issues and are committed to ensuring payments are released as quickly as possible.
The Scottish Government told us they had agreed with the integration authorities to provide 50 per cent of their assumed future costs for social care, with a view to reviewing that in November.ii
We are disappointed to learn about delays in payments being passed on. We recognise the need to evidence these claims but have noted the simpler requirements placed by Scottish Government on accessing additional funds by Partnerships (and Local Authorities). We therefore ask the Scottish Government to ensure requirements imposed by IAs are proportionate and appropriate recognising the essential and emergency nature of the services being provided.
Covid-19
Wider Health Impacts of Covid-19
Any discussion of the impact of Covid-19 must also include the wider impacts on individuals’ health, and their use of healthcare services, in addition to the direct impact of Covid-19 infection.
Reasons for this may include:
Individuals being reluctant to use health services to avoid burdening the NHS or due to an anxiety about the risk of infection;
The health service delaying preventative and non-urgent care such as some screening services and planned surgery;
Other indirect effects of interventions to control Covid-19, such as mental or physical consequences of social distancing measures.
Impact on hospital services
At the start of the pandemic NHS boards were asked to halt all non-urgent procedures as the health service moved to an emergency footing.
Public Health Scotland analysed of data describing changes in health service use in Scotland during the Covid-19 pandemic. This showed hospital admissions, attendances at A&E departments, and cases in out of hours services all fell to around half the average levels seen 2018-19 and have since recovered only modestly. There was a smaller fall in attended ambulance incidents and no appreciable change in NHS 24 111 completed contacts.
Figures suggest just under 60,000 planned operations took place in Scottish hospitals from March to August of this year, compared to 168,000 over the same period in 2019. Although the August figures show an improvement on March to July with the drop being from 28056 in August 2019 to 13831 in August 2020 as services gradually resumed.
Public Health Scotland statistics show wide variations between health boards. In NHS Borders there were 80% fewer operations in August 2020, compared to 32% fewer in Fife. NHS Orkney was operating at 91% of its August 2019 level.
Mental Health Unscheduled care
There were significant falls in the use of unscheduled care for mental health problems compared to the pattern seen in previous years, with a sharp fall of 30-40% in out of hours contacts for mental health problems, starting in early March 2020.
A&E attendances for mental health problems fell by 40-50% from early March 2020 and by the beginning of September had still not fully recovered, remaining at around 10% below previous levels.
New outpatients National Waiting Standard
This requires 95% of new outpatients to have waited no longer than 12 weeks from referral to being seen. In the quarter ending 30 June 2020 there were 61.7% fewer patients seen than in the previous quarter and 65.9% fewer than the same quarter in 2019.
Cardiovascular A&E attendances
Overall there was a sharp drop in cardiovascular attendances at Accident and Emergency Departments. Attendances were around 60% lower compared to the 2018-2019 average. Levels rose again by the end of May, but remain around 30% below the 2018-19 average.
It should however be noted that as a result of new recording procedures for 2020, even prior to the introduction of lockdown measures, these figures appear somewhat lower when compared to previous years.
NHS waiting times - 18 weeks referral to treatment (RTT)
There has been a substantial reduction in the overall number of eligible 18 weeks RTT waits reported from March onwards; dropping to a low of 27,900 in April before gradually increasing to 45,166 in June. The comparable figure for February was 94,481 (excluding NHS Grampian).
Chronic Pain Clinics
In the quarter ending 30 June 2020, 1,501 new patients were referred to a chronic pain clinic. This compares to 4,972 in the same quarter in 2019, a reduction of 69.8%.
In the same quarter, 547 patients were seen at a chronic pain clinic. This compares to 2,741 in the same quarter in 2019, a reduction of 80%.
Those waiting for a first appointment are also waiting longer. At the end of June 2020, 52.9% of patients had been waiting more than 18 weeks. This compares to 15.4% at end of June 2019 and 23% at end of December 2019.
Cancer Waiting Times
The 31-day standard states that 95% of all patients will wait no more than 31 days from decision to treat to first cancer treatment.
There were 5,056 eligible referrals within the 31-day standard in the period April to June 2020, a decrease of 23% on the same period in 2019.
97.1% of patients started treatment within the 31-day standard, compared with 96.1% in the previous quarter and 94.7% for quarter ending June 2019.
The 31-day standard was met by 14 NHS Boards. The only Board that did not meet the standard was NHS Grampian (94.5%).
The 62-day standard states that 95% of eligible patients will wait a maximum of 62 days from referral to first cancer treatment.
The 62-day standard was not met by any NHS Boards. NHS Boards’ performance ranged from 71.4% (NHS Orkney) to 94.9% (NHS Ayrshire & Arran).
There were 3,056 eligible referrals for the 62-day standard in the period April to June 2020, a decrease of 22% on the same period in 2019.
84.1% of patients started treatment within the 62-day standard, compared to 84.7% in the previous quarter, and 82.4% for quarter ending June 2019.
It is clear the impact of lockdown will have long lasting and far reaching medical impacts on the population. Only time will tell the extent of these and we support every effort being made to avoid future cessation of services and to address the inevitable backlogs and delays that have occurred.
We also learned of numerous changes and innovations to the delivery of services across all sectors and areas of health and social care. Much is mentioned throughout this report such as use of technology and care at home services as well as new ways to deliver services. Additionally, we heard decision making was streamlined with the emergence of strategic groups, quicker decision making with senior officials and leaders being empowered to make decisions subject to significantly less internal oversight and scrutiny.
We are aware that Health Boards and HSCPs have prepared remobilisation plans and would welcome further clarification on the basis of these plans and detail of when the backlog in treatments and waiting lists is expected to be resolved. It would also be helpful to know how any such plans might be affected by any return to emergency measures in the health system as a result of increased Covid-19 infections and admissions.
We urge the Scottish Government to produce a method by which the outcomes of patients delayed as a consequence of lockdown can be measured in order to assess for the future whether putting the NHS on an emergency footing is a proportionate response.
We also urge the Scottish Government, Health Boards and the IAs to take the opportunity presented to look at the innovative practices and processes that have been created across the country and ensure these are both embedded and shared widely.
Financial Stability of Health Boards
Brokerage and 3-year budgeting
In October 2018, the Scottish Government announced that Territorial Health Boards could plan their budgeting to break even over a three year timescale, rather than one year, with the flexibility to underspend or overspend by up to 1% of budgets in any one year.
The Scottish Government also stated they would not seek to recoup brokerage paid to territorial boards in the last five years leading to a total of £150 million being written-off in April 2019.
In 2019-20 however, four NHS Boards required additional financial support from the Scottish Government, with a cumulative total of £41 million:
NHS Tayside (£7 million);
NHS Ayrshire and Arran (£14.7 million);
NHS Highland (£11 million); and
NHS Borders (£8.3 million).
We understand these sums fall to be repaid along with any future brokerage payments required. We are not convinced the aim of all Boards returning to financial balance over the 3-year period with all brokerage repaid will be achieved and ask for confirmation the above remains the policy along with details of any anticipated brokerage payments for 2020-21.
Unachieved savings
A significant aspect of all boards budgeting plans is reflected in savings to be achieved both in-year and more permanently. The Scottish Government have estimated in budgetary forecasts savings should account for £1.7 billion of the overall health budget over the period 2016-17 to 2023-24. We understand that “routine financial planning and development of savings plans were temporarily paused” to address Covid-19 implicationsi although have now restarted.
We were also advised that all additional costs related to Covid-19 would be fully funded and given that position the Scottish Government indicated their expectation that boards would continue to deliver the saving trajectories that had been agreed.i A number of boards however indicated to us there were impacts on planned savings. For example Greater Glasgow and Clyde told us a large part of the costs associated with the pandemic were unachieved savings—the figure is about £70 million. Described as “the opportunity cost”, associated with spending time delivering Covid-19 services, then remobilisation rather than on saving money. Although we were also told that figure would likely come down over time.i
Falkirk IA told us savings targets were unlikely to be fully achieved this year. Work was underway to reassess the position and recommence savings schemes. In addition they were hoping to identify alternative savings arising from new ways of working adopted during lockdown.i
We ask the Scottish Government whether they consider unachieved savings are matters to be covered by Barnett consequentials and for an updated estimate of the level of unachieved savings across all boards and how those shortfalls will be funded in this and future financial years.
Covid-19 efficiencies and innovations
A number of witnesses and submissions indicated operational efficiencies had emerged as a consequence of changes required to address the pandemic. These range from working practices, with many indicating arrangements put in place were improvements on previous practice which had been sought over a lengthy period of time. Others include increased use of video consultations utilising Near Me, remote monitoring, other digital arrangements and decentralisation of decision making, the latter particularly for IAs.
We strongly support the decentralisation of decision making wherever possible and empowerment of leaders to make and be accountable for decisions. We also applaud other initiatives which have emerged as a consequence of the approach to the pandemic and ask the Scottish Government what financial assessment has been made of the implications of the changes which have emerged.
Financial Framework Longer-term financial stability and structures
In October 2018, the Scottish Government set out a Medium Term Financial Framework for Health and Social Care, covering plans for health and social care expenditure over the period to 2021-22 (or 2023-24 in some places).
We recognise the pandemic will have impacted on financial plans over the period of the Medium Term Financial Framework and acknowledge the Scottish Government have paused development of three year financial and savings plans.i
We ask the Scottish Government to indicate when they will be returning to the planning process, and when they intend to assess the impact of Covid-19 in terms of this financial year and the period reflected in the Medium Term Financial Framework.
The Medium Term Financial Framework also indicated an intention to seek “greater regional approaches to the planning and delivery of services”, noting that:
Based on evidence from other healthcare systems it is assumed that productivity savings of just over 1% could be delivered through effective regional working.
We ask the Scottish Government to indicate when they will be evaluating the productivity savings that could be made through Regional working and the extent to which these opportunities have increased as a consequence of learning during the pandemic.
GP attendance and use of hubs
We were also interested in the impact on GP practices and in particular any change in their workload as a consequence of the pandemic.
Community hubs and general practice
To help manage demand in the NHS allowing it to focus its efforts on treating those that need it most and as a method of triaging calls for assistance in relation to Covid-19 symptoms a dedicated telephone Community Hub services in each Health Board and over 40 assessment centres across Scotland were established. The Community Hub system which has cost £35 million to date is designed to meet local needs and ensures members of the public have access to the right kind of assistance as close as possible to where they live.
With NHS 24 as the key point of contact, Community Hub and Assessment Centres have since 23 March been providing wide-scale triage of patients with symptoms away from GP Practices and out of hours services towards Assessment Centres established exclusively to respond to patients with suspected Covid-19. Between 23 March and 12 August, 130,379 patients received a consultation through the hubs and assessment centres.
We were told the establishment of community hubs, and redirection of suspected Covid-19 cases has allowed GP practices to remain open, accessible and at the forefront of community services to deal with non-Covid-19 medical care throughout the pandemic.
Although patient demand initially reduced including a reduction in routine attendance and a reduction in the range of services GPs could refer to. Greater Glasgow and Clyde Health Board also told us of other demands on GPs including Care Home support as well as requests for mental health support.ii
The reality may be somewhat different. We have received numerous reports from constituents of GPs refusing to see people, including one case where a woman with a breast lump was refused a GP appointment. We have also heard numerous accounts of GPs indicating Covid-19 is the priority which leads us to wonder if Covid-19 patients are going through the hubs, what are GPs doing?
The Cabinet Secretary for Health and Sport advised us they were “actively considering how to use the community hubs and assessment centres infrastructure to help to redesign urgent care” and “it would be crazy to disband them and go back to the old ways of working”.iii Currently the impact of the community hub model on primary consultations in general practice has not been confirmed, we understand work is ongoing to better understand activity data in this area.
While the extent of such incidents is unclear we are clear there is a need to ensure consistency in service delivery and accessibility across GP practices with clear information being available to the public.
Financial impact
General practices are run by independent contractors who are funded according to patient lists rather than for providing individual services and consultations, and this model did not change during the pandemic.
Scottish Government provided additional funding of £20 million to directly support general practice and to ensure that practices stayed open during the April and May public holidays. That funding also ensured practices had sufficient funds to meet increased costs of staff absence, and were able to make adjustments to new ways of working during the pandemic. General practice income was also protected.i
While many general practice services were reduced or suspended during lockdown at the early stages of remobilisation, there were no reductions in running costs as general practice continued to operate throughout, providing as many services as could be safely provided remotely, including face-to-face services where deemed clinically necessary.i
GP workload
As indicated we have received correspondence from constituents about issues in contacting and accessing GPs and services during the pandemic and we asked Greater Glasgow and Clyde Health Board (GGCHB) about the workload of their GPs although we are aware from our other work that the workload and output of GPs is not measured.
The Chief Executive of GGCHB told us:
We set up the community assessment centres and the GP hubs. GPs have been supporting those processes, which means that they have had to augment or change their normal ways of practice working in order that they can help us in the community hubs and GP hubs. They have done significant additional work on top of their normal day job, and in a different way. GPs have supported the whole system across Greater Glasgow and Clyde very well. Had we not had the community assessment centres, GP hubs and so on, we would not have been able to separate the Covid-19 and non-Covid-19 pathways.i
Given the high volume of patients accessing the hubs and assessment centres it is unfortunate there continues to be no monitoring of GP regular activity delivered as part of core services. This prevents any examination of workload, any impact of the new contract to utilise multi-disciplinary teams and in this instance any examination of the changes in the use of practices by the public.
We note this is also an issue raised by GPs themselves. In a joint report compiled by BMA Scotland and Health and Social Care Scotland following a series of collaborative events across Scotland it is stated:
As you read throughout this report, lack of data within primary care is a significant and recurring theme, and as stated by one colleague “ We suffer from a lack of data, ED [Emergency Department] has data, acute has data, we don’t and we can’t keep discussions proportionate.ii
We will return to the subject of data and measuring GP productivity and outcomes in our forthcoming report on Primary Care.
At this time we ask the Scottish Government to bring forward evidence of what change there has been to GP throughput of patients during the pandemic together with details of the work undertaken in GP surgeries during the last 7 months.
How far has the Integration Agenda progressed?
The 2018 Audit Scotland update report into health and social care integration identified that Integration Authorities (IAs) are “operating in an extremely challenging environment and there is much more to be done”. It made a number of recommendations in six areas which we have consistently covered in our reports throughout this session:
Commitment to collaborative leadership and building relationships;
Effective strategic planning for improvement;
Integrated finances and financial planning;
Agreed governance and accountability arrangements;
Ability and willingness to share information; and
Meaningful and sustained engagement.
The Ministerial Strategic Group for Health and Community Care (MSG), Review of Progress with Integration of Health and Social Care agreed with the Audit Scotland recommendations commenting that the recommendations should be acted upon in full. It also acknowledges that “the pace and effectiveness of integration need to increase.i
That report was reviewed earlier this year including actions to address what were described as:
the stubborn lack of progress made with particular proposals.
Actions were agreed for each of the 25 proposals contained in the report.
We note the ongoing work by the Integration Leadership Group which was due to meet every 6 weeks and seek an update on the current position in relation to each of the 25 proposals.
Delayed Discharge
On 5 October 2016 we wrote to the then Cabinet Secretary for Health and Sport indicating:
Delivering reductions in the number of delayed discharges will be a key marker of the success of the new integrated system.i
Throughout this session we have been interested in understanding the reasons for the varying levels of delayed discharge. As we noted in last year’s budget report:
if this aspect of the health service is not managed effectively, it has serious implications for the overall budget.ii
We have highlighted the fluctuations in the number of persons delayed year on year and IA by IA and the reasons provided for delays. We observed that waiting for community care assessment, care packages or care home availability accounted for 75% of delays.iii And we also reported in last year’s report the estimated cost to the Health Service of £125 million in 2016/7 with an average daily cost per patient delayed of £234. Similar costs were reported for 2017-18 (total cost of £122 million and average daily cost per patient delayed of £248).
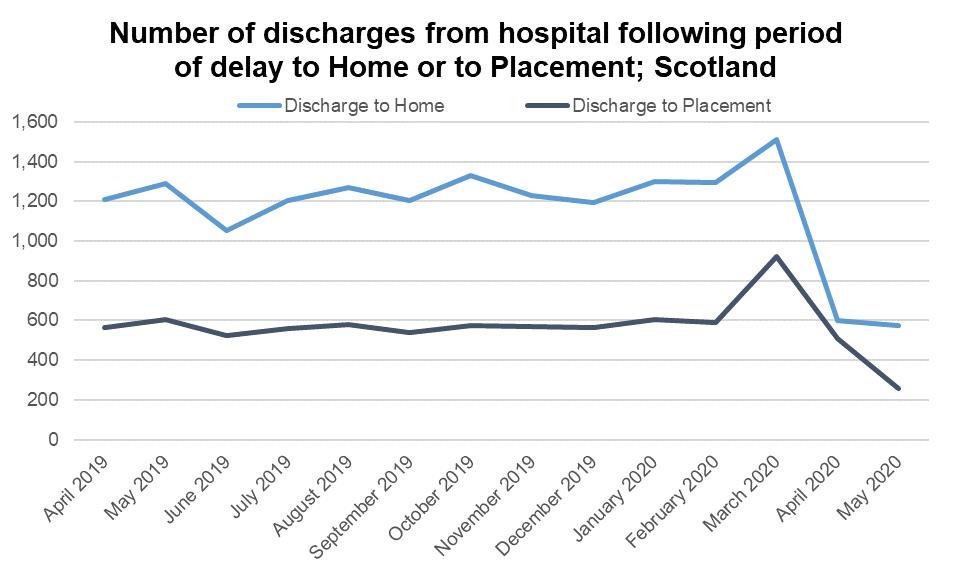
Section 16 of the Coronavirus Act 2020 allows for people to be moved out of hospital without the usual consultations to help manage pressures on the NHS. As a consequence of the Director General of Health and Social Care writing to all partnerships the number of people delayed in hospital fell dramatically from 1627 in February to 604 at the end of April as shown in the undernoted table.iv
The reductions were supported by funding of £50 million from the Scottish Government.v Numbers are however starting to rise again.
In the lessons learned reportvi it is stated Covid-19 was the stimulus to the removal of historic barriers as well as providing incentives for progress.
We applaud this seismic shift, along with the changes in attitudes and approaches that have allowed the reduction to occur. The challenge now is to maintain the reductions while tackling the remaining numbers many of whom are delayed as a consequence of legal difficulties.
In 2016 we suggested the problems caused by the Adults with Incapacity Act (AWI) leading to delayed discharges should be resolved quickly. We noted the Scottish Law Commission 2014 report on adults with incapacity which included a number of recommendations and contained a draft Bill which included changes to address the issues with the AWI Act. We are disappointed no action has been taken to address this otherwise intractable problem in this session and seek an update on the timetable for reform of this aspect of mental health legislation.
Having scrutinised the lessons learned document carefully, we welcome the many initiatives being shown and the efforts being made to import best practice from other areas in Scotland. We particularly applaud “home first” and “discharge to assess” initiatives and the roll out of intermediate care facilities.
There is however one area missing from that particular piece of work and this is an area we have also highlighted many times this session, namely that of preventative practices. While we are pleased to see the recognition of the cost implications highlighted in our budget report last year, we are clear that by far the most effective approach to both those delivering care and those who might need care is to provide early interventions to avoid or delay the need for care.
We are disappointed the report concentrates entirely on those requiring or receiving care and urge that a focus should be given to supporting people to keep them out of care. We very much support the comment from the Chief Executive of NHS Lothian who said:
Hopefully, we can start to have a sensible conversation about how we reduce demand and promote health rather than just treat ill health.v
We ask the Scottish Government to give prevention greater focus and to monitor closely initiatives across the country with prevention at their core ahead of the need for medical intervention and support. We would welcome the views of the Scottish Government on ways this can be addressed.
Engagement
We have previously raised concerns about a lack of effective engagement by IAs with stakeholders, as highlighted in our 2017 report on engagement. The Ministerial Strategic Group’s report also included a recommendation that “Effective approaches for community engagement and participation must be put in place for integration” and its November 2019 update rated progress against this recommendation as ‘amber’. The report commented that effective engagement:
…is critically important to our shared responsibility for ensuring services are fit for purpose, fit for the future, and support better outcomes for people using services, carers and local communities. Revised statutory guidance will be developed by the Scottish Government and COSLA on local community engagement and participation based on existing good practice, to apply across health and social care bodies. Meaningful engagement is central to achieving the scale of change and reform required, and is an ongoing process that is not undertaken only when service change is proposed.
In correspondence following our 2020/21 budget consideration the Cabinet Secretary for Health and Sport told us work to produce statutory guidance for Health Boards and IAs had been paused to allow work in responding to Covid to be prioritised. But this position would be reviewed "once the impact of Covid-19 becomes clearer".i
Given the importance of engagement, increasingly so when resources are stretched with more people waiting for treatment and support we would welcome an update on when the statutory guidance will be available and in force.
Social Prescribing
At the end of 2019 we completed our inquiry into social prescribing and reported our understanding of how social prescribing for sport and physical activity could improve the health and wellbeing of people in Scotland. Our report explored key opportunities for the wider health and social care system including:
the role of sport and physical activity in preventative health care as well as self-care for health and wellbeing;
the role of the GP and the multi-disciplinary team in exercise referral or encouraging self-care and self-management; and
how social prescribing for sport and physical activity has been used in health and social care and how this can inform the way future services are managed and delivered.
We also considered some of the barriers to, and drawbacks of, social prescribing as a means for increasing levels of physical activity, exercise and sporting participation levels.
Our conclusions were:
We have no doubts about the significant role physical activity and sport, and social prescribing, can contribute as part of preventative care for health and wellbeing. Addressing accessibility to, and awareness of, community and voluntary schemes will improve individuals' health and wellbeing outcomes, begin to shift the balance of care from acute to community settings and help achieve national outcomes.
Social prescribing and primary prevention approaches can help in preventing long term conditions and dependence on pharmaceutical prescriptions. They also have the potential to ease the pressure on existing health and social care services, as well as reducing waiting times, unplanned admissions to hospital and delayed discharges.
We found that the health and social care system needs to maintain its focus on improving public health and the development of preventative models of care (including self-management). If we want it to be financially sustainable, tackle persistent health inequalities, improve long-term outcomes and reduce pressure on the workforce. We cannot simply react to the management of patients with long-term conditions without taking long-term action across the health and care system as a whole.
Having established compelling financial and health benefits arising from social prescribing of physical activity, and wider preventative activity, we reported that we expected a significant proportion of each Integration Authority budget should be spent on commissioning local services to increase physical activity levels and improve health in communities. We recommended that figure be not less than 5% and this target be achieved within 2 years.
Our report was debated and approved by Parliament on 18 February this year. Subsequently, on 25 February, we heard from the Cabinet Secretary for Health and Sport as part of our budget scrutiny for the current year when she indicated she was happy to discuss our recommendation that 5% of the IA budget be spent on social prescribing while also noting spending on social prescribing was not exclusively a matter for the health and sport budget.i
In preparation for this budget inquiry we sought information from each IA as to the amount they are spending on social prescribing and received the following figures from those who responded:
IA Amount Reported Aberdeenshire 886,000 Aberdeen 700,000 Angus 475,000 Argyll and Bute 30,000 Clackmannanshire and Stirling nil Dumfries and Galloway 1,120,000 Dundee 1,460,000 East Ayrshire 568,000 East Dunbartonshire 201,000 East Lothian 274,000 East Renfrewshire 349,000 Edinburgh 1,100,000 Falkirk 466,000 Glasgow 6,770,000 Inverclyde 362,000 Midlothian No figure provided Moray 539,000 North Ayrshire 540,000 North Lanarkshire 949,000 Perth and Kinross 208,000 Renfrewshire 330,000 Scottish Borders No figure provided Shetland 55,000 South Ayrshire 159,000 South Lanarkshire 749,000 West Dunbartonshire 121,000 West Lothian 1,040,000 Western isles 110,000 Total 19,561,000 No replies were received from Orkney or Highland council.
The total reported spend is just over £19.5 million which represents significantly less than 1% of the IA budget for 2020/21 and we ask the Scottish Government again to support our ambition noting the title of our earlier report that “physical activity is an investment not a cost.”
We also ask that Public Health Scotland work with IAs to champion an increased share of total spend on social prescribing to the levels recommended in our report last year.
Shifting the Balance of Care
The integration of health and social care is intended to bring about a shift in the balance of care, from hospital to community care. The Scottish Government’s stated aim is that, by the end of this Parliament, at least 50% of spending will take place in Community Health Service. In its Medium Term Health and Social Care Financial Framework, the Scottish Government estimated that, on the basis of 2016-17 data, 49.1% of frontline health spending is in community health services. This is expected to rise to 50.5% by 2021-22. The integration authorities are considered to be an important vehicle for making progress in this area.
Although only a modest change is required in order to meet the Scottish Government commitment, we have previously heard evidence about the challenges involved in even standing still against this measure, given the demographic pressures, rising demand and prescribing costs. In oral evidence sessions and in written submissions received by us despite quite significant changes in service delivery, there has not been any evidence of a significant shift in the balance of care, or any expected reduction in the set aside budget. However, there appears to be an expectation that the coronavirus pandemic might have led to changes that could see progress in achieving this shift.
In evidence on 11 August 2020i, Richard McCallum, interim director of health finance and governance at the Scottish Government said:
We have talked about shifting the balance of spend and have provided evidence in the past about how we see that happening. I am quite keen to see how that can be accelerated as a result of Covid so that the funding follows the patient pathways that we will look to put in place in the most appropriate way.
Later we heard from IA chief officers on a range of initiatives in relation to the delivery of services differently, many not involving attendance at buildings and were told "it would be a real shame if we reverted to a system that was heavily weighted towards and dependent on buildings and infrastructure …….. particularly given the difference that we have experienced over the past few months".i With people in Dundee only being asked to "attend buildings for assessment, treatment and care" where there was no other alternative. i
We were told of specialist clinicians now providing care in peoples homes working closely with GPsi and of the need to retain such changes and innovations with but in from the specialists.
We ask the Scottish Government whether, in the light of the changes and innovations seen during the pandemic, it would expect to see further shift beyond the 50% target (and what target do they now consider should be achievable).
Set Aside Budget
We have pursued the issue of set aside budgets for a number of years hearing repeatedly that the ‘set aside’ budget is treated as being under the control of the NHS board, rather than the IJB, with the result that it is difficult for IJBs to use the money to shift from acute hospital care to community-based and preventative services.
This issue has been flagged by Audit Scotland and the Ministerial Strategic Group on Health and Community Care, with the view that failure of set aside budgets to operate as intended is hampering the progress of integration.
In our budget report last year we said it was unacceptable four years after integration that set aside budgets continue to be problematical and that we expected all issues to be resolved by the end of [the last] financial year with clear identification of released sums reported quarterly.i
The Cabinet Secretary told us plans had been agreed with COSLA to make improvements to set-aside budgets. Plans have been stalled as a consequence of Covid but there is no disagreement about the importance of the approach or of picking it up as soon as possible.ii
We anticipated this would be the position and asked IA chief officers for their views on whether set-aside was working effectively. We heard:
The focus should be on what it is that we want to do and what we want to change, and the budget should follow from that.ii
We also heard the focus should be wider than the set aside budget with Vicky Irons chief officer Dundee Health and Social Care Partnership explaining a wider and more ambitious approach:
In addition, it is only a slice of the acute activity that we want to tackle in a different, more integrated way. I am far more interested in having discussions about the total resource; I use the word “resource” rather than “budget”, because we see change through people. If we can have an upfront adult conversation about the total resource, where that needs to be and how we can genuinely shift the balance of care into the community, after the experience that we have all just lived through, that is where we need to focus our attention, rather than trying to increase the figure that is nominally indicated in our set-aside budget.ii
The Committee would welcome an update on progress towards achieving the intended operation of the set aside budget and would also welcome any examples of the set aside budget operating effectively, with resources being directed by the IA rather than the Health Board.
Care Inspectorate
This part of our report focusses on the role of the Care Inspectorate (CI) during the pandemic. The CI is an executive non-departmental public body who operate independently from Scottish Ministers and were created to:
protect the users of social care services;
to encourage a diversity of services;
to promote the independence of users of care services; and
to identify and promote good practice in social care.
Alongside this broad remit, the CI registers and inspects care services for children and adults. They play a role in supporting improvement in care services and local planning and health and social care partnerships.
The CI's strategic objectives are:
We will give public assurance and build confidence that social care and social work in Scotland is rights-based and world-class, through robust and independent scrutiny and improvement processes.
We will inform local and national policy to contribute to ensuring a world-class care system in Scotland, through intelligence-led, risk-based, and evidence-based approaches to scrutiny and improvement.
We will support people’s understanding of high quality, safe and compassionate care by promoting standards and quality of service they should expect and help make sure their voices are heard.
We will perform as an independent, effective and efficient scrutiny and improvement body, working to consolidate excellence, deliver cultural change, invest in a competent, confident workforce and work collaboratively with partner agencies to support the delivery of safe and compassionate, rights-based care.
We held the session with CI partly as part of our scrutiny of actions and activity during the pandemic, partly as part of our ongoing scrutiny work across all public bodies falling within our report and as a precursor to our inquiry into social care. The session was followed up by written correspondence and the detailed exchange can be found here. Our report later in the session on social care will consider more detailed aspects of their scrutiny and inspection role.
The inspection work of the CI has been heavily curtailed during the pandemic and we took evidence from them on 25 August, a session which was preceded by our conducting a short survey asking stakeholders two questions:
‘Considering the pandemic, and its impact on social care services, what role should the Care Inspectorate have in ensuring those receiving adult care and support services are better protected?’.
‘What role should the Care Inspectorate have in creating a more resilient and sustainable adult social care sector?’.
There were around 80 responses providing us with a picture of experience and insight during the pandemic.i
CI told us their role during the pandemic had changed as they moved more to remote monitoring and had adapted their approach. The Scottish Government said the organisation had been repurposed and becoming more intelligence led while providing support to care services working in partnership with others.ii We were particularly interested in any leadership role they had occupied to support the sector and in particular care homes and care at home services.
The submissions we received painted a mixed picture of an organisation that came under the spotlight. The Coalition of Care and Support Providers Scotland (CCPS) had concluded that the role of the CI during the pandemic should be:
supporting the continued provision of social services through reduction of administrative burden previously associated with regulatory requirements, whilst ensuring that any infection prevention control (IPC) measures taken to reduce risk of infection are done in a manner consistent with the Health and Social Care Standards.
Scottish Care suggested:
the Care Inspectorate should have been at the forefront of communications, guidance, inspections and the sharing of best practice guidance in the context of the Care Standards (not only infection control).
This in the context of providers receiving multiple sources of information and guidance. While recognising the focus on health and infection control they noted this had come at a damaging price to the wellbeing of supported individuals leading to an overly medicalised and clinical approach in what are peoples homes.
We agree with Scottish Care when they say:
it would appear that an opportunity has been missed for the Care Inspectorate to provide a reliable and accessible main point of access for routing of information to services.
We were disappointed to hear the emphasis being given to their role as inspection, scrutiny and improvement and note the first line of their first objective to “ give public assurance and build confidence that social care and social work in Scotland is rights-based and world-class” considering that can only be achieved by going further than “through robust and independent scrutiny and improvement processes”.
We also note the Scottish Government in its COVID report (3rd Report), retained the emergency power to intervene to ‘safeguard the life, health and wellbeing of care home residents’. And we considered whether this should be a role for the Care Inspectorate and suggest that there is a need for the CI to have strengthened powers in this regard.
We further suggest the Scottish Government consider the need for a sector focal point and whether the Care Inspectorate, given their insights through the inspection and scrutiny role is the appropriate organisation to undertake that position.
One further area of comment in relation to the CI relates to their relationships with the IA’s. We were disappointed to learn that 5 years into integration they have completed only 8 inspections of IA’s out of the 31 that exist. We would have expected given the fundamental role of the IA’s in the commissioning and delivery of social care there is a need for a greater engagement and monitoring.
We would have expected given the fundamental role of the IA’s in the commissioning and delivery of social care there is a need for a greater engagement and monitoring. We ask the Scottish Government for their views on the benefits of assessment and the regularity with which they consider they should occur.
We ask the Scottish Government for their views on the benefits of assessment of the IAs and the regularity with which they consider they should occur.
Covid-19 international travel and quarantine
To protect against the risk of imported cases of coronavirus, the Scottish Government made regulations requiring travellers to self-isolate for 14 days when arriving in Scotland from a country outside the Common Travel Area (UK, Republic of Ireland, the Channel Islands and the Isle of Man).
The self-isolation rules apply to all travel to Scotland, by train, ferry, coach, air or any other route whether arriving directly or via another part of the UK.
The Regulations set out a list of exempt countries or territories from which travellers are not required to self-isolate. This list is continuously reviewed by the Scottish Government and we have been considering weekly revisions to the regulations to take off or add countries.
Uniquely and given the Public Health focus these Regulations come into force automatically when made by Ministers and prior to any Parliamentary scrutiny. We have taken a close interest in the operation of these regulations and their enforcement both the cost and time impacts of enforcement and the consequential impact on other activities such as the tracing centre.
Public Health Scotland contacts all individuals, via email, who require to self-isolate, on their return from a country not exempt from quarantine. The National Contact Tracing Centre subsequently contacts a sample of those individuals to confirm they are quarantining at the address provided.
The following statistics provide a summary of the number of passengers entering Scotland from outside the UK, those required to quarantine, and the numbers contacted by the National Contact Tracing Centre. Details of passenger arrivals into Scotland are provided by the Home Office to Public Health Scotland (PHS). PHS then take a sample of those passengers who are required to quarantine and pass the data to NHS National Services Scotland, which runs the National Contact Tracing Centre. The final column for the week ending 18 October is information provided to us by the Minister for Public Health in evidence on 27 October.i
Table 5: Quarantine Statistics by date
Cumulative Total 22 Jun to 4 Oct Latest Week to 4 Oct Week ending 18 Oct Number of people arriving in Scotlandi 369,088 26,883 27,340 Number of people requiring to quarantineii 115,984 9,203 15,157 Number of people contacted by National Centreiii 7,376 822 3,132 Of the total number of people contacted by the National Centre, Table 6 shows the breakdown of these contacts.
Table 6: Number of people contacted by National Centre by status.
Cumulative Total (22 Jun to 4 Oct) Latest Week (to 4 Oct) Successful contacts madeiv 5,915 558 Unable to contact individualv 1,410 213 In progressvi 51 51
In the course of considering quarantine regulations we have also questioned the Cabinet Secretary for Justice on a number of areas around the approach to identifying affected and non-affected countries, Parliamentary processes for consideration and review and the enforcement of the regulations.
We requested the Cabinet Secretary to consider taking a more nuanced and regional approach to determining future designations and we are pleased to note this is starting to occur.
We heard from the Cabinet Secretary in August that only a small proportion of people required to quarantine were subject to any follow up contact after receipt of an initial e-mail. A target of up to 20% had been provided for the numbers to be followed up with a maximum capacity of 450 set although that figure had been exceeded. The Cabinet Secretary also indicated he would like to go further than the 450 capacity, towards the 20% target. During the 2 weeks to 24 August we were told around 16,000 people entering Scotland had become liable to quarantine. And in October the number was similar being just over 15,000.i
We consider, given the emergency nature of these regulations, and the danger posed to the Scottish public that there is a high risk of infection being brought to Scotland from travellers arriving here carrying the virus.
We consider it vital, given the restrictions imposed on the Scottish public, that every effort is made to prevent importation of the virus into Scotland by travellers. Identifying, checking and tracing those persons subject to quarantine requires to be given the highest priority and the numbers being followed up must be substantially increased to reach in excess of the target figure.
We further consider there would be benefits to testing passengers on arrival both as a health protection measure and as a means to shorten the required period of quarantine. We ask the Scottish Government for their views on these approaches.
Annexe A
Extracts from the Minutes of the Health and Sport Committee Meetings
3rd Meeting, 2020 (Session 5) Tuesday 4 February 2020
3. Budget Scrutiny 2021-22 (in private): The Committee considered and agreed its approach to the scrutiny of the Scottish Government's Budget 2021-22.
19th Meeting, 2020 (Session 5) Tuesday 11 August 2020
1. Pre-Budget Scrutiny: The Committee took evidence as part of its Pre-Budget Scrutiny from—
Elinor Mitchell, Interim Director General Health and Social Care, and
Richard McCallum, Interim Director of Health Finance and Governance, both from Scottish Government.
2. Pre-Budget Scrutiny (in private): The Committee considered evidence heard earlier in the meeting.
20th Meeting, 2020 (Session 5) Tuesday 25 August 2020
9. Pre-Budget Scrutiny: The Committee took evidence as part of its Pre-Budget Scrutiny from—
Peter Macleod, Chief Executive; and
Kevin Mitchell, Executive Director of Scrutiny and Assurance, both from Care Inspectorate.
11. Pre-Budget Scrutiny (in private): The Committee considered the evidence heard earlier in the meeting.
21st Meeting, 2020 (Session 5) Tuesday 1 September 2020
1. Pre-Budget Scrutiny: The Committee took evidence as part of its Pre-Budget Scrutiny from—
Hazel Borland, Interim Deputy Chief Executive/Nurse Director; and
Derek Lindsay, Director of Finance, both from NHS Ayrshire and Arran.
5. Pre-Budget Scrutiny (in private): The Committee considered the evidence heard earlier in the meeting.
22nd Meeting, 2020 (Session 5) Tuesday 8 September 2020
1. Pre-Budget Scrutiny: The Committee took evidence as part of its Pre-Budget Scrutiny from—
Judith Proctor, Chief Officer, Edinburgh Health and Social Care Partnership;
Vicky Irons, Chief Officer, Dundee Health and Social Care Partnership; and
Eddie Fraser, Chief Officer, East Ayrshire Health and Social Care Partnership.
4. Pre-Budget Scrutiny (in private): The Committee considered the evidence heard earlier in the meeting.
23rd Meeting, 2020 (Session 5) Tuesday 15 September 2020
5. Pre-Budget Scrutiny: The Committee took evidence as part of its Pre-Budget Scrutiny from—
Jane Grant, Chief Executive, and Mark White, Director of Finance, NHS Greater Glasgow and Clyde;
and then from:
Calum Campbell, Interim Chief Executive, and Susan Goldsmith, Director of Finance, NHS Lothian.
7. Pre-Budget Scrutiny (in private): The Committee considered the evidence heard earlier in the meeting.
24th Meeting, 2020 (Session 5) Tuesday 22 September 2020
5. Pre-Budget Scrutiny: The Committee took evidence as part of its Pre-Budget Scrutiny from—
Joe FitzPatrick, Minister for Public Health, Sport and Wellbeing; and
Richard McCallum, Interim Director of Health Finance and Governance, both from Scottish Government.
7. Pre-Budget Scrutiny (in private): The Committee considered the evidence heard earlier in the meeting and agreed to issue an invite to Jeane Freeman, Cabinet Secretary for Health and Sport to give oral evidence on 29 September 2020.
25th Meeting, 2020 (Session 5) Tuesday 29 September 2020
2. Pre-Budget Scrutiny: The Committee took evidence as part of its Pre-Budget Scrutiny from—
Jeane Freeman, Cabinet Secretary for Health and Sport; and
Richard McCallum, Interim Director of Health Finance and Governance, both from Scottish Government.
4. Pre-Budget Scrutiny (in private): The Committee considered the evidence heard earlier in the meeting.
28th Meeting, 2020 (Session 5) Tuesday 3 November 2020
8. Pre-Budget Scrutiny (in private): The Committee considered and agreed a draft report on its Pre-Budget Scrutiny 2021-22.
Annexe B
Written evidence
Call for views: How well is the Care Inspectorate fulfilling its statutory roles?, published responses.
Health Board Budget pro-formas:
Health and Social Care Partnerships pro-formas:
Supplementary written evidence
Letter to Scottish Government officials from the Convener - 21 August 2020
Letter from Elinor Mitchell, Interim Director General Health and Social Care - 1 September 2020
Letter to the Care Inspectorate from the Convener - 3 September 2020
Letter from the Care Inspectorate to the Convener - 24 September 2020
Letter to NHS Ayrshire and Arran from the Convener - 10 September 2020
Letter from John Burns, Chief Executive, NHS Ayrshire and Arran to the Convener - 25 September 2020
Letter to Vicky Irons, Chief Officer, Dundee Health and Social Care Partnership - 24 September 2020
Letter to Calum Campbell, Interim Chief Executive, NHS Lothian from the Convener - 7 October 2020
Letter to Jane Grant, Chief Executive, NHS Glasgow from the Convener - 7 October 2020
Letter from Calum Campbell, Interim Chief Executive, NHS Lothian to the Convener - 20 October 2020
Official Reports of meetings of the Health and Sport Committee
Tuesday 11 August 2020 - evidence from the Scottish Government
Tuesday 25 August 2020 - evidence from the Care Inspectorate
Tuesday 1 September 2020 - evidence from NHS Ayrshire and Arran
Tuesday 8 September 2020 - evidence from Integrated Joint Boards/Health and Social Care Partnerships
Tuesday 15 September 2020 - evidence from NHS Greater Glasgow and Clyde and NHS Lothian
Tuesday 22 September 2020 - evidence from the Scottish Government
Tuesday 29 September 2020 - evidence from the Scottish Government