Health and Sport Committee
Looking ahead to the Scottish Government - Health Budget 2019-20: Is the budget delivering the desired outcomes for health and social care in Scotland?
Introduction
The Finance and Constitution Committee has a new written agreement with the Scottish Government on the budget process which the Scottish Parliament debated and agreed on 8 May 2018. It sets out a full year budgeting process and an outcomes-based approach to scrutiny. i
For the Health and Sport Committee, these developments have not necessitated a major revision to current practice, as we have for some years undertaken elements of budget scrutiny throughout the year.
This year the health budget has been explored in a number of inquiries we have conducted including NHS Governance, Technology and Innovation in Health and Social Care and Preventative Agenda. Budget considerations have also been an important component of our evidence sessions with special health boards and territorial boards looking at their performance, the outcomes delivered and the added value each body provides. This work is intended to help us understand and, where necessary, influence the content of the future budget and the relative priorities given to the health elements.
We have also conducted some specific pre-budget scrutiny. We have returned to the theme of budget transparency, which we explored in our 2017 pre-budget report and considered two further themes. The first theme being the strategic direction of financial planning, taking account of high level, longer-term planning set out in Scottish Government documents. The second theme being the progress with financial aspects of integration, building on issues raised in previous budget scrutiny sessions.
To inform our work we issued to all integration authorities a short survey regarding their budgets. We also held an oral evidence session on 22 May with representatives from the following integration authorities: Scottish Borders, East Ayrshire, Moray, Edinburgh and North Lanarkshire. These integration authorities also provided written evidence in advance of the meeting.
We also took evidence from the Scottish Government. On 5 June we held an oral evidence session with Paul Gray, Director-General Health & Social Care and Chief Executive NHSScotland. The Director-General was accompanied by Christine McLauglin, Director of Health Finance, Shirley Rogers, Director of Health Workforce and Strategic Change, Dr Catherine Calderwood, Chief Medical Officer and Alison Taylor, Head of Integration Division.
The timing of this report, in advance of the publication of the Scottish Government’s Budget, is to give the Scottish Government time to consider implementing our recommendations in its forthcoming budget 2019-20.
We intend to hold an evidence session with the Cabinet Secretary for Health and Sport following the publication of the budget. This report focuses on the health aspect of the budget although it is envisaged that the evidence session with the Cabinet Secretary will cover both the health and sport portfolios.
Budget Transparency
Our Pre-budget report last year was titled ‘Looking ahead to the Scottish Government Health and Sport Draft Budget 2018-19: A call for greater transparency’ i ("Pre-budget report 2017") As the title indicates the report called for greater transparency and availability of information relating to the health and sport budget to assist with our scrutiny function. We are interested in establishing the criteria on which funding decisions are made and what outcomes the funding the Parliament approves is achieving.
Integration authorities
Our Pre-budget report 2017 raised specific concerns regarding accessing comprehensive and timely data on the budgets of integration authorities ("IAs"). We were critical then that there was a lack of transparency regarding the allocation of over £8bn of public investment to integration authorities and we called for a breakdown of this figure to individual integration authority level.
In response the then Cabinet Secretary for Health and Sport, Shona Robison wrote to us on 12 December 2017 and committed to publishing regular financial monitoring information on integration authorities' budgets and spend.i
In our post-budget evidence session on 9 January 2018 with the then Cabinet Secretary for Health and Sport, Shona Robison, Christine McLaughlin, Director of Health Finance said—
“There is a lot about transparency in the report that the committee produced in December, and we have introduced a number of measures to make it easier to understand and get information about spend, including planned spend. We have also agreed with the integration authorities that, from February, we will start consolidated reporting on spend.”ii
We subsequently wrote to the Cabinet Secretary for clarification on the nature and timing of information to be provided and received a response with some further detail.
On 2 May 2018, the Cabinet Secretary wrote to us and provided the first consolidated report on integration authority finances, including details of spending on mental health and Alcohol and Drug Partnerships, providing a 2017-18 year end position.iv
The Cabinet Secretary also committed to engaging in ongoing dialogue over the content and format of these reports to ensure that they were of value to us in our scrutiny work.
On 22 August 2018, integration authorities provided the second of their quarterly consolidated financial returns, which are the Pre Audit Out-turn for 2017-18. The third consolidated financial returns were published on 28 September.v
Subsequent reports are expected in December 2018 and March 2019.
In our evidence session with IAs they welcomed the publication of the quarterly financial updates as a tool for benchmarking performance and enabling learning across IAs.
Pam Gowan of Moray Health and Social Care Partnership said—
“We need to understand the detail of what lies beneath the information. The process, which stimulates debate and allows us to ask more questions, will be very useful”. vi
NHS Boards
Another area of progress made since the publication of our Pre-budget report in November 2017 has been the provision of information on NHS Board Local Delivery Plans (LDPs). The Scottish Government originally indicated it would provide quarterly financial updates based on the LDPs.
In June 2018 Jeane Freeman, Cabinet Secretary for Health and Sporti wrote to us to provide the current financial position of NHS boards and indicated this information would now be published monthly.ii
The information contained in these monthly updates includes the monthly financial position for NHS Scotland for the reporting year 2018-19. It also sets out the year to date position and the forecast position for the year end.
We have recommended in numerous budget reports the need for improved transparency in the Scottish Government’s budget. We have previously made calls for further information to allow us and the Parliament to understand and scrutinise the extent to which the allocation of budgets reflects the Scottish Government’s stated priorities for health and sport and ultimately whether the recipients are delivering the intended outcomes. Until now, not having access to basic information on budget allocations for integration authorities has made fulfilling our scrutiny function difficult.
We welcome the commitment made by the Scottish Government to provide consolidated financial reports on integration authorities on a quarterly basis to us and the work of integration authorities in compiling this information. We also welcome the improvement in the frequency of reporting on the financial position of NHS boards. We believe, over time, provision of this information will assist in assessing patterns and trends in investment.
We are pleased that integration authorities consider these financial reports to be helpful for benchmarking performance and enabling learning across IAs. We ask for further information on how the Chief Officers’ Network and Chief Finance Officers’ Group intends to use this information and what changes it expects to see as a result.
We encourage the Scottish Government to consider whether it would be practical for the provision of financial information on integration authorities to be provided on a monthly basis in line with the frequency of the provision of information at an NHS board level.
Ultimately, we are interested in establishing the criteria on which funding decisions are made and what the funding is achieving. We discuss later in this report the limited progress made by integration authorities in reporting budgets against the nine national health and wellbeing outcomes. We believe greater linkages need to be made between the investment, outputs and performance in delivering services by integration authorities and NHS boards
We expect this step change in approach to information provision from the Scottish Government and integration authorities to be built upon to include information on outputs and outcomes.
We need to not only be able to establish the budget allocation but the impact and outcome of the investment. This information is essential to allow the Committee and the Parliament to understand and constructively comment on policy priorities and allocation of resources.
Financial Planning
A key focus of our pre-budget scrutiny was consideration of whether the financial frameworks were in place to enable long-term financial planning by the health and social care sectors.
The Budget Process Review Group recommended that the Scottish Government should adopt a more strategic approach to financial planning— “setting out its expectations and broad financial plans/projections for at least the next five years”. The intention was that this document would allow parliamentary committees “to consider the overall fiscal context and the financial implications of existing government policies over the years”.i
The Committee has also made repeated calls for long-term budget planning for the health portfolio. Our Pre-budget report 2017 explained improvements in long-term budget planning would in turn support effective decision making and delivery of the Scottish Government's Performance Framework.
In the evidence session on 22 May 2018 integration authorities commented on the value of a longer-term financial framework.
Janice Hewitt of North Lanarkshire Health and Social Care Partnership told us “If I were to ask for anything, I would implore for guaranteed approximate budgets. […] A five-year approximate budget would be great for us”.ii
Eddie Fraser of East Ayrshire Health and Social Care Partnership spoke about the difficulties not having a long term financial plan presented for workforce planning and in determining investment in buildings and technology. He suggested longer-term financial planning could also assist in delivering changes in practice.ii
Pam Gowans of Moray Health and Social Care Partnership also suggested longer-term planning could support service redesign—
“Longer-term planning gives confidence in decision making. When we are having critical conversations with communities, highlighting the trajectory that we are on and the system that we need to redesign, longer-term planning allows us to be confident in setting clear parameters.”ii
Eddie Fraser added that it was possible to strategically plan at the moment without longer-term financial plans as the reality was their budgets would only move by a few percentage points on an annual basis, with upwards of 95% of the budget being known. He explained, however, that given the size of the budgets the remaining 5% would be a large amount of money. He suggested longer-term financial planning would offer an improved “level of surety” to their partners including the third sector and in ensuring IAs delivery of preventative approaches.iii
Scottish Government Medium Term Financial Strategy
Following the Committee's evidence session with integration authorities the Scottish Government published on 30 May 2018 its first Medium Term Financial Strategy (MTFS). It restated the plan to increase resource spending on the NHS by £2 billion over the course of this Parliament (2016-17 to 2021-22).
The MTFS also restated the commitment to pass on all health resource Barnett consequentials.
The UK Government subsequently announced plans for increased investment in the NHS in England which will result in Barnett consequentials for the Scottish Government. The anticipated Barnett consequentials for the period 2019-20 to 2021‑22 total £1.32bn. This is more than the Scottish Government’s planned uplift of £1.26bn over the same period, as set out in the May 2018 MTFS. As such, the Scottish Government’s plans outlined in the MTFS could be achieved without any further action beyond passing on the anticipated Barnett consequentials.
Scottish Government Medium Term Health and Social Care Financial Framework
In October 2018 the Scottish Government published its Medium Term Health and Social Care Financial Framework [Financial Framework].i
The Cabinet Secretary’s Ministerial Statement to the Scottish Parliament set out a new three-year financial plan and performance framework for NHS territorial boards.ii
The Cabinet Secretary detailed NHS boards will be required to deliver a break-even position over a three-year period, rather than annually as is the case currently. She also explained that in each year, boards will have 1% flexibility on their annual resource budget to allow them scope to marginally underspend or overspend in that year. She told the Parliament this would be accompanied by the Scottish Government writing off all outstanding brokerage from NHS boards. No reference was made to the approach or any sanctions the Scottish Government would take if boards failed to deliver a break-even position.
The Financial Framework provides confirmation of four main health and social care expenditure commitments. The Framework states-
“Over the course of this parliament, baseline allocations to frontline Health Boards will be maintained in real terms, with additional funding over and above inflation being allocated to support the shift in the balance of care. This means that health expenditure will be protected from the impact of rising prices and will continue to grow in excess of GDP deflator projections;
Over the course of the next five years, hospital expenditure will account for less than 50% of frontline NHS expenditure. This relates to the policy commitment to ‘shift the balance of care’ with a greater proportion of care provided in a setting close to a person’s home rather than in a hospital;
Funding for primary care will increase to 11% of the frontline NHS budget by 2021/22. This will amount to increased spending of £500 million, and about half of this growth will be invested directly into GP services. The remainder will be invested in primary care services provided in the community; and
The share of the frontline NHS budget dedicated to mental health, and to primary, community, and social care will increase in every year of the parliament. For adults, and in some cases for children, these services, along with unscheduled hospital care, are now managed by integration authorities.”i
The Financial Framework also considers the factors driving expenditure on health and social care and the rates of growth and reform for health services. The Financial Framework states that future demand projections for health have been based on an annual growth rate of 3.5% in the cash budget. It also refers to an increase of £1.5bn in spending on frontline NHS boards over the period 2016-17 to 2021-22.i
The Institute for Fiscal Studies and Health Foundation estimate that UK spending on healthcare will have to rise by an average of 3.3% a year in real terms over the next 15 years just to maintain NHS provision at current levels, and that social care funding will need to increase by 3.9% a year in real terms in order to maintain current provision. As with the Scottish Government calculations, these projections assume that productivity improvements will deliver savings over the period and act to offset the spending increase that would otherwise be required.v
We welcome the announcement by the Scottish Government of a move to a three-year financial planning cycle as this is something we have made repeated calls for over a number of years. We welcome the introduction of more financial flexibility for NHS boards. Ultimately, we wish to ensure that improvements in long-term budget planning in turn support effective decision taking and delivery of the Scottish Government's Performance Framework. We ask the Scottish Government for further information on what changes it expects to see NHS boards make as a result of the move to three-year budget management. We also request further information on how it will monitor the implementation of this change in approach. And what actions it proposes to take against any Boards who fail to meet or are considered to be on a trajectory to fail to break even.
During the course of our pre-budget scrutiny IAs commented on the value of having a longer-term financial plan. A short-term input focused budget process does not support the development of genuine reform. The Committee believes it would be beneficial for integration authorities to have more longer-term financial plans. We ask the Scottish Government to respond to the concerns raised by IAs. We also ask for clarification on what impact it expects the move to three-year budget management for health boards will have on IAs approach to budget setting, for example whether it will improve timescales for agreement on the budget.
We have noted in previous inquiries that budgets are increased at various times during the year to take account of changes and initiatives introduced. We heard when taking evidence from NHS Greater Glasgow and Clyde this, in part, is anticipated when they set their budget although there is no guarantee of exact sums that may be allocated. We are concerned the receipt of additional funds on a seemingly ad-hoc basis during the year does not assist prudent budget management. We ask the Scottish Government how this will be affected by the move to longer-term budgeting.
We also welcome the publication of the Scottish Government's Medium Term Health and Social Care Financial Framework. The framework provides confirmation of the four key health and social care expenditure commitments. To assist scrutiny, it would be helpful if regular progress updates were provided for each commitment and that definitions are clear e.g. for what is included in the definition of primary care.
We note the concerns raised in evidence about the merits of longer-term financial planning. We recommend the Scottish Government clearly set out and specify for each NHS board planned health expenditure over the course of this Scottish Parliament taking account of the commitments made in the Framework.
The Framework contains a range of figures using different definitions and covering different time periods. In advance of publication of the Budget it would be helpful if absolute clarity could be provided on the detail that it contains. This will assist us when we consider the actual budget proposals.
One area in particular is clarification on the increase in spend on the NHS in Scotland. The Medium Term Financial Strategy published in May referred to resource spending on the NHS increasing by £2 billion over the course of this Parliament (to 2021-22). The Medium Term Health and Social Care Financial Framework refers to an increase of £1.5bn in spending on frontline NHS Boards over the period 2016-17 to 2021-22. Although this relates to a narrower definition of health spending it is unclear to us how this reflects the planned £2bn additional health spending. We ask the Scottish Government to clarify and specify the issue and also to confirm the extent to which the figure fully includes the anticipated Barnett consequentials.
The Framework also refers to funding for primary care increasing to 11% of the frontline NHS budget by 2021/22. We request confirmation of the actual amount this will equate to and the current amount and percentage of the NHS frontline budget which is spent on primary care.
The Financial Framework states that future demand projections for health have been based on an annual growth rate of 3.5% in the cash budget. If demand pressures are to be met within this annual uplift, then substantial savings will need to be found, as outlined in the document. We ask the Scottish Government what plans it has for future funding should these savings plans prove unachievable.
NHS board brokerage
The issue of NHS boards requiring brokerage is one that the Committee has explored in its evidence sessions with NHS boards.
The information earlier provided by the Scottish Government highlights that, as of December 2017, NHS boards had overspent by £76.8m. Overspends by NHS territorial boards (£80.8m) were partially offset by underspends (£4m) by special boards. As at December 2017, the largest projected overspends were in:
NHS Greater Glasgow and Clyde (£25.3m)
NHS Ayrshire and Arran (£18.5m)
NHS Highland (£12.2m)
NHS Tayside (£6.7m)
In a session with the Committee on 8 May 2018, NHS Greater Glasgow and Clyde stated the overspend identified in December 2017 had been managed so that financial balance had been achieved by the year end.i
A letter from the Director-General to the Public Audit and Post-Legislative Scrutiny Committee dated 21 May 2018 confirmed that brokerage requests for 2017-18 had been approved for NHS Ayrshire and Arran (£23m) NHS Highland (£15m) and NHS Tayside (£12.7m).ii
We note that each of these NHS board overspends increased quite significantly in the last three months of the financial year.
The same letter confirmed that on-going brokerage was anticipated for these three boards, as well as for NHS Borders in 2018-19—
“The financial forecast for 2018/19 is informed by the Board’s annual Operational Plans. These plans indicate that the three Boards outlined above; NHS Ayrshire and Arran, NHS Tayside and NHS Highland will require a two to three year timeframe to return to financial balance and the Scottish Government continues to engage with these Boards to fully understand the parameters of their financial position in-year. In addition to these three Boards, NHS Borders has also indicated a forecast deficit position in 2018/19. The initial estimated request for financial brokerage for each of these Boards is as follows: NHS Tayside (£20 million); NHS Ayrshire and Arran (£20 million); NHS Highland (£19 million); and NHS Borders (£13.2 million). All other Boards have assumed a breakeven position, recognising that there is a further level of saving that will require to be identified in-year.”ii
The issue of brokerage was explored in the Committee’s evidence session with the Scottish Government in June 2018. Christine McLaughlin, Director of Health Finance explained that the expectation was that, for those boards that were in deficit, recovery would take more than one year. She also suggested that the brokerage required for each board was likely to fluctuate during the year. She detailed the reasons for this “We might expect boards to be more prudent at the beginning of the year and then to make improvements through the year”.iv
We note Christine McLaughlin’s suggestion that boards may require less money by the financial year end does not match with the actuality of brokerage requests in 2017-18, all of which followed the opposite trajectory.
The Director-General was asked whether the need for brokerage reflected temporary problems or structural deficits that required fundamental action. In response he told the Committee—
“I do not have evidence to show that there is an underlying structural deficit in boards. One of the bases on which we provide brokerage is that the board has a plan to recover sustainable financial balance. We cannot really have one without the other”.iv
Efficiency savings
An analysis of the data available shows that when compared with the anticipated position on efficiency savings that boards had set out in their Local Delivery Plans, the majority of boards had not made as much progress as had been expected in achieving efficiency savings. Overall, boards had achieved £20.1m less in efficiency savings than had been expected to be achieved by December 2017. Again, this was largely due to a weaker performance from the territorial boards. Special boards had collectively achieved £1.9m more in efficiency savings than they had forecast at December 2017. By contrast, efficiency savings achieved by territorial boards were £22m less than had been anticipated.
This overall position reflects a mixed performance across boards, with half of territorial boards under-achieving against their efficiency savings targets by December 2017 and the other half over-achieving. NHS Greater Glasgow and Clyde was furthest from its efficiency savings target, with savings £22.4m lower than forecast at December 2017. By the current financial year end, NHS Greater Glasgow and Clyde is expecting efficiency savings to be £44m lower than planned.
We explored the position of NHS Greater Glasgow and Clyde with the Director-General. He told the Committee that having discussed the NHS board’s position with the Chair “I think that NHS Greater Glasgow and Clyde will find efficiencies in the course of the year that will defray the £44 million to a point at which it will come into financial balance”.i
Christine McLaughlin emphasised it was important the process of setting a budget was not viewed as something done for a 12- month period but as a continual process. In relation to NHS Greater Glasgow and Clyde she explained that consideration should be given to whether the level of savings that a board had achieved was very different from the level it achieved in previous years. She highlighted that NHS Greater Glasgow and Clyde along with NHS Lothian was achieving savings not dissimilar to previous years.
She also told the Committee efficiency savings should not be considered in isolation but looked at within the context of transformational change plans as the answer lay in the reform of services in addition to achieving a core level of efficiency savings—
“When it comes to the timeframe, the transformational change savings tend to have a ‘longer tail’, whereas boards will expect to achieve a minimum level of efficiency savings of 3% in-year. It is necessary to look at the total picture”.i
We note that the Financial Framework outlines spending plans that depend on substantial levels of savings being achieved. We ask the Scottish Government to comment on how realistic this aim is, given the challenges that Boards already face in meeting efficiency saving targets.
Change in approach to outstanding brokerage expenditure
The Cabinet Secretary told the Scottish Parliament on 4 October 2018 that as part of the new deal for NHS boards, the Scottish Government would not seek to recover their outstanding brokerage (the expenditure that they had incurred over the past five years that has been above their budget). She added—
“However, at the end of three years, the territorial boards have to break even. We cannot continue with a situation in which boards have significant overspends on their budgets, albeit that those spends were made on patient care.”
“I want the lessons learned from boards in which financial management and quality of patient care are being finely balanced but are being managed to be transferred to colleague boards, and my officials will help them to do that. That is actively happening right now.”i
In response to questions the Cabinet Secretary indicated that the Scottish Government’s current estimate of the cost of brokerage for the past five years was around £150 million. Territorial boards would start with a “clean slate” from 2019-20. The Cabinet Secretary also stated—
“In the meantime, boards will continue to work to reduce their anticipated level of brokerage. That level is reducing significantly in many boards as they refine and finalise their reform and service delivery plans.”i
We note that the brokerage requests from NHS boards for 2017-18 showed a significant increase in the finances required in the last three months of the financial year. We ask the Scottish Government why this increase was not anticipated and what steps have been put in place to improve the accuracy of financial monitoring.
The Cabinet Secretary has estimated brokerage for NHS territorial boards for the last five years as £150m. We ask the Scottish Government to confirm how it has arrived at this figure broken down to NHS board level. In response to this report we ask the Scottish Government where the funding to ‘write off’ the brokerage payments is coming from.
We ask the Scottish Government how NHS boards will be incentivised to reduce their need for brokerage and meet efficiency savings before the financial year end given the commitment that all outstanding brokerage expenditure will be written off.
We note that the money to write off outstanding brokerage expenditure has as yet not been approved by the Scottish Parliament. To allow Parliament to consider this proposal would the Cabinet Secretary indicate her proposed absolute maximum and what measures are in place to ensure the announced open-ended guarantee is not subject to any misuse by these or other NHS boards?
Regional planning
The National Health and Social Care Delivery Plan committed to putting in place new arrangements for the regional planning of some services. In 2017, an existing NHS Chief Executive was appointed to each of the three regional boards (West, East and North). Each of the three regions was asked to gather expertise and write a regional delivery plan for submission to the Delivery Board in 2017.
At the April 2018 Conveners’ Group the First Minister was asked about regionalisation and the implications for accountability. She said—
“The building block of regionalisation is still individual health boards, and accountability matters with regionalisation just as it does with services that are provided within individual health boards. However, we are thinking increasingly about whether changes are required.”i
Our NHS Governance inquiry considered the operation of regional planning boards and the way in which these interact with NHS boards and integration authorities. We received examples of how accountability may be blurred with NHS boards being held responsible for performance against the cancer waiting time targets, despite cancer services increasingly being planned and delivered on a regional basis.
Our inquiry report concluded lines of accountability for integration authorities and regional boards are not always clear. We recommended immediate attention was given to Audit Scotland’s call for the Health and Social Care Delivery Plan to simplify and make clear the lines of accountability and decision-making between the Health and Social Care Delivery Plan Programme Board and major work programme delivery oversight groups, regional boards, NHS boards and integration authorities. ii
We returned to these issues in our evidence session with the Director-General who told the Committee that the regional plans were in development and would be available once the financial framework was published. iii
He emphasised that regionalisation was about both the planning and delivery process. Shirley Rogers, Director of Health Workforce and Strategic Change detailed that the strategy for the delivery of health and social care had three key elements – national, regional and local. She explained that the focus was on considering service delivery from the patient perspective and ensuring the delivery plan methodology emphasised the local delivery of services where it made most sense to do so. iii
She told the Committee—
“although there is governance around that regional structure, regions are quite porous structures. They have boundaries, and we are not necessarily going to make somebody who lives on the outer edge of a region travel a long distance when they could skip over the boundary.”iii
We asked the Director-General how he anticipated lines of accountability developing at a regional level. He acknowledged there was a possibility in the future that there might need to be an element of regional accountability. However, he emphasised the current focus was on ensuring regional delivery was in place and then consideration would be given to whether this required changes to accountability structures. He stated “Each of the chief executives remains an accountable officer and there is no immediate plan to change that”.iii
Regionalisation will be an important aspect of future financial planning. We are therefore concerned that although the three regional boards were asked to provide a delivery plan in 2017 they are still to be published. We request this lack of transparency be addressed and the delivery plan be published by the Scottish Government in advance of the budget.
We have received examples where there is confusion regarding where responsibility as well as accountability for delivery of some services lies. Whilst recognising the ‘organic’ approach taken to date in the development of regionalisation we believe this is presenting challenges that need to be addressed by making lines of accountability and decision-making clearer and more transparent.
We believe there are currently issues around accountability of services. Evidence we received from the Scottish Government suggested that changes to accountability was something for future consideration. However, we have received examples of issues around accountability that are already occurring as a result of service delivery at a regional level. We would welcome the Scottish Government’s comments on this and believe steps should be taken now to address issues around accountability structures.
Integration Authorities
Leadership
An overarching theme raised during our pre-budget scrutiny has been the importance of relationships and leadership in determining progress towards integration.
Judith Proctor of Edinburgh Health and Social Care Partnership told the Committee—
“All the guidance and the legislation that we have in place that drives us to work in a certain way is necessary, but more important than that are the relationships and willingness for integration to work and for the budget-setting process to continue in a positive, proactive way.” i
Emphasis was placed by several witnesses on the importance of ensuring effective relationships at a leadership level. Robert McCulloch-Graham of Scottish Borders Health and Social Care Partnership told the Committee— "[…] if the relationships at the senior level between the three main organisations are not working, the system will just not work.”i
He suggested that the legislation underpinning integration may be “overcomplicated” and placed too much reliance on the importance of the relationships between individuals in the local authority, health board and integration authority.
Pam Gowans of Moray Health and Social Care Partnership told us she believed that relationships were the key to success for integration. She discussed that they strive to maintain relationships between the key partners involved in integration as she considered it to be important to try to resolve issues together. She suggested, however, there may be a need for integration authorities to show more authority— “[…] we need to ask whether we are asserting the authority and the power that we have at the level that we could be. As we move forward, we need to do so confidently.”i
This was an issue we highlighted in our Pre-budget report 2017 in which we called for clear leadership to be provided by the Chief Officers of each IA in line with direction provided by the Scottish Government to drive this change forward and ultimately ensure its delivery.iv
The importance of relationships and leadership in ensuring the delivery of integration are also issues Audit Scotland has raised in its reports on integration. Most recently the exploration of the leadership role of IA Chief Officers has been considered by the King’s Fund in its Report “Leading across health and social care in Scotland: Learning from chief officers’ experiences, planning next steps”. v
The King's Fund report highlights previous work it has conducted on lessons to be learned for the English system from other UK countries’ approach to integration. Its conclusion on the system in operation in Scotland reflects the views expressed to the Committee by integration authorities that relationships are a key area requiring development.
The Kings Fund stated—
“it was noticeable that Scotland had made progress in all the policy and systems issues identified as important (and yet, unsurprisingly the aspects that cannot be legislated for, notably developing relationships and embedding cultural change, continued to require work).”vi
The King’s Fund report suggests six areas for action for IA Chief Officers and the Scottish Government’s policy leads for integration of health and social care. This includes strengthening the work and role of the Chief Officers’ network including ensuring provision for individual and collective leadership development.v
Achieving 'true' integration
The role of leadership and relationships in delivery of integration was raised within the context of concerns that there continues to be a perception of ‘health’ and ‘social care’ funding as two distinct streams.
We stated in our Pre-budget report 2017 that, two years into the operation of integration authorities, we were concerned funding for integration authorities was still failing to ‘lose its identity’ as the legislation on integration intended.i
The evidence we received during the course of our pre-budget scrutiny this year suggested these concerns remained. Written evidence from North Lanarkshire Health and Social Care Partnership stated—
“The current system encourages the funding to work through both the local authority ledger and the health board ledger. The funding does not therefore lose its identity as was intended by the legislation.”ii
Robert McCulloch-Graham of Scottish Borders Health and Social Care Partnership suggested that relationships and conversations between partners were easier in situations where it was new money as they were able to ‘pump-prime’. He explained in these situations disinvestment in one area was not required to bring investment in another and this resulted in an increased level of debate between stakeholders as there was a greater degree of freedom regarding how the funding was to be invested.iii
Robert McCulloch-Graham also offered further insights into the conversations that were required between the key partners. His evidence suggested the loss of identity of funding between health and social care funding was not yet in evidence—
“I think that all the parties are conflicted in deciding on the budget. There are allocations from councils and allocations from the NHS, and then there is a smattering of free money, if you like, in between. There are concerns in the NHS and council bodies about the value that they get on the back of the money that has gone in. There is bound to be a good thing in that regard, but a difficult negotiation has to take place at the IJB on how we are actually going to make the spend.” iii
His comments also raised questions regarding the authority of IAs in such negotiations he told us—
"There are a number of masters over the funding, and trying to keep everybody on the same page is a difficult, challenging and enjoyable job for us all. There is more that we could do to simplify the money with regard to how the budgets are delegated to the IJBs.”iii
In oral evidence Janice Hewitt of North Lanarkshire Health and Social Care Partnership stated that health and social care integration will be successful “only when you cannot see the lines between budgets, between workforces and between organisations, and there is strategic planning across the whole system”. iii
Direct funding
We returned to the issue of direct funding (which we considered in our Pre-budget report 2017) as one potential solution to the concerns that funding was failing to lose its identity.
Several IAs commented that integration worked most effectively when money came directly to them without a “health” or “local authority” label. Eddie Fraser of East Ayrshire Health and Social Care Partnership said— “We see the resources working best when they have come to us jointly”.i
Judith Proctor of Edinburgh Health and Social Care Partnerships, expressed views on moving to direct funding and offered insights into the importance of relationships in delivering progress towards integration. She told us she was hesitant about adopting a direct funding approach. She suggested there were challenges in how the IA budget process operated. However, she explained the current approach meant challenging conversations had to be had between IAs and their partners. She was unsure if the same engagement and discussion would be achieved if these conversations were not required because there was a different approach to budget allocations.i
Scottish Government view
We explored with the Scottish Government issues regarding leadership and the achievement of ‘true’ integration and direct funding.
The Director-General told us—“I would not expect integration to be perfect after two years”. He said there was evidence of it working well in some areas with examples of staff who are delivering front-line services being identified not as being part of the NHS or local government but by the service they are providing.i
He spoke positively of the “real determination” of Chief Officers and Chief Executives to bring together the two cultures of the health service and local government for the benefit of patient care. i
The Director-General also told us work was being done to support the leadership that is provided by chief officers. He later added—
“We are doing all that we can to ensure that those senior posts have the right amount of power, authority, accountability and responsibility, consistent with what we are asking them to do.”i
We asked the Director-General whether the fact that IA Chief Officers are associated with either a health board or local authority led to a conflict of interest. In response he told us—
“there certainly should not be conflicts of interests, because the appointments are deliberately designed as joint appointments, in that the health board and the local authority have equal say.”i
His response went on to suggest that he considered the right processes to be in place, but that progress still needed to be made to ensure effective delivery.
In response to questions regarding the use of direct funding, the Director-General told us that the current approach placed integration at the core of the delivery of health and care services and what lay behind the legislative approach being taken was “the genuine and persistent ambition to ensure that health, local government and third sector partners have joint ownership of integration”.i
Christine McLaughlin Director of Health Finance told us “The fact that the resources come in from parent bodies should not, in itself, be the barrier". She did suggest however that there may be ways to make the approach easier “we could, for example, take away some of the complexity about individual allocations for various things and how they flow through.”i
For the integration of health and social care to deliver transformational change in services requires a fundamental change in the relationship between local authorities and health boards. Integration authorities are tasked with leading and driving this change and ensuring it is embedded in the culture and approach being taken.
The message we have received from the Scottish Government is that it considers the legislation underpinning integration to be clear regarding lines of accountability and IA Chief Officers should feel empowered to provide the clear leadership direction and authority that is required in this role.
However, three years [we include in this period the 12 months for set up] into integration, a number of integration authorities do not appear to be exerting that challenge function and ultimately their authority and control over the budget is being dictated by individual partners. This situation cannot be allowed to persist and we would welcome the views of the Scottish Government on when they consider it appropriate for the changes agreed by Parliament, when passing the legislation, to be delivered.
We have explored in our pre-budget scrutiny whether there are further steps that could be taken to support integration authorities. This has included addressing concerns that IA Chief Officers (and Finance Officers) are associated with either a health board or a local authority leading to conflicts of interest. Also whether direct funding may be an appropriate change to allocating funding. However, to date, the Scottish Government has emphasised that it is about supporting and facilitating the effective operation of the current arrangements, not making changes to lines of accountability or mechanism for budget allocation.
If in response to this report the Scottish Government remains firm on this view we believe it must then take further action to support IAs in their relationships with local authorities and health boards. We do not believe at this stage we are seeing evidence that IA leadership across all 31 IAs is equipped to deliver this change in relationships and ultimately deliver the transformational change in health and social care that is required. We ask the Scottish Government in response to this report to detail the steps it is taking to measure the quality of leadership at IA level.
We note the King’s Fund call for individual and collective leadership development at a Chief Officers level. We ask the Scottish Government since publication of the King’s Fund report what steps it has taken to support this work. We ask the Scottish Government how it evaluates leadership within the IAs and, where concerns regarding leadership and relationship are found, what steps are taken to improve performance. We believe further steps need to be taken to ensure IA leadership is sufficiently robust in setting out requirements and providing clear direction. To rephrase the quote from Robert McCulloch-Graham there can only be one master; it is the responsibility of the IAs to lead on allocation of funding in areas delegated to the IA.
The King’s Fund suggests six areas for action for IA Chief Officers and the Scottish Government’s policy leads for integration of health and social care. We ask the Scottish Government to provide comments on each of these recommendations and information on how they are being taken forward.
Set aside budgets
How set aside budgets should operate
The set aside budget is the IAs share of the budgets for delegated acute services provided by large hospitals on behalf of the IA. Set aside only applies to “large hospitals” i.e. hospitals providing care to patients from more than one partnership [set aside only applies to the 30 integration joint boards and is not relevant to the lead agency model in Highland, as hospital services are not delegated].
An IA determines how much it expects will be required for delegated acute services. The IA then decides whether it will include this amount in the payment that the NHS boards make to the IA, or whether it will exclude this amount from the NHS board payment to the IA, in which case this amount is “set aside” and retained by the NHS board. All but two IAs (Dumfries and Galloway and Argyll and Bute) have chosen to allow the NHS board to retain the “set aside” amount (although this budget, in theory at least, remains available for direction by the IA we have not been able to identify any instances where the theory has worked in practice). For those IAs with a set aside budget, it represents between 6% and 15% of the total IA budget. The variance will, in part, reflect differing scopes of delegated hospital services. In 2017-18, set aside budgets accounted for a total of over £800m within IA budgets.
If expenditure on delegated acute services turns out to be more than the amount anticipated in the budget, the IA will need to fund this additional expenditure from elsewhere in its budget. On the other hand, if expenditure turns out to be lower than expected (for example, if unplanned admissions are reduced), then the IA should – in principle – have access to the funds realised and be able to direct the additional funds to other areas of activity, such as social care.
So, in theory – as shown in the diagram below – Integrated Joint Boards (IJBs) should exercise control over the set aside budget. (Note the term IJB is used here, as set aside only applies in the IJB model, not the lead agency model.)
Set aside budget how it should work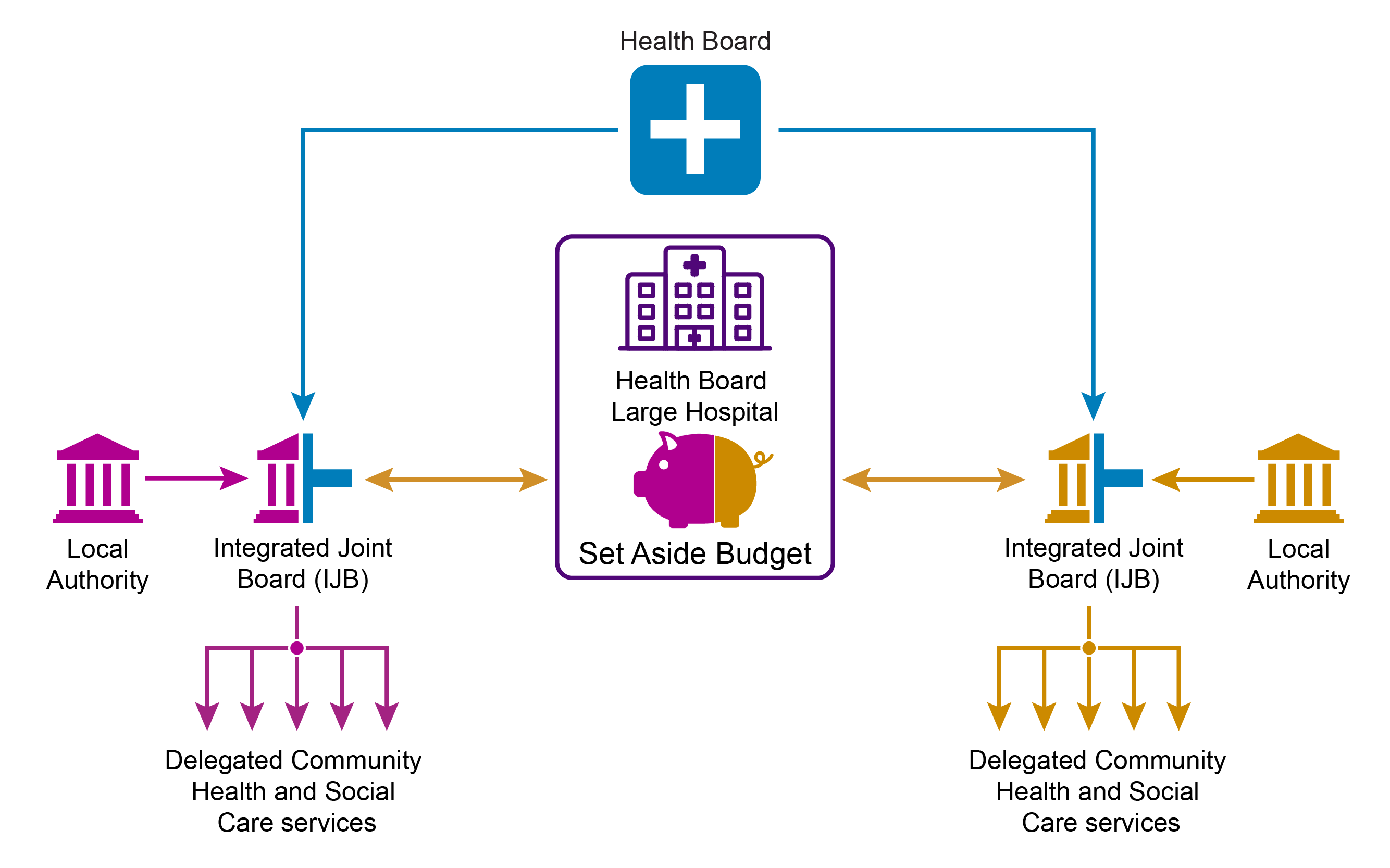
However, in practice, evidence given to the Committee suggests that the IJBs are not effectively controlling the set aside budget and these funds remain under the control of the health board. This is highlighted in the diagram below, which shows how the set aside budget is used to deliver delegated services, but is not effectively controlled by the IJB.
Set aside budget how it works in practice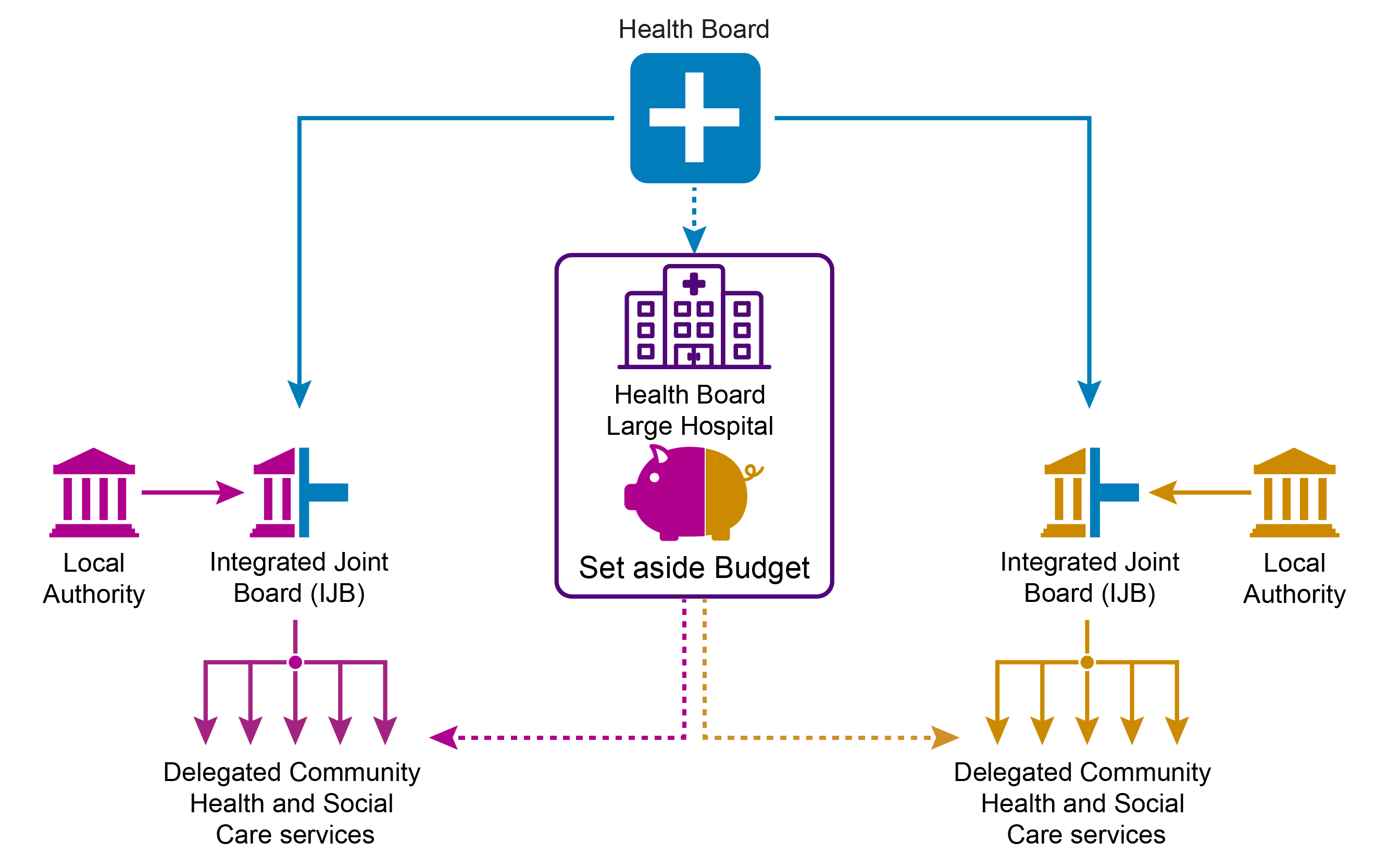
The current operation of set aside budgets
According to the 2017-18 information provided by the Scottish Government, 10 IAs had an overspend on their set aside budgets i.e. expenditure on acute hospital services was more than anticipated. Those with overspends on their set aside budgets included Edinburgh (£2.7m overspend (2.9%) on its set aside budget) and Scottish Borders (£3.5m overspend (16.8%) on its set aside budget).
In the case of Scottish Borders, this will be met by increased funding from NHS Borders. Two IAs have reported underspends on their set aside budgets.
Our Pre-budget report 2017 concluded that IAs were facing problems with respect to set aside budgets and that the current operation of set aside budgets presented a barrier to the success of integration. In response to the report the Scottish Government indicated that the Director of Health Finance at the Scottish Government would be convening a group (Integration Finance Development Group) to undertake work in this area, looking at where partnerships were experiencing common challenges.i
We returned to these issues in our pre-budget scrutiny this year.
Integration authorities' view
In written evidence several of the IAs referred to the statutory guidance relating to set aside budgets. Moray Health and Social Care Partnership said the guidance “aspires to be a commissioning type relationship for set aside services with the IA having strategic planning responsibilities over these services”.i
We received limited examples of set aside budgets being redirected away from acute services. North Lanarkshire Health and Social Care Partnership did provide one example “the transfer of the Community Assessment and Rehabilitation Service from acute sector to localities is an example of a shift in resources of £1.4m from the set aside budget to the directly managed community budgets”.ii
The majority of evidence we received reiterated the concerns we had heard during last year’s pre-budget scrutiny that the set aside budget is not operating as intended.
Several witnesses suggested that the budget was treated as being under the control of the NHS board, rather than the IA, with the result that it was difficult for IAs to use the money to shift from acute hospital care to community-based and preventative services.iii
Pam Gowans of Moray Health and Social Care Partnership told us that if the IA achieved reductions in unscheduled care to a particular level this would technically mean the IA had the money to invest in the community setting. However, she stated that it was to date “a notional budget”.iii
She explained— “It is a budget with potential, but it is not any size of actual budget that we are able to invest in making change”.v
Eddie Fraser of East Ayrshire Health and Social Care Partnership expressed a similar view “In many areas the set aside figure is just a statistic […] In the first few years of operation, it has been a reporting position, rather than a leverage position”.iii
Scottish Government views
We explored in our evidence session with senior Scottish Government officials the concerns that had been raised by IAs regarding the operation of the set aside budget.
The Director-General acknowledged that there was a difference between the theory and the actual operation of the set aside budget-
“there is a set of principles around how the setaside budget should work, but within health boards, local authorities and the integration partnerships there are genuinely contested views about how they should work in practice.”i
He highlighted the discussion he had convened with stakeholders to “work through” these issues. He told us the Ministerial Steering Group jointly chaired by the Cabinet Secretary for Health and Sport and the Health Spokesperson in COSLA was showing an interest in the matter too.i
The Director-General also highlighted there was a complexity faced in releasing money through the set aside budget. He explained that whilst an IA may reduce the demand for hospital care through its activities this may not result in releasing finances. He detailed that it may be only part of a service on a ward that is no longer required. It was difficult to release an efficiency saving if only a part of the service had been removed as the ward would still need to be funded.i
Christine McLaughlin, Director of Health Finance emphasised that for the set aside budget to operate effectively the acute component of hospital care needed to be included in IA plans for services. “It has to be about more than just calculating a budget; it has to be something that features in their plans”. She added “The flow of money should be based on the service delivery plans; it should not be the other way around”.i She highlighted that good progress with this approach had been made in Aberdeen City IA.
Alison Taylor, Head of Integration Division described the set aside budget as a “mechanism to shifting the balance of care”. She explained the merits of the set aside budget being part of IAs budgetary control—
“One of the challenges that we are trying to address now is the potentially avoidable use of institutional care in hospitals and care homes for frail older people and others, and we recognised that the only way that the new partnerships could get a grip of transforming that kind of care would be if they had some authority over aspects of it.”i
The Director-General in further correspondence following the evidence session emphasised that making a success of the set aside arrangements required new kinds of working arrangements in the local system. The Director-General detailed the statutory guidance which sets out six main recommendations to encourage this.vi
It is clear that 12 months on from when we last raised concerns with the operation of set aside budgets, there remains a disconnect between how the set aside budget should operate in principle compared with how it is operating in practice.
The Scottish Government described the set aside budget as a mechanism for shifting the balance of care, however this mechanism is not being utilised effectively across all IAs. Some IAs describe the budget as a “notional” budget rather than an actual budget that they can use to affect change. Three years into the operation of IAs we do not consider this position to be acceptable.
The statutory guidance to support the new working arrangements and the Scottish Government’s Integration Finance Development Group to date have not delivered results in ensuring the set aside budget is working effectively in all IAs.
Progress needs to be made in the funding allocated to delegated acute services. We recommend the Scottish Government consider placing a requirement that NHS boards delegate their acute hospital services budget to the IA rather than having the option of the NHS board retaining this budget. We believe this approach would assist in addressing the impasse in the operation of these budgets in some IAs at present.
We note the views expressed by the Director-General that there can be challenges to release an efficiency saving if only a part of the service, for example a ward, is no longer required, as the ward still needs to be funded. If acute services budgets are not delegated to IAs we ask the Scottish Government how the situation where there is a partial reduction in a service is not sufficient to release funds can be rectified.
The Scottish Government emphasised that the acute component of hospital care should be built into service delivery plans. These plans should then direct how the money flows – in turn assisting with how the set aside budget operates. The Scottish Government highlighted that Aberdeen City IA as a good example of this. We ask the Scottish Government why Aberdeen City has been able to deliver this approach whilst other IAs have not? What barriers are other IAs facing which have prevented them from successfully implementing this approach and how can these be overcome?
We believe leadership is an important component in determining the effectiveness of the operation of the set aside budget. The Director-General referred to “contested views” between health boards, local authorities and IAs about how the set aside budget should work. The Scottish Government spoke of set aside budgets as giving IAs some ‘authority’ over aspects of acute hospital care. We believe that the current operation of the set aside budgets in IAs suggests they are not exerting this authority with regard to the operation of the set aside budget. We ask the Scottish Government how this can be rectified in the coming financial year.
We also request information on the target that has been established for the set aside budget impacting on the shift in the balance of care. We wish to monitor progress towards delivery of this target and request this information is provided as part of the overall figures on progress towards delivery of the shift in the balance of care.
We are concerned that IAs are not providing the clear leadership, direction and authority required in these situations. We ask what further actions the Scottish Government will take to ensure IAs Chief Officers ‘lead’ and use the tools they have at their disposal to ensure the effective operation of the set aside budget.
Linkages between budgets and outcomes
The activities of IAs are expected to contribute towards nine ‘national health and wellbeing outcomes’. In addition, IAs are required to report budgets against these outcomes.
In our budget report of 2016 we first raised concerns over the IAs awareness of these reporting requirements and the apparent lack of progress towards publishing budget information of this nature.i
Our evidence session with integration authorities highlighted continued challenges with IAs adopting this approach.
Robert McCulloch-Graham of Scottish Borders Health and Social Care Partnership commented that many activities would be working towards a range of different outcomes. He concluded—
“It is important that we are scrutinised against the outcomes and demonstrate how we are meeting and working towards them. However, allocating specific funding to a specific outcome would not be that helpful.”ii
We note that Robert McCulloch-Graham made a similar point when he gave evidence to us in October 2016 when he was the Chief Officer at Edinburgh Health and Social Care Partnership.ii
We explored with the Scottish Government the support it was currently providing to integration authorities to help them to develop their reporting of budgets against outcomes. The Director-General told us—
“We have been keen to help integration partnerships to have the necessary underpinning data to support their analysis both of what they should do, including the areas that they should prioritise, and of the outcomes that they achieve.”iv
He referred to the NHS National Services Scotland’s local intelligence support teams which were providing IAs with access to local data. He detailed that this data could identify the specific areas where patients use the most health and social care funding. It also enabled an assessment of trends in service use by patients to determine if shifts were being made away from the acute sector to provision of services nearer to home. iv
Alison Taylor, Head of Integration Division told us the Ministerial Strategic Group was receiving quarterly updates from IAs demonstrating the extent of progress towards improvements in six priority areas including unscheduled occupied bed use and the balance of spend on palliative and end-of-life care. She detailed this data was beginning to illustrate to the Ministerial Group that there was variation between IAs both in how services are used and in the ambition of projections for future usage.iv
In the context of determining outcomes Scottish Government officials also discussed the importance of ensuring outcomes captured qualitative information as well as quantitative. The Director-General told us—
“Outcomes are not only objective; they are also subjective. In other words, whether the patient felt that the quality of care was good it just as important to me as whether we can, by some measurement, say that the quality of care was what it should have been.”iv
Christine McLaughlin told us that it was starting to look at high-level expenditure but there were challenges to producing this information. She highlighted the difficulties in cases like mental health spend where expenditure was across both primary care and social care.
She explained that the Scottish Government’s current costing information systems needed investment to ensure the information was meaningful and provided on a real-time basis for IAs. Whilst she highlighted the Scottish Government had started to invest in such systems to look at national outcomes in relation to financial expenditure she told the Committee “we do not yet have a comprehensive programme budgeting approach across either health or social care”.iv
Targets
Another issue raised by integration authorities in the context of outcomes was that individual targets could divert expenditure. Several IAs referred to delayed discharge as being an area of high focus which could distract from delivery of other outcomes.
Janice Hewitt of North Lanarkshire Health and Social Care Partnership highlighted the implications of targets for budget-setting, noting that savings were most likely to be found from areas of activity that did not have specific targets. She said—
“Attaching a target with an expectation of delivery drives a set of behaviours. Only 46 per cent of my budget can be challenged for savings; the rest is fixed. An incredible amount of money is set, from which I cannot take anything.”i
She gave the example of care packages, which could not be removed, later acknowledging these could be remodelled over the longer-term. i
Judith Proctor of Edinburgh Health and Social Care Partnership also cited the example of funding committed to GP services which is largely fixed.i
We explored with the Scottish Government officials whether targets were distorting behaviour and if so whether this was an area of concern. Paul Gray told the Committee—
“We are very alert to the fact that, in certain contexts, targets can create perverse incentives, but I always take the view that the public are entitled to know what to expect from a health and care system."iv
He stated in relation to the health and social care objectives they were set out in legislation at a sufficiently high level to avoid the risk of perverse incentives.
He detailed to us that targets such as the A&E waiting time were clinically appropriate targets for driving behaviour and were relevant to integration as what happened in the community and social care setting impacted on the target.iv
Alison Taylor told us that a lot of integration authorities had added their own objectives, and were not working to the priority areas the Ministerial Strategic Group was requesting data from IAs on. She detailed that some IAs had worked with their local communities to develop objectives and ambitions appropriate to their local system.iv
Whilst there is a statutory requirement for IAs to report on how they have used their resources to achieve the health and wellbeing outcomes, it is unacceptable this is not being done and the Scottish Government and Parliament does not know how some £8billion is being spent.
We note some IAs continue to raise the same concerns regarding the complexity of linking budgets to outcomes and the value of adopting such an approach.
There is a statutory obligation for IAs to provide this information yet limited progress has been made to date. For IAs to embrace this approach there must be value in it. We consider it unacceptable IAs are taking allocation and investment decisions without assessing, or even possessing the ability to assess the relationship between the effectiveness of spending on outcomes.
We have previously called for direction to be given by the Scottish Government to provide IAs with clear parameters within which to measure and quantify IA budgets against specific outcomes. We now expect such measurement to be provided.
We welcome the comments from the Scottish Government which suggest some steps are being taken to look at national outcomes in relation to financial expenditure. We also welcome the Scottish Government’s comments which recognise the importance of ensuring this information is meaningful and provided on a real-time basis for IAs.
However, we believe it remains unclear what priority this work is being given by the Scottish Government; how long a system linking spend with outcomes will take to develop and implement and, ultimately, at what stage the Scottish Government will be able to evaluate IAs performance against its own priorities. We expect this issue should be a key priority and Parliament should no longer be put in the position of approving allocations which are not measurable.
The Scottish Government must, in advance of the publication of the budget, provide assurance that developing budget information against outcomes is a top priority, advise when this information will be available and provide further information on the work that is being undertaken with the deadlines set for delivery.
In relation to data that is currently available we note the comments from the Scottish Government that data they are starting to gather on IAs performance in priority areas is not only demonstrating a variation in performance but also in ambition for change between different IAs. Given this, we expect the Scottish Government to take steps to ensure this variation in performance and ambition is addressed.
We note the concerns raised by some IAs that a large proportion of IA budgets are ‘fixed' at least in the short term. We ask the Scottish Government if only a limited proportion of the budget is ‘free’ to be directed by IAs how it can be assured this is not hampering innovation in the delivery of services. It is impossible to track spend on innovation and there is no way of evaluating its overall success. Where that does happen we are unaware of any system which rolls out successful changes. We request further information on how information on innovated approaches is being collected and disseminated.
The impact of targets on behaviour is an issue we have explored in previous budget reports and most recently with Sir Harry Burns in the context of his review of Targets and Indicators in Health and Social Care in Scotland.
We recognise and support the comments we received in our pre-budget evidence sessions regarding ensuring outcomes capture both quantitative and qualitative data. As we stated in our NHS Governance report, targets should be aligned with quality of care and outcomes. We are disappointed with the lack of progress that appears to have been made in the further development of a suite of health and care targets following the findings and recommendations in Sir Harry Burns review. In advance of the publication of the Scottish Government budget we request a timetable from the Scottish Government for when the new targets will be in operation.
Shifting the balance of care
The integration of health and social care is intended to bring about a shift in the balance of care. The Scottish Government’s stated aim is that, by the end of this Parliament, less than 50% of spending will take place in the hospital sector.
The Scottish Government estimates that, on the basis of 2016-17 data, 49.1% of frontline NHS spending is on primary and community health services. The IAs are considered to be an important vehicle for making progress in this area.
We have previously highlighted limited evidence of any discernible shift in resources from the acute to the community sector. We requested in our survey to all IAs how they split their budget between broad service areas.
The responses from IAs show there have been some modest shifts in budget allocations over the three years of operation of the IAs. Family health and prescribing and social care budgets have reduced as a proportion of the total budget, while there have been modest increases in the shares of IA budgets accounted for by both hospital and community healthcare. [2018-19 data are based on only 26 IAs as information was not provided by four IAs]
IA budgets by service area 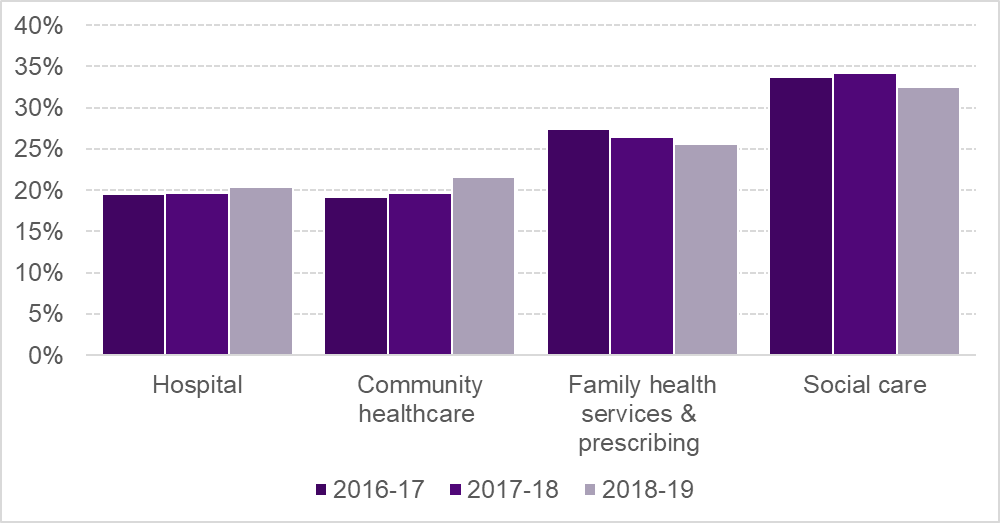
While these figures do suggest progress in shifting the budgets towards community healthcare, this appears to be at the expense of family health services/prescribing and social care, rather than resulting from a reduction in hospital expenditure, which is showing an increased proportion of spend.
We explored these findings with IAs. They told the Committee that in the context of increasing pressure on acute services, it would be surprising to see a marked shift away from hospital services, but that integration had succeeded in preventing a further shift of resources towards the acute sector.
Eddie Fraser of East Ayrshire Health and Social Care Partnership said real progress had been made but noted—
“The demand on acute services would be much greater if we were not doing what we are doing. We do not want to set up a false conflict between community and acute services: both sides are really busy and are, on the whole, doing appropriate things.”i
Asked whether IAs were ‘chasing their tails’, Robert McCullloch-Graham of Scottish Borders Health and Social Care Partnership said—
“We will never catch the tail, because the pressure is on both sides of the system. Without the work of the partnerships, I think that the hospitals would have fallen over by now. The work that we are doing to shift people in the community, where they want to be cared for, is the right thing to do.”i
Scottish Government view
The Director-General told the Committee that real progress was being made towards the Scottish Government aim of 50% of spending taking place in the Community Health Service. He told the Committee that the figure was over 49%.i
We explored with the Scottish Government whether the target was ambitious enough given the progress that had already been made. The Director-General told the Committee— “I would have no difficulty in discussing whether the target ought to be extended.” i
Dr Catherine Calderwood, Chief Medical Officer, was also supportive of consideration being given to reviewing the target as she highlighted there was scope to increase the capacity in services such as ‘hospital at home’. She told the Committee the service was preferred by patients and that it reduced prescribing costs and readmission to acute hospital.i
Christine McLaughlin told the Committee that the focus on shifting the balance of care was on achieving “differential growth rather than seeing overall reductions.” She emphasised that to achieve a 50% spend in community health service required not only a shift in resource but making efficiencies in spend where possible. She highlighted prescribing as an area where efficiencies had been made resulting in the avoidance of an increase in primary care spending. i
The Scottish Government Medium Term Health and Social Care Financial Framework states that although there has been a growth on average of 9.5% year on year in community services it does not yet represent a shift in the overall balance of care. This is because expenditure on hospital services has also been growing significantly, with high rates of growth in outpatient (5.5%), Accident and Emergency (4.8%) and hospital drug expenditure (5.7%). The Framework also notes that social care expenditure has also increased in all categories, however in the last five years adult social care spend has risen broadly in line with GDP. v
We believe accelerating the pace of change in shifting the balance of care is required. To assist with this acceleration, we ask the Scottish Government to consider a re-evaluation of the aim that by the end of this Parliament, at least 50% of spending will take place in Community Health Service. We ask the Scottish Government to consider if this target was significantly more ambitious whether this would assist in driving changes in behaviour and practice.
We note the comments made by integration authorities that, in the context of rising demand it is an achievement just to prevent a further shift towards spending on acute services. In the context of rising demand, we ask the Scottish Government for its view on what further shift in the balance of care is considered realistic.
During the course of the Committee’s pre-budget scrutiny we explored two specific areas of health spending: mental health and alcohol and drug partnerships.
Mental health
Mental health and access to services is an area that is frequently raised with us as an area of concern. We carried out a short inquiry into mental health in Scotland in 2016 which fed into the Scottish Government’s new Mental Health Strategy.
The Scottish Government has previously stated that “investment in mental health will …exceed £5 billion over this Parliament.” The majority of this funding will be undertaken by IAs. We have previously noted how challenging it can be to get comprehensive information on spending in this priority area. The Scottish Government has recently responded to our concern by providing information on mental health spending by IAs.
In relation to the information provided, the Scottish Government notes that, in the first report, the information relates to NHS service budgets specifically identified as Mental Health, which are part of Integration Authority budgets. However, the letter notes—
“…the Scottish Government and a pilot Integration Authority are now developing a methodology for identifying all mental health related expenditure in Integration Authority budgets, including local authority service spend and all NHS services (including prescribing). This will be used to assess the progress towards achievement of the Scottish Government’s target for the share of total resources to support mental health increasing as a proportion of the total health budget.”
The information provided shows the total forecast expenditure on mental health services by IAs in 2017‑18 to be £554m. This represents an increase of 3.4% on 2016-17. However, it also shows large variations between IAs in the changes to mental health expenditure, from a reduction of 3.5% in mental health expenditure in Scottish Borders, to an increase of 28.9% in Shetland. For some IAs, expenditure on mental health services in 2017-18 was lower than the budget allocated to these services.
We explored in an oral evidence session with IAs their spending on mental health services. IAs provided some examples of changes they had made in the provision of mental health services. Some IAs cited a move from in-patient care to provision of services and support in a community setting. Some IAs referred to the role of link workers and work with GP practices in their localities.
Judith Proctor of Edinburgh Health and Social Care Partnership told the Committee—
“We need to consider the entire spectrum across mental health services, from primary prevention and promotion of mental wellbeing to support for people, whether they have low-level mental health issues or long-term and enduring problems.”i
Eddie Fraser of East Ayrshire Health and Social Care Partnership suggested that the benefits of the extra investment would be seen at what he termed ‘the lower-level preventative end’ in primary mental health rather than acute mental health which their current mental health teams focused on. i
During oral evidence, several IAs discussed the increase in demand on CAMHS. Janice Hewitt, North Lanarkshire Health and Social Care Partnership noted referrals to their child and adolescent mental health services have risen in tier 3 and ‘severe’ by 23%. She spoke about the need to invest properly in the right range of practitioners to address these issues. i
Robert McCulloch-Graham of Scottish Borders Health and Social Care Partnership, noted the need to make sure link workers were available in clusters and community work, to deal with lower level issues which if not addressed promptly developed into more serious cases.i
The Committee heard during its recent informal visits to schools and colleges as part of its work on the Year of Young People 2018 that further work should be undertaken to look at transition services from CAMHS to adult services. One of the main concerns expressed was for those experiencing mental health issues they were cut off from CAMHS at 18 and had to join a waiting list for adult services. A number of those we spoke with told us they had tried to commit suicide in the intervening period. They felt abandoned by the system.
In our evidence session with the Scottish Government we explored some of the concerns IAs had raised regarding mental health service provision and discussed the additional Scottish Government investment of £35 million in mental health over the next five years.
We also sought further information from the Scottish Government on its commitment to fund an additional 800 mental health workers over five years in key settings like A&Es, GP surgeries, custody suites, and prisons.
The Director-General Health stated in correspondence that the Scottish Government were currently finalising plans with IAs regarding the additional workers. Plans would be considered by the Health and Justice Collaboration Improvement Board in September.
Following the concerns raised by IAs in oral evidence regarding provision of CAMHS services on 29 June a new CAMHS Taskforce was announced by the Scottish Government. The taskforce is to look at reshaping and improving CAMHS supported with £5 million of investment. Paul Gray, Director-General in correspondence to the Committee confirmed the funding for the new CAMHS taskforce was additional to the £35 million workforce funding.
We also sought to explore with the Scottish Government not only the level of investment in mental health services but how it determined the effectiveness of the spending. Shirley Rogers, Director of Health Workforce and Strategic Change, highlighted the challenge faced in being able to determine the saving made in mental health spending due to investment in early intervention. She told the Committee—
“With the multidisciplinary teams, we are trying to ensure that early intervention prevents escalation. That means that the point about the effectiveness of the spend becomes even more complicated, because we look for an achievement from that early intervention and try to calculate what any failure to intervene appropriately at an early stage means for the clinical condition thereafter.”v
The Chief Medical Officer also discussed the provision of mental health services and stated the need for an active transition from CAMHS to adult services had not previously been recognised. She stated the Scottish Government now understood the need for such a transition service.v
There is broad agreement of the need to achieve parity of esteem between mental and physical health. This can only be achieved if there is adequate investment in mental health services to deliver the outcomes that are required.
We note the ambition to spend £5billion on mental health during this Parliament. We note that some increases have been promised and we would welcome from the Scottish Government detail setting out anticipated spending in all areas which will result in the £5billion target to be met.
To date, investment does not appear to be delivering the outcomes that are required. We have continued to hear concerns regarding access to services and support for those with mental health conditions since the publication of the Scottish Government’s Mental Health Strategy in 2016.
We therefore welcome the additional investment of £35 million in mental health over the next five years. We also welcome the recognition of specific concerns regarding the provision of CAMHS services through the additional investment of £5 million for a new CAMHS Taskforce.
We note that, to date, some IAs have spent less than the budget that has been allocated to these services. Given concerns raised regarding mental health service provision we find it difficult to understand why this is the case. We ask the Scottish Government to clarify if those areas are currently delivering an adequate service and meeting targets. The Committee also asks the Scottish Government what assurances can be given that the funding allocated to mental health and specifically CAMHS will be utilised for that purpose.
We note that the Scottish Government, along with a pilot integration authority, is developing a methodology for identifying all mental health related expenditure. We request an update on this work and confirmation of when this methodology will be adopted by all integration authorities.
Whilst investment in mental health services is important, ultimately it is the outcomes of this investment which should be the focus. We note the complexities faced in linking investment to outcomes especially when mental health spend deals with expenditure across both primary care and social care. However, we believe this assessment is vital to determine that funds are being allocated and used appropriately to deliver the right services and ensure the correct outcomes are achieved. We believe this is an issue the Scottish Government must prioritise, especially given the high levels of additional investment it wishes to make in this area. We ask the Scottish Government to confirm how it proposes to measure the effectiveness of any such investment.
We believe specific focus should be given to assessing the outcomes of investment in preventative spend in mental health. Our recent inquiry on preventative health and public health has found a lack of a longer-term focus and strategic direction to increase preventative action. We acknowledge there are challenges faced in being able to determine the saving made in mental health spending due to investment in early intervention. However, we believe this requires to be quantified to identify both the financial and practical benefits of adopting this approach. It is important investment in preventative spend on mental health is evaluated and its cost effectiveness assessed. We call upon the Scottish Government to provide details on how this information will be included in budget documents.
We recognise the importance of improving transition services from CAMHS to adult services. We therefore welcome the acknowledgement by the Chief Medical Officer of the importance of this service. We ask specifically how the additional investment in mental health services will ensure concerns regarding lack of a transition service is addressed.
We also ask the Scottish Government to provide an update on the allocation of 800 mental health workers since its consideration by the Health and Justice Collaboration Improvement Board in September. We are specifically interested in how it has determined what type of mental health workers will be appointed and where to. We request further information on how the approach taken to determining allocation will ensure the appropriate outcomes for mental health can be delivered.
Alcohol and Drug Partnerships
In our Pre-budget report 2017 we were very critical of the lack of comprehensive information on Alcohol and Drug Partnerships (ADPs) budgets and spending and were concerned by reports of the need to submit Freedom of Information requests to obtain information on the allocation of funding to specific areas.
The issue of ADPs has also been raised within the context of our specific work on substance misuse, as part of our inquiry on preventative agenda. Following our consideration of the issue of substance misuse we wrote to the then Minister for Public Health and Sport on 6 March 2018 with our findings. In our letter we noted that funding for Alcohol and Drug Partnerships was reduced by 22 per cent in cash terms, from £69.2m in 2015-16 to £53.8m in 2016-17 and 2017-18. In our letter we observed that NHS boards were expected to maintain existing services, resources and outcomes at 2015/16 levels yet we had heard a number of health boards had not made up the shortfall.i
Our letter also raised concerns at the number of drug-related deaths in Scotland and the rate of deaths in comparison to other countries. The number of drug-related deaths in Scotland had steadily increased over the last 20 years, rising from 244 in 1996 to 867 in 2016.
In response to our letter the Scottish Government indicated that its refresh of the substance misuse strategy would address the concerns we raised.
The then Cabinet Secretary for Health and Sport also wrote to us in May 2018 with some initial information on spend in ADPs. There were some caveats attached to the data and it was seen as a first step in reporting in this area.
The information provided by the Scottish Government showed a total spend by ADPs of £101.7m in 2017-18, representing a decrease of 1.4% on the previous year. The data also showed some variation between IAs in the changes to ADP expenditure, from a reduction of 15% in ADP expenditure in Argyll and Bute, to an increase of 60% in Angus. Whilst for some IAs spend was in line with the budget, for others expenditure on ADP services was lower than the budget allocated.
The letter also detailed that the Scottish Government expected a significant increase in spend in 2018-19, reflecting the new investment in this area of £20 million.
In August 2018 a letter from the Director-General confirmed the allocation of both the baseline funding to ADPs and the additional £20m had now been agreed. The instruction issued to NHS Chief Executives from the Scottish Government on ADP funding states—
“The allocations described in this letter represent the minimum amounts that should be expended on alcohol and drug treatment and prevention services in 2018-19. We fully expect that additional resources, including funding, will continue to be contributed by ADP partners with an emphasis on investment in innovation and prevention.”iii
In our evidence session with the Scottish Government we explored the concerns that in some IAs spend on ADPs had been lower than the budget allocated. Christine McLaughlin told the Committee—
“we also need to understand whether an area has been able to deliver what it needs to deliver with fewer funds. If it is a case of a reduction in spend and not delivering outcomes, you would expect us to take the same action that we would take for any area of performance. However, you can be assured that the area is one of real priority and that we will focus on understanding how that money is invested.”iv
We are very concerned at the high number of drug-related deaths in Scotland and the rate of deaths in comparison to other countries. We believe a reduction in drug related deaths must be a priority area for the Scottish Government. We still await publication of the Scottish Government's refreshed substance misuse strategy and ask the Scottish Government to confirm when this will be published.
We welcome the additional investment of £20 million to ADPs. In the absence of the refreshed strategy and a methodology to measure impact we ask the Scottish Government what assurances it can provide that this funding will be invested effectively to deliver the outcomes that are required, including the reduction of drug related deaths.
We are concerned that, to date, some IAs spend on ADPs has been lower than the budget allocated. This approach would be appropriate if IAs were delivering the outcomes that are required with less funding. However, given the high number of drug-related deaths we are concerned that NHS boards and ultimately IAs have not given this issue the priority that is required and are not investing the level of funds into services required to deliver improved outcomes. We are disappointed IAs and health boards have not felt it appropriate to prioritise action on this and now ask the Scottish Government what steps it will take to ensure this issue is prioritised and the number of drug-related deaths reduced.
The Committee welcomes the assurance that the Scottish Government will now provide information on ADP budget and expenditures on a regular basis. The Committee hopes that the Scottish Government will continue to seek to improve the quality and comparability of the data provided.
Annex A - Minutes of meetings
11th Meeting, 2018 (Session 5) Tuesday 27 March 2018
3. Pre-budget scrutiny (in private): The Committee considered and agreed its approach to pre-budget scrutiny 2019-20.
17th Meeting, 2018 (Session 5) Tuesday 22 May 2018
1. Pre-budget scrutiny 2019-20 : The Committee took evidence from—
Judith Proctor, Chief Officer, Edinburgh Health and Social Care Partnership;
Eddie Fraser, Director of Health and Social Care, East Ayrshire Health and Social Care Partnership;
Pam Gowans, Chief Officer, Health and Social Care, Moray Health and Social Care Partnership;
Janice Hewitt, Chief Accountable Officer, North Lanarkshire Health and Social Care Partnership;
Robert McCulloch-Graham, Chief Officer, Health and Social Care, Scottish Borders Health and Social Care Partnership.
2. Pre-budget scrutiny 2019-20 (in private): The Committee considered the evidence heard earlier in the session.
18th Meeting, 2018 (Session 5) Tuesday 5 June 2018
3. Pre-budget scrutiny 2019-20: The Committee took evidence from—
Paul Gray, Director-General Health & Social Care and Chief Executive NHSScotland;
Christine McLaughlin, Director of Health Finance;
Shirley Rogers, Director of Health Workforce and Strategic Change;
Dr Catherine Calderwood, Chief Medical Officer, and
Alison Taylor, Head of Integration Division, all Scottish Government.
9. Pre-budget scrutiny 2019-20 (in private): The Committee considered the evidence heard earlier in the session. The Committee agreed to issue a draft report on pre-budget scrutiny 2019-20.
26th Meeting, 2018 (Session 5) Tuesday 23 October 2018
1. Pre-Budget Scrutiny (in private): The Committee considered and agreed a draft report on its Pre-Budget Scrutiny.
5. Pre-Budget Scrutiny (in private): This item was not considered given the conclusion at Agenda item 1 above.
Annexe B - Evidence
Written evidence - integration authorities survey responses on budget information
Written evidence
Additional written evidence
Official Reports
Tuesday 22 May 2018 - evidence from Integration Joint Boards
Tuesday 5 June 2018 - evidence from the Scottish Government