Health inequality and COVID-19 in Scotland
The COVID-19 pandemic has impacted everyone in Scotland but the impact has not been spread evenly across society. This briefing outlines how different groups have been affected by direct and indirect health harms of the pandemic, and how existing health inequalities have been exacerbated.
Summary
Health inequalities are defined by public health professionals and academics as “avoidable and unjust differences in people’s health across the population”. Many researchers and professionals in public health see them as avoidable and unjust because they can be outside of an individual's control, and caused by structural differences in society and the economy. This briefing explains what health inequalities are in a Scottish context, and looks at how they are being and might continue to be affected by the COVID-19 pandemic.
The concept of "health inequalities" is regularly used by the Scottish and UK Governments, along with organisations such as Public Health Scotland and the NHS. It is also in wide use internationally, although is sometimes known as "health inequity" elsewhere.
Health inequalities in Scotland affect a wide range of different groups, including:
disabled people
people from ethnic minorities
people who live in deprived areas
the unemployed
vulnerable groups such as refugees and rough sleepers.
Health inequalities mean there are differences in health between these groups and the rest of the population, such as:
reduced life expectancy
greater incidence of cancer
greater mortality from heart disease
worse reported mental health and wellbeing.
Reducing these inequalities in health has been prioritised by the Scottish Government and the NHS for a long time but, in recent years, improvements in average life expectancy have stalled, and the gap in life expectancy between the most and least deprived areas has increased.
In March 2020, Scotland began to feel the direct effects of the COVID-19 pandemic. Cases began to spread rapidly, and restrictions were introduced to limit the spread of the disease. Harms from the disease were not spread evenly across society. For example:
those from the most deprived areas were much more likely to be admitted to hospital with serious illness from COVID-19
the death rate from the virus in the most deprived areas was double that of the rate in the least deprived areas
people of South Asian background were around twice as likely to die from COVID-19 compared to white people.
COVID-19 can also cause long term illness which has become known as 'long COVID'. It is not known how many people are suffering from long COVID in Scotland, but it is estimated to be in the thousands. Long COVID is more likely to affect women than men.
Restrictions to daily life introduced in March 2020 to control the spread of COVID-19 have had a myriad of adverse effects on people's health and well-being, such as:
some routine healthcare treatments delayed or cancelled
screening for cancer and other diseases paused
GP appointments moved online
non-urgent dental and optometry appointments cancelled
isolation and loneliness increased
education disrupted
food insecurity increased.
All of these harms have had a disproportionate impact on a range of groups, including:
those who were already suffering from poor physical and mental health
people from ethnic minorities
women
younger people and children
low-paid workers.
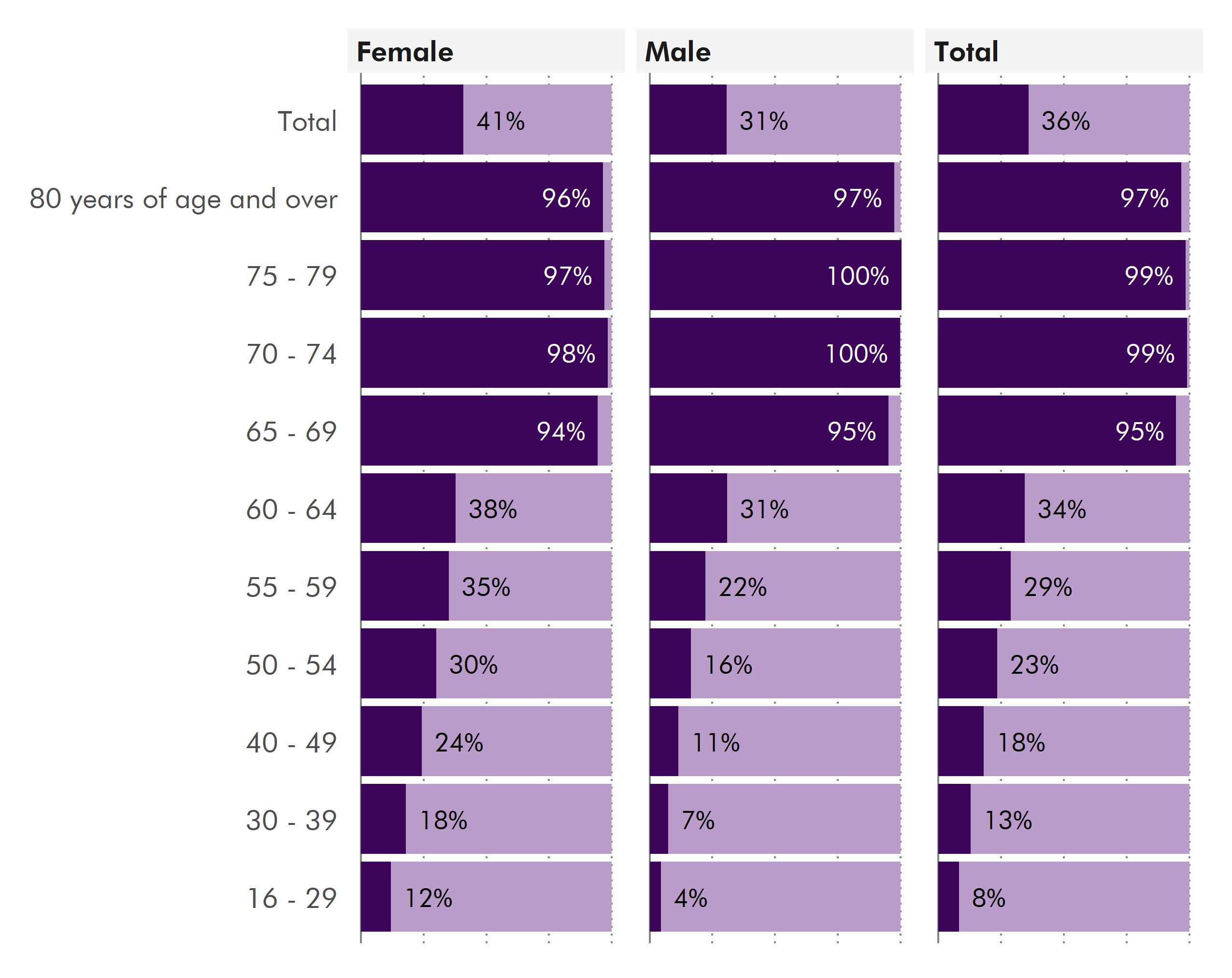
The vaccination programme has progressed very quickly since vaccinations began in December 2020. Prioritisation of vaccination has been carried out following UK-wide guidance issued by the Joint Committee for Vaccination and Immunisation, according to age and clinical vulnerability. People's occupation (with the exception of health and care workers), ethnic background or level of deprivation has not been taken into account.
It is feared that vaccine uptake has been lower in some groups of people and areas of Scotland. This includes people from some ethnic minority groups. This risks introducing more inequality in vulnerability to COVID-19.
Reports by organisations such as The Institute of Health Equity say that the recovery from the pandemic could provide an opportunity to rebuild Scottish society and the economy in a way that prioritises addressing inequality and poverty, whilst tackling the challenges of the climate crisis. The COVID-19 pandemic has shone a light on existing health inequalities across society. If they are not focused on in the recovery, academics and public health professionals expect that gaps in health outcomes and access to services will continue to increase.
An introduction to health inequalities
Health inequalities are defined by Public Health Scotland and others as “avoidable and unjust differences in people’s health across the population”.123 Variations in health across a population are not necessarily health inequalities. If these differences affect certain groups in the population in a way that is unfair and avoidable, they are seen as inequalities. These differences in health are considered by some to be socially unjust because they are avoidable, and outside an individual’s control. They are seen as being determined by the conditions in which people are born, grow, live, work and age. These conditions are seen to disadvantage people and affect their opportunity to enjoy good physical and mental health.
Health inequalities in society have a wide variety of effects which can be seen across a range of health outcomes. For example, healthy life expectancy is the length of time a person can expect to live in good health. Healthy life expectancy varies drastically between the most and least deprived areas. In the least deprived areas of Scotland, a boy born now can expect to spend 26 years longer in good health than a boy born in the most deprived areas. The differences for women are similarly large: a girl born in the least-deprived areas can expect to spend 22 years longer in good health than a girl born in the most deprived areas.4
In the most deprived areas of Scotland, healthy life expectancy is 26 years shorter for men and 22 years shorter for women compared to the least deprived areas
What causes health inequalities?
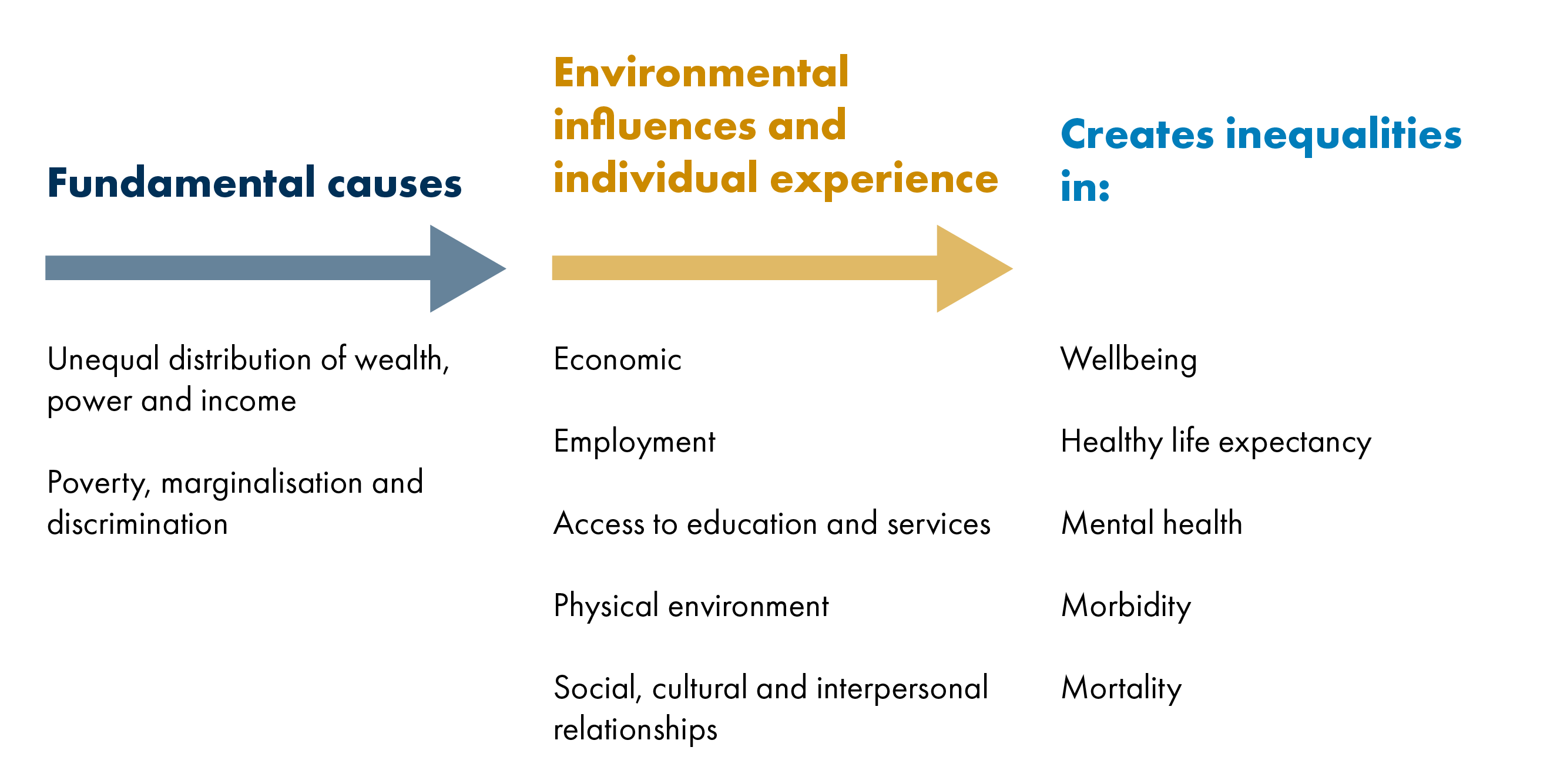
According to Public Health Scotland and academic research, health inequalities are "fundamentally caused by the uneven distribution across society of income, wealth and power".1 Political and policy decisions can influence this distribution. These fundamental causes affect the wider environment that people live in, such as their access to good quality housing, healthcare, work, education and services. People’s experience of their environment, such as poor housing, low income, unemployment, poor education and barriers to access services then results in health inequalities. These circumstances are known as the 'social determinants of health'. Figure 1 below, adapted from Public Health Scotland material, shows the main causes and effects of health inequalities.
Who is affected by health inequalities?
Health inequalities exist across many different groups in society.1
Health inequalities can exist across groups affected by many factors as listed below, but this list is not exhaustive.
Socio-economic position and deprivation (low income, unemployment, poor housing, poor education).
Protected characteristics (age, sex, sexual orientation, race, disability, pregnancy and maternity, religion or belief).
Vulnerable groups in society such as asylum seekers, migrants, people with learning disabilities,homeless people and rough sleepers, Gypsy, Roma and Traveller groups, sex workers, prisoners.
Geography (urban compared to rural, island compared to mainland).
Intersectionality
These groups affected by health inequalities do not exist in isolation. The links between different groups and the inequalities they experience is sometimes described as ‘intersectionality’. Intersectionality is defined as “the interconnected nature of social categorisations such as race, class, and gender, regarded as creating overlapping and interdependent systems of discrimination or disadvantage”. 1 It is important to consider the effect of this intersectionality on people. Data available on health tends to group people into individual categories, such as by ethnic background or gender. People who fit into several of these groups can experience inequalities which combine and increase their disadvantage. For example, a woman from an ethnic minority background living with a disability will have different experiences from a white man without a disability. These experiences will differ because she is a woman, because she is from an ethnic minority background, and because she has a disability.
Inequalities in healthcare access and health outcomes
Inequalities exist in the access people have to healthcare, the services they receive, and the outcomes they experience. The 'Inverse Care Law' is used by public health professionals and academics to describe how people with the most need of healthcare are the least likely to use it.
In the UK, the NHS is universally available, which limits inequalities in access to services, but they still exist. Someone living in a remote rural area may not be able to access specialist health treatment as easily as someone living in a major city. High demand and availability of private services in some sectors, such as dentistry and physiotherapy, can lead to inequalities in access. People in society who are particularly vulnerable, such as homeless people, may experience difficulties in accessing healthcare. According to Scotland's Public Health Observatory, this could be because they aren't able to engage with support services and may not be registered with a GP, or have difficulty communicating their needs.
Inequalities in health outcomes can arise due to inequalities in healthcare access, but also arise because of the fundamental causes of health inequalities such as deprivation, poor housing, low income, and the wider environment people live in. It is common for some groups of people to experience inequalities in health outcomes despite good access to healthcare.
How do we measure health inequality?
If health inequalities are to be addressed effectively, they must be measured and monitored to evaluate how measures are performing, but not at the expense of action. Health inequalities can be measured and monitored in a range of ways. The Scottish Government produces annual statistics monitoring health inequalities. These include data showing the numbers of deaths from different causes in groups across society, such as deaths from coronary heart disease by socio-economic deprivation level, deaths from all causes across different ethnic groups in society, and deaths from drugs and alcohol by sex.
In order to understand how inequalities change over time, they need to be monitored. Two common metrics used in longer term monitoring data in Scotland are the Relative Inequality Index (RII), and the Absolute Inequality. Both of these metrics rank the population by deprivation level. The RII measures how steep the gradient of health outcomes is across the deprivation levels, relative to the average health of the population. The bigger the RII, the bigger the difference between the most deprived and the population average. The advantage of this metric is that it is based on data from across the population.1
Absolute inequality is the difference between the most and least deprived groups in the population. It can be calculated on a wide range of data. For example the difference in life expectancy in years, or the difference in cancer incidence per 100,000 people. This type of metric has the advantage of being intuitive to understand, but only looks at extremes at either end of the scale, and neglects people in between.
Health inequality in Scotland before the pandemic
Health inequalities in Scotland
Until the middle of the 20th century, life expectancy in Scotland was comparable to the rest of Western Europe. However, in the last few decades, average life expectancy in Scotland has not improved at the same rate as elsewhere.1
In 1977, the UK Government commissioned an independent enquiry to look at the connections between people's health and their social class. The 'Black Report' was published in 1980.2 The report drew attention to differences in mortality across the social classes, showing those in the poorest groups suffering the highest mortality. It also noted that people in working class groups were less likely to access preventative services. The report recommended improving social welfare by measures such as by increasing child benefit, and improving housing quality. However, there was a change of government since the report was commissioned, and the new administration did not accept the recommendations in it.
In 1998, the Acheson Report3 was published after the new government in 1997 commissioned another independent inquiry into health inequalities. This report recommended putting public health and health inequalities at the heart of decision making processes.
Twelve years later in 2010, the Marmot Review4 was published. It showed that stark inequalities were still present in the UK, and proposed strategies to address them. These centred on action to deal with the social determinants of health, such as improving employment prospects, improving education and services for children and strengthening preventative health measures.
In 2020, just prior to the COVID-19 pandemic, the Institute of Health Equity published a follow-up report to its 2010 report, called 'The Marmot Review: 10 years on'.5 It reported that since 2010, improvements to life expectancy had stalled, and for some groups actually fallen. Health inequalities had widened over the preceding decade.
It is worth noting that all these reviews made very similar recommendations to address health inequalities.6
The 'Glasgow effect'
It is recognised that much of the research into health inequalities carried out in England and Wales or the UK as a whole is relevant to Scotland. However, Scotland does show differences when compared to England and Wales, particularly in excess mortality. This difference is known as the 'Glasgow Effect' because it is observed most strongly in Glasgow and the west of Scotland, but it is seen across the whole of Scotland. In 2015, premature mortality (here defined as death before age 65) was 20% higher across Scotland in than in England and Wales, and is 30% higher in Glasgow when compared with similar cities such as Manchester, Liverpool and Belfast.1
Research has suggested that a combination of historical policies of managed decline and de-industrialisation contributed to the Glasgow effect, and could account for the greater premature mortality compared to similar cities elsewhere in the UK.
Health inequalities in 2019
The Scottish Government publishes annual statistics which monitor health inequalities across a range of health indicators in relation to deprivation level. The most recent pre-COVID-19 figures cover 2019.1 They show that large health inequalities exist between the least and most deprived people, and in some instances the gaps have increased and are at their highest ever levels.
For example, healthy life expectancy (HLE) is the number of years a new born baby can expect to live in good health. For both males and females, there is a large gap between the most and least deprived areas.
Premature mortality is defined as dying before reaching the age of 75 years. This measure also shows a significant gap between the most and least deprived.
The premature death rate per 100,000 people was 817.6 in the most deprived areas, compared with 198.2 per 100,000 in the least deprived areas.
Differences are not just present in deaths. Mental wellbeing and morbidity from diseases also vary greatly across the deprivation scale. For example, in 2019, using data from the Scottish Health Survey, 24% of adults in the most deprived areas had below average wellbeing, compared with 9% in the least deprived areas.1 The admission rate to hospital for heart attacks in the most deprived areas was over double that of those living in the least deprived areas. Cancer incidence is more common in the most deprived areas of Scotland, although this is not true for all types.3 Higher incidences of some types of cancer in the least deprived areas could be driven by higher screening uptake, but there is debate about the extent of these effects. They could be due to inequalities in healthcare access.
Policies to address health inequalities
In 2013, the Scottish Parliament Health and Sport committee conducted an inquiry into health inequalities.1 Witnesses highlighted that measures which focus on changing harmful behaviours almost always fail to address health inequalities, possibly because these policies are often universal and therefore not targeted at those most in need. Examples include public health campaigns to reduce harmful behaviours such as consuming alcohol, smoking and not exercising regularly. The committee concluded that to improve health inequalities, the fundamental causes need to be addressed. This is difficult because it requires action from all sectors of government, rather than just the NHS.
In 2012, Audit Scotland published a report into health inequalities. It found that measures taken to try to address health inequalities had generally had poor results, and that more partnership working was needed across different parts of the NHS and government.
Public Health Scotland has developed an interactive tool which allows users to model the impact of various interventions on health inequalities. It allows users to investigate how different metrics of health outcomes, such as hospital stays and premature deaths, are affected by policies including income redistribution, the physical environment and alcohol and drug use. A report was published in 2019 outlining the modelling of interventions and their impacts at a Scotland-wide, and more local scale.
Some specific policies have been successful at reducing harmful behaviours. Smoking cessation services may have been successful: the percentage of adults smoking in Scotland fell from 25% to 17% between 2009 and 2019, although the gap in smoking prevalence between the most and least deprived areas grew between 2017 and 2019 to 26%.2 It is not clear to what extent smoking cessation services have contributed to this decline in overall smoking prevalence. Public Health Scotland found that smoking cessation services could reduce health inequalities but only if targeted in the right way.
Violent crime disproportionately affects those living in more deprived communities. In 2005, the Scottish Violence Reduction Unit was set up, which is a partnership between the Scottish Government, Police Scotland, the NHS and other groups. It treats violence as a public health problem, aiming to reduce homicides by addressing the causes of violence. Since 2010 homicides in Scotland have fallen by about a third, but it is not known to what extent this fall is due to violence reduction strategies compared to wider societal and behavioural changes.
Teenage pregnancy has historically been higher in Scotland than in comparable western European countries, with a large gap in the rate between the most and least deprived areas. The gap between the rate in the most and least deprived areas has reduced since 2008, and the absolute rates have reduced for all levels of deprivation over the same period. In 2016 the Scottish Government published its strategy to reduce teenage pregnancies and inequalities. The reduction in teenage pregnancy rates started before the Scottish Government's strategy was published, so other factors such as wider behaviour shifts are thought to be occurring too.
The COVID-19 pandemic in Scotland – a brief overview
What is COVID-19?
COVID-19 is a new disease caused by the Sars-CoV-2 virus, which is a coronavirus. Other coronaviruses include those that cause the common cold, and more serious illnesses such as Middle East Respiratory Sydrome (MERS) or Severe Acute Respiratory Syndrome (SARS).
COVID-19 first emerged in China in late 2019. It is a disease which mainly affects the respiratory system of the body.
For most people, COVID-19 results in mild or moderate respiratory illness and they will recover without special treatment. People with underlying health conditions and older people are at greater risk of serious illness or death if they contract COVID-19.
COVID-19 is highly infectious and spreads through the air when people breathe, speak, cough or sneeze, or when they touch surfaces where it has landed then touch their eyes, nose or mouth.
Asymptomatic transmission is possible with COVID-19. This means that people can carry the disease without experiencing any illness, but can still transmit it to others. This makes the disease more difficult to control. If people are unaware they have the disease, they are more likely to maintain contact with other people and attend work and social settings.
COVID-19 in Scotland
COVID-19 reached Europe early in 2020, and the first cases were identified in Scotland in March 2020. The first confirmed death in Scotland from COVID-19 occurred on 13 March 2020. Hospitalisations and deaths increased dramatically during late March and April 2020.
In March 2020, the Scottish Government introduced restrictions on daily life to reduce the transmission of the virus. The main aim of these restrictions was to stop hospitals becoming overwhelmed with the number of COVID-19 patients. Restrictions were eased during summer 2020, but cases began to rise again and restrictions were reintroduced, initially targeted in specific areas such as the West of Scotland and Aberdeen, but more widespread rules were introduced in September 2020. Later in the Autumn, stricter rules were imposed, then a new national lockdown was announced in January 2021. More detail on the timeline of the COVID-19 pandemic in Scotland can be found in the SPICe blog 'Timeline of Coronavirus (COVID-19) in Scotland.'
Long COVID
COVID-19 can also cause longer-term illness, called post-COVID-19 syndrome. This has become known as 'long COVID'. Symptoms can persist for 12 weeks or more after the original infection. The symptoms that have been reported are wide-ranging. They can include respiratory, digestive system, muscular, cardiovascular and neurological symptoms, although this list is not exhaustive.
Studies have shown a significant proportion of COVID-19 patients can expect to experience some long-term symptoms.1 In England, over 20% of people who had COVID-19 experienced symptoms lasting longer than five weeks. 30% of COVID-19 hospital patients were readmitted to hospital within five months of being discharged
Research is ongoing into long COVID, and it is not known exactly how many people in Scotland have symptoms, or how long they will last. It has been estimated that 6,000 people in Scotland may have long COVID symptoms from the first wave of infections in 2020, with this number not taking account of the large number of cases in winter 2020-21. The Health Secretary Jeane Freeman, in response to a parliamentary question, said "At present there are no plans to establish a national register of people experiencing symptoms of Long COVID."
In Scotland, the NHS is planning to manage long COVID through GPs, rather than setting up specialist clinics as is the case in England. In response to a parliamentary question, the Health Secretary said "There are already a range of services in place, to support people experiencing symptoms of Long COVID, including local primary care teams, community based rehabilitation services and specialised secondary care where needed...".
The Scottish Intercollegiate Guideline Network has issued guidelines for the treatment of long COVID symptoms.
The impacts of COVID-19 in Scotland
COVID-19 has a wide range of impacts on the whole of society. These impacts are caused by the illness and death from the disease itself. They are also caused by the restrictions introduced to control the spread of the virus. It can be helpful to break up these impacts into two groups: direct health harms, and indirect health harms.
Direct health harms are the illness and deaths caused by COVID-19 itself.
Indirect health harms are those caused by the restrictions to control COVID-19. These include impacts on non-COVID health services and social care, such as screening for cancer or cancellation of routine operations. These impacts have short and long term consequences for people's health. Indirect health harms also include impacts on people's mental health through economic and societal factors, such as loneliness, job security and disruption to education. These harms affect the fundamental causes of health inequalities: inequalities in wealth, income and power. Physical health indirect impacts include possible changes to people's diet and exercise habits, and greater exposure to domestic or family violence.
The Scottish Government has set out its strategic framework for dealing with COVID-19 by dealing with the 'four harms of COVID-19' .1 These four harms are:
The direct health harms from the virus.
The indirect health harms from wider impacts on health and care services.
Social harms due to restrictions affecting peoples way of life.
Economic harms from the restrictions having an impact on employment and prosperity.
This briefing will predominantly consider the first two harms, whilst recognising the interconnected nature of the impacts. The social and economic harms will also have long-term health impacts as they are important health determinants.
It is important to note that the changes brought by the pandemic have had some positive effects on health inequalities. For example, evaluation of online medical appointments found that for some people, such as those living in remote areas or in some hard to reach groups, access to services had been improved. A study by Stirling University found that for some drug users, access to support and treatment had been improved during the pandemic.
Direct health harms from COVID-19 and their uneven impact
As of 18 March 2021, since the start of the pandemic in March 2020, there have been 211,854 COVID-19 cases in Scotland, 14,580 hospitalisations and 9,831 deaths. These harms have not been distributed evenly across society.
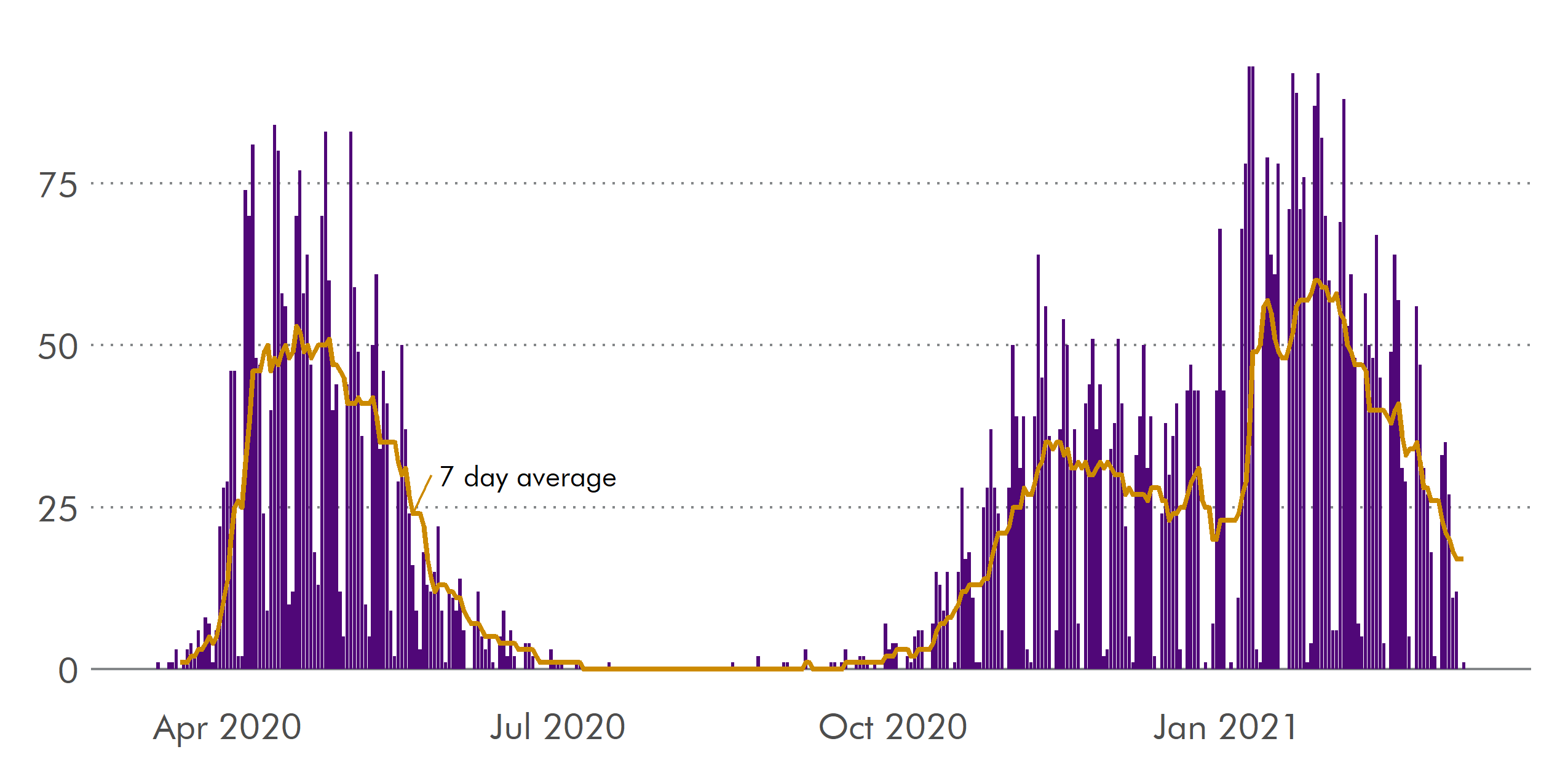
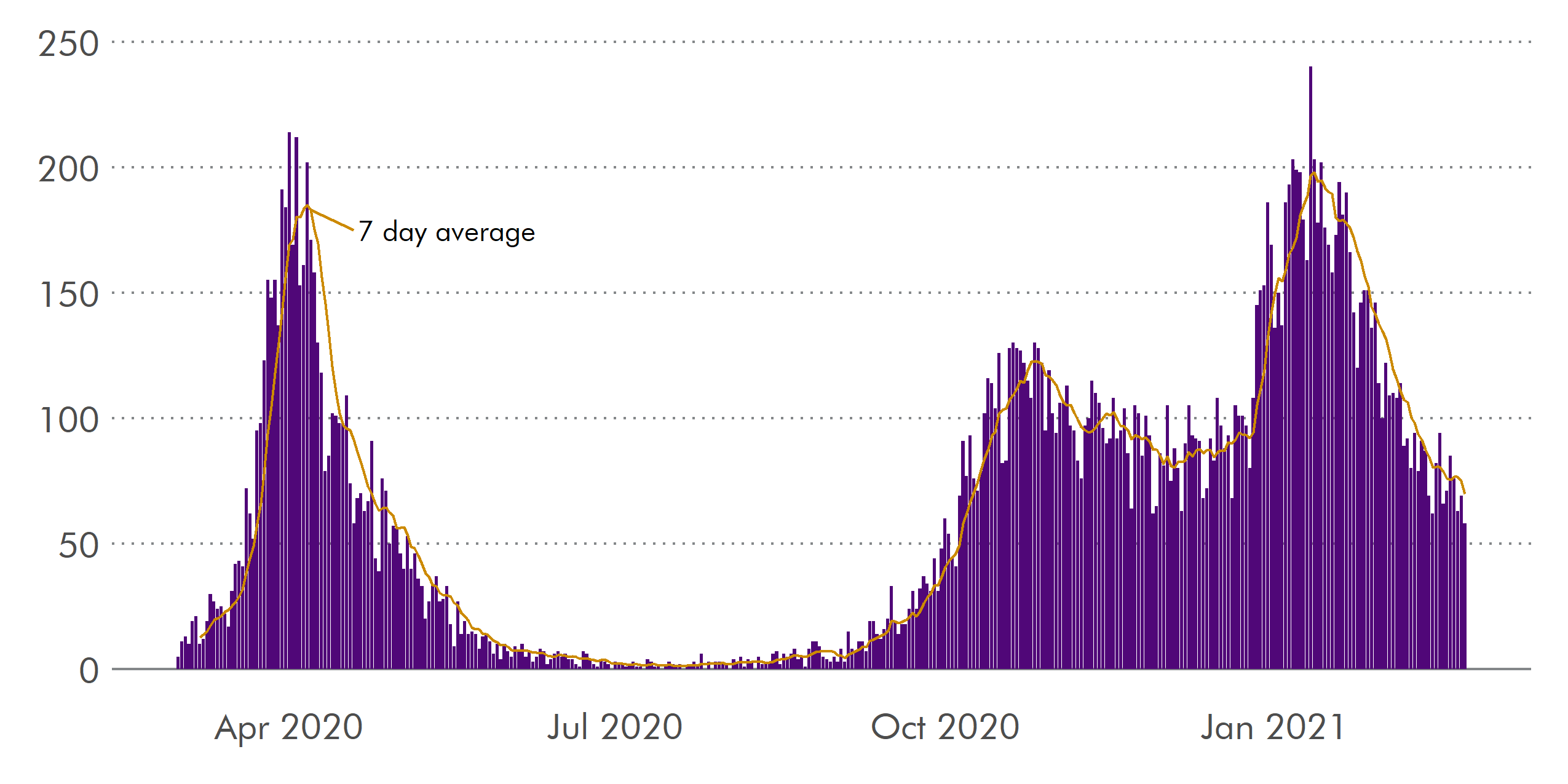
The pandemic has had two main 'waves' of infections which can be seen in figure 3 below: the first wave during Spring 2020, and the second wave starting in Autumn 2020.
Direct health harms and age
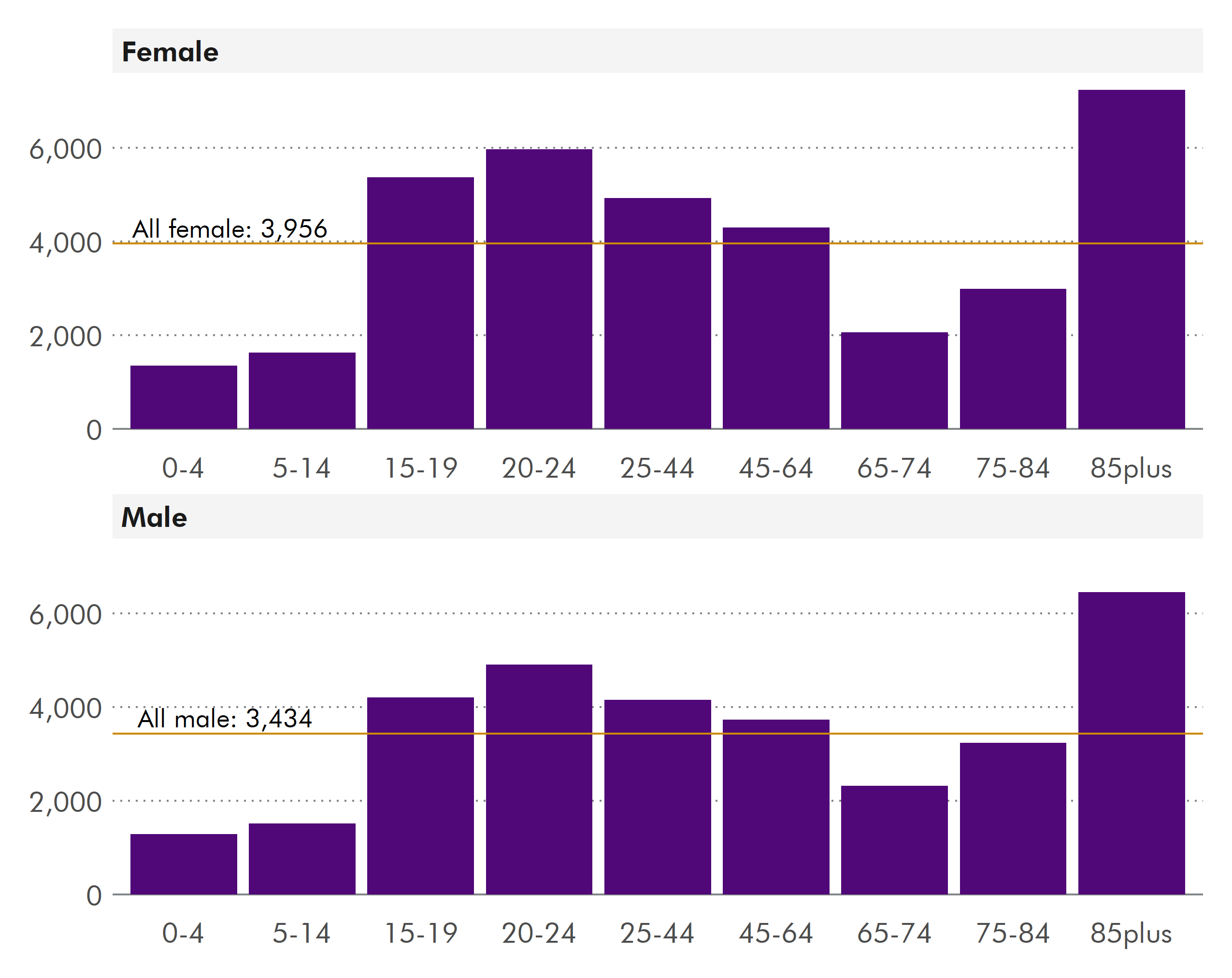
The direct health harms of COVID-19 have affected older people much more than young people. Cases have been more evenly spread across ages, but the rate is greatest for the oldest age groups in both men and women, which can be seen in figure 4. The rate for those aged 16-64 years is also high. The 65-84 years group has a relatively lower case rate, especially compared to the 85+ years group.
Older people have been much more likely to develop serious illness requiring hospital treatment. Hospitalisation rates per 100,000 people have been much higher for older age groups, shown in figure 5.

Deaths from COVID-19 have overwhelmingly affected older people. National Records of Scotland figures show that the death rate per 100,000 people from COVID-19 for both sexes in the older age groups is 688 per 100,000 for those aged 65-74 years and 1403 per 100,000 for those aged 75-84 years, but only 4 per 100,000 for those under 40 years.
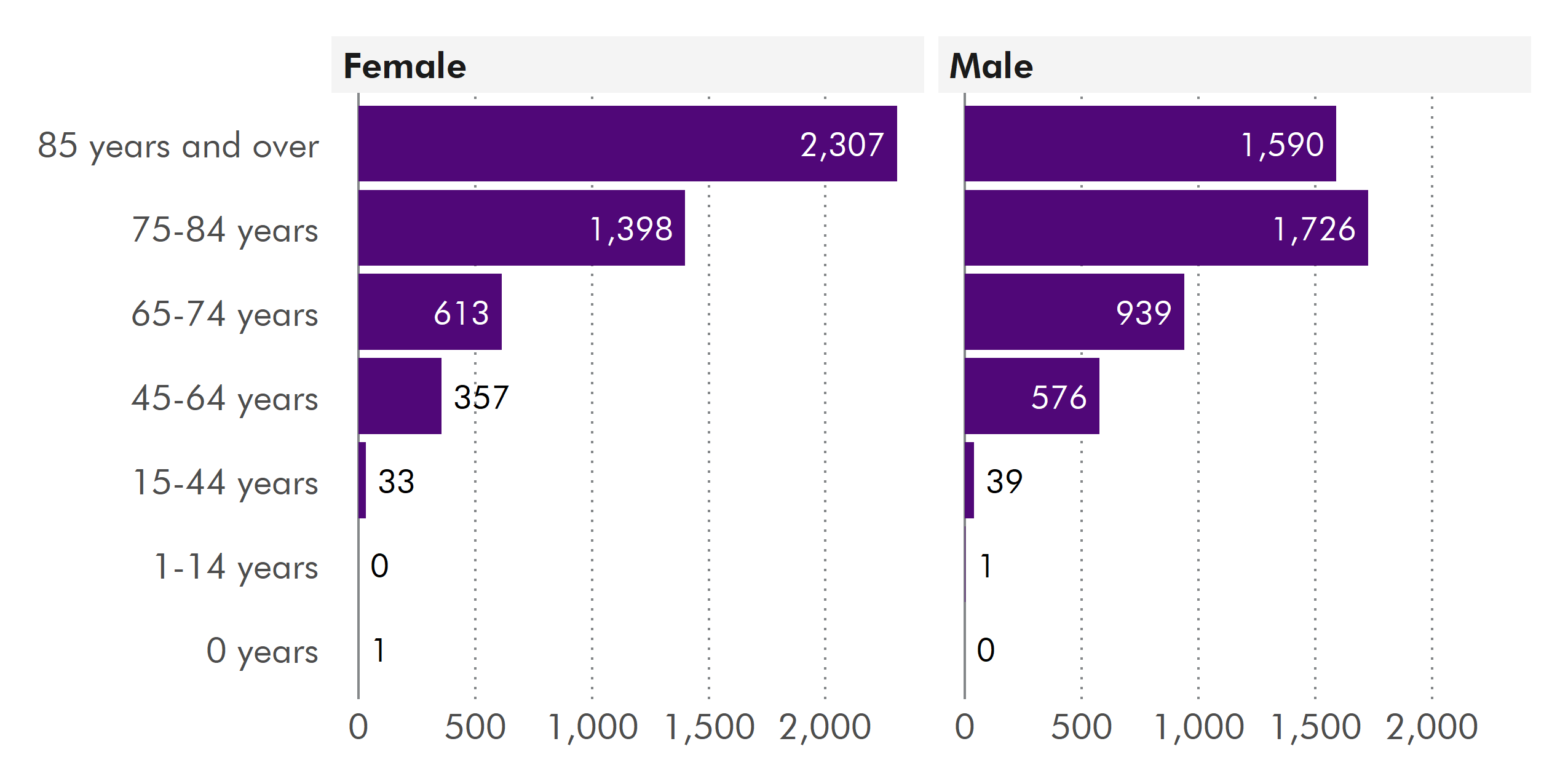
Direct health harms and gender
Since the beginning of the pandemic there have been more cases of COVID-19 in women have than men (see figure 4 in this section). This Scottish Government report into the impact of COVID-19 on equalities says that this is because women are more exposed to the virus: they are more likely to work in health and social care, are more likely to work in service industries and less likely to be able to work from home. It is possible that this could be due to differences in the take up of testing by men and women, perhaps because women make up a higher proportion of health and care workers who have been tested more than the general population.
However, the death rate per 100,000 people is greater for men than it is for women. For men at all ages, the age-standardised death rate from COVID-19 has been 217 per 100,000, whereas for women it is 147 per 100,000 (figures from National Records of Scotland). According to the Global Health 50/50 Project, there are many possible reasons for this difference. It could be because men are less likely to seek medical help until later on in the disease than women, or are more likely to participate in risky behaviours such as smoking and drinking alcohol.1 There is a long-standing debate pre-pandemic about the difference in mortality rates between men and women.
Direct health harms and ethnic group
Growing evidence has emerged throughout the course of the pandemic which highlights the inequalities impacting most on ethnic minorities. In a UK-wide study, people of ethnic minority background were most likely to test positive for COVID-19, with people of South Asian and Black background roughly three times more likely to test positive than white people.1 In another UK study, people of ethnic minority background were found to be around 30% more likely to be admitted to critical care than white people, and people of South Asian background were more likely to die if admitted to hospital with COVID-19. 2
National Records of Scotland analysed the ethnic background of deaths in the first wave of the pandemic.3 People of South Asian background were twice as likely to die as white people. Numbers of deaths in other ethnic minority groups were not large enough to calculate similar relative risks.
Public Health Scotland conducted analysis of rates of hospitalisation and death by ethnic group during both the first and second waves of infection. They found that people from an ethnic minority background were generally more likely than white people to require hospital treatment, and subsequently die from COVID-19. For some groups, the difference in death and hospitalisation rates were higher in the second wave than the first: for example, people of South Asian background were twice as likely to die or be hospitalised in the first wave, but were three times more likely to die or be hospitalised in the second wave.4
Greater morbidity and mortality in ethnic minority groups is likely due to a variety of clinical, social and economic factors. Structural racism was found by researchers at Manchester University to be an important driver in inequalities in COVID-19 outcomes in ethnic minority groups. Language and cultural barriers may prevent access to some health services. Some ethnic minority groups are more likely to live in multi-generational housing, which increases the risk of transmission to older relatives, and could make self isolation difficult. Ethnic minorities are over-represented in healthcare and other key worker industries, which may increase exposure. Some ethnic minority groups such as Gypsy/Roma travellers, asylum seekers and refugees are likely to experience barriers to engaging with healthcare services.
These factors, and intersectionalities between ethnic background and socio-economic deprivation mean that ethnic minorities in Scotland are more likely to be exposed to, and become seriously ill or die from, COVID-19.
Direct harms and disability
In Scotland, around 1 in 4 people live with a limiting long-term physical or mental health condition. This proportion increases to around one third of people in the most deprived areas, but is one sixth of people in the least deprived areas.
Disabled people experience elevated clinical risk from COVID-19 because of underlying chronic conditions and co-morbidities. Disabled people experience greater barriers in healthcare access, and this includes COVID-19 testing and vaccination. Some disabled people were told they would not be given life-saving treatment and would receive 'do not resuscitate' orders if they were seriously ill with COVID-19.
People living with learning disabilities already experienced health inequalities before COVID-19. Research during the first wave of infection found that, when compared to the general population, people with learning disabilities were around twice as likely to test positive for COVID-19, twice as likely to be hospitalised, and around three times more likely to die from COVID-19.1
Direct harms and deprivation
The links between poverty, deprivation and health outcomes are well-documented.
Statistics about deprivation in Scotland usually refer to the Scottish Index of Multiple Deprivation (SIMD). This ranks small areas called 'datazones' on their level of deprivation. This is calculated using data on factors such as employment, income, access to services and crime. These ranked zones can then be divided into groups such as 'quintiles' - this means five groups ranging from most deprived to least deprived. Statistics on deprivation in this briefing refer to the most and least deprived quintiles, where 1 is the most deprived, and 5 is the least deprived.
COVID-19 has affected the most deprived areas in Scotland much more than better off areas. There have been more COVID-19 cases in the most deprived areas than the least deprived areas.
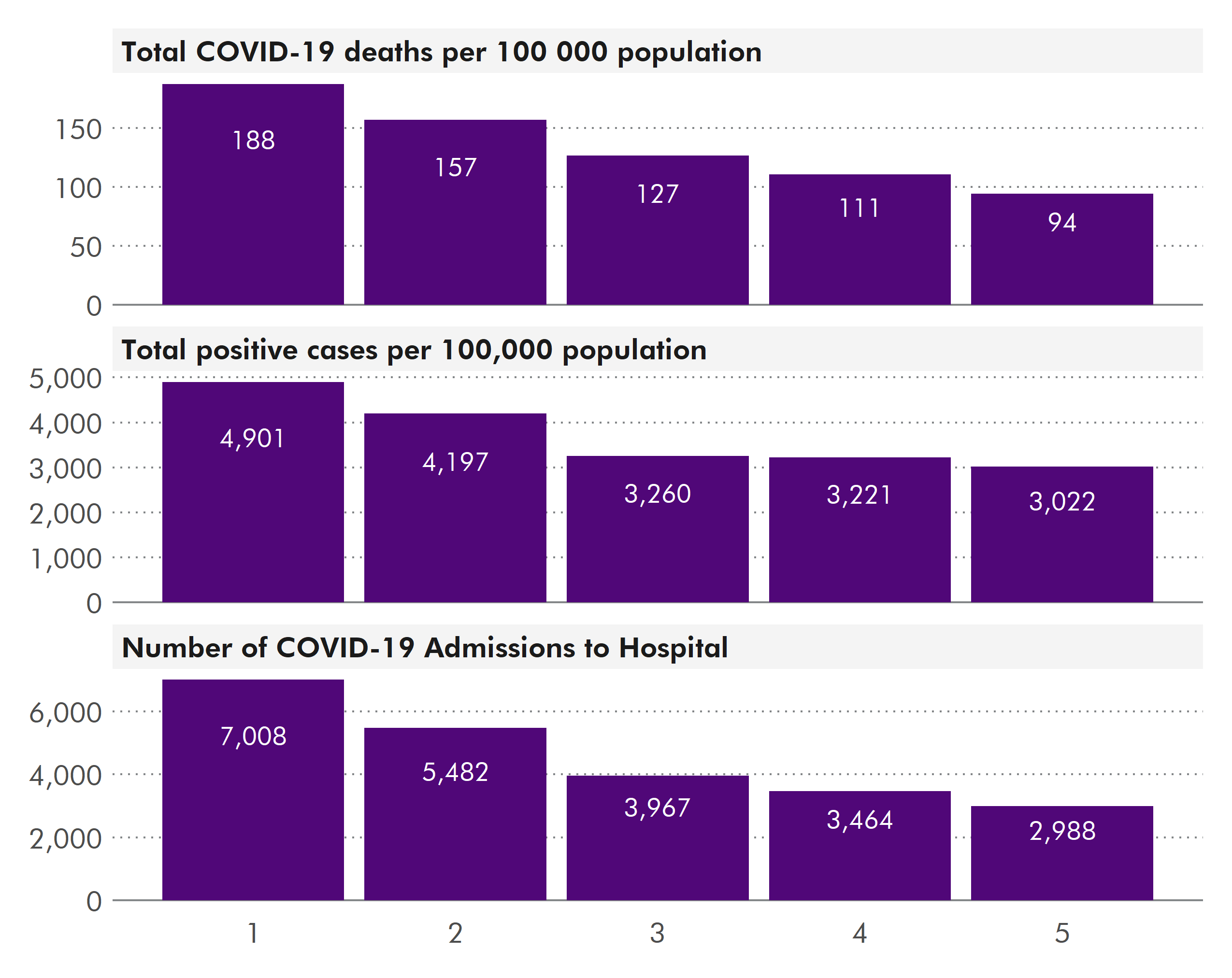
The number of people hospitalised who live in the most deprived areas is much greater than those who live in the least deprived. Deaths have followed a similar pattern; the death rate from COVID-19 in the most deprived fifth of areas has been double the rate in the least deprived fifth. Research showed that those from the most deprived areas were more likely to die in hospital when admitted to intensive care than those from the least deprived areas.1
There are many connected factors which contribute to this greater risk of direct health harms in the most deprived parts of society. People living in deprived areas are more likely to have poor health to start with, so are more likely to suffer greater health harms from the disease. They are less likely to be able to work from home and so are more exposed to the disease, and are more likely to live in poor quality housing which limits their ability to self isolate effectively.
Obesity is an important risk factor in COVID-19, and people with obesity are more likely to live in deprived areas. Obese people are more likely to be admitted to hospital with COVID-19, and are more likely to die from COVID-19 than those with a Body Mass Index in the healthy range.
Long COVID in Scotland
There is not much data available about the number of people experiencing long COVID symptoms in Scotland, but it is expected to be a significant proportion of COVID-19 patients. Since the spread of COVID-19 cases has not been even across society, then logically we expect there to be uneven numbers of long COVID sufferers too.
Long COVID is currently being treated through primary care like other chronic conditions. Groups of people who are less likely to access GP services could also be less likely to seek help with long COVID. These groups could end up suffering for longer than those able or willing to access help earlier, which could further increase the gap in health outcomes for people living in the least and most deprived areas.
Some research has shown that women are more likely to experience symptoms of long COVID, with one study finding that women under 60 years were twice as likely as men in the same age group to report symptoms.
Indirect health harms from COVID-19 and their uneven impact
Aside from the direct effects of COVID-19, the restrictions on people's lives, and the closure of services have created indirect health harms. This section will explore some of these harms, but due to the large number of impacts COVID-19 has had and is continuing to have on society and the economy, it is not an exhaustive summary. The extent of some of these indirect health harms may only become apparent in the years or decades to come.
There is an age divide in the impact of indirect health harms. The direct harms have overwhelmingly affected older people, but indirect harms have affected younger people more. Young people have suffered disruption to education through school, college and university closures. They are more likely than older people to have been made redundant, and more likely to be placed on furlough. The proportion of people under 25 claiming universal credit and work-related benefits rose significantly, and the number of graduate jobs advertised for university leavers fell by as much as 60%.
Impacts on healthcare services
From March 2020 onwards, a significant proportion of NHS services were affected by cancellations and closures. GP consultations moved to virtual platforms, and routine screening programmes were paused. Waiting times for routine appointments were longer than before the pandemic. The number of people dying whilst on waiting lists for treatment also increased.
Impacts on hospital admissions
The closure and restriction of routine NHS services to prioritise resources for COVID-19 had a large impact on waiting times. The number of people seen within six weeks for diagnostic tests and screening fell markedly in March 2020 (see figure 8), and is still below pre-pandemic levels. Screening uptake was lower pre-pandemic in the most deprived areas. With greater barriers to treatment and screening due to COVID-19 restrictions, the impact on the most deprived areas will be greater than more well-off areas.
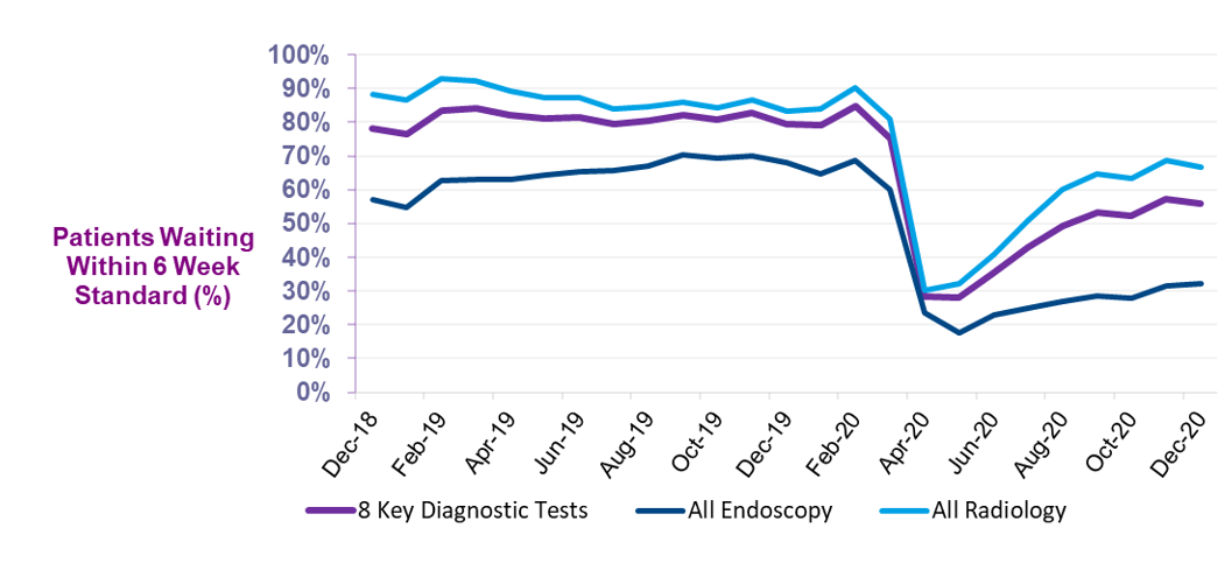
During the second wave of infection, similar trends have emerged, with planned operations falling by 35% in December 2020 compared to previous years.
For unplanned hospital admissions the trends have been similar.
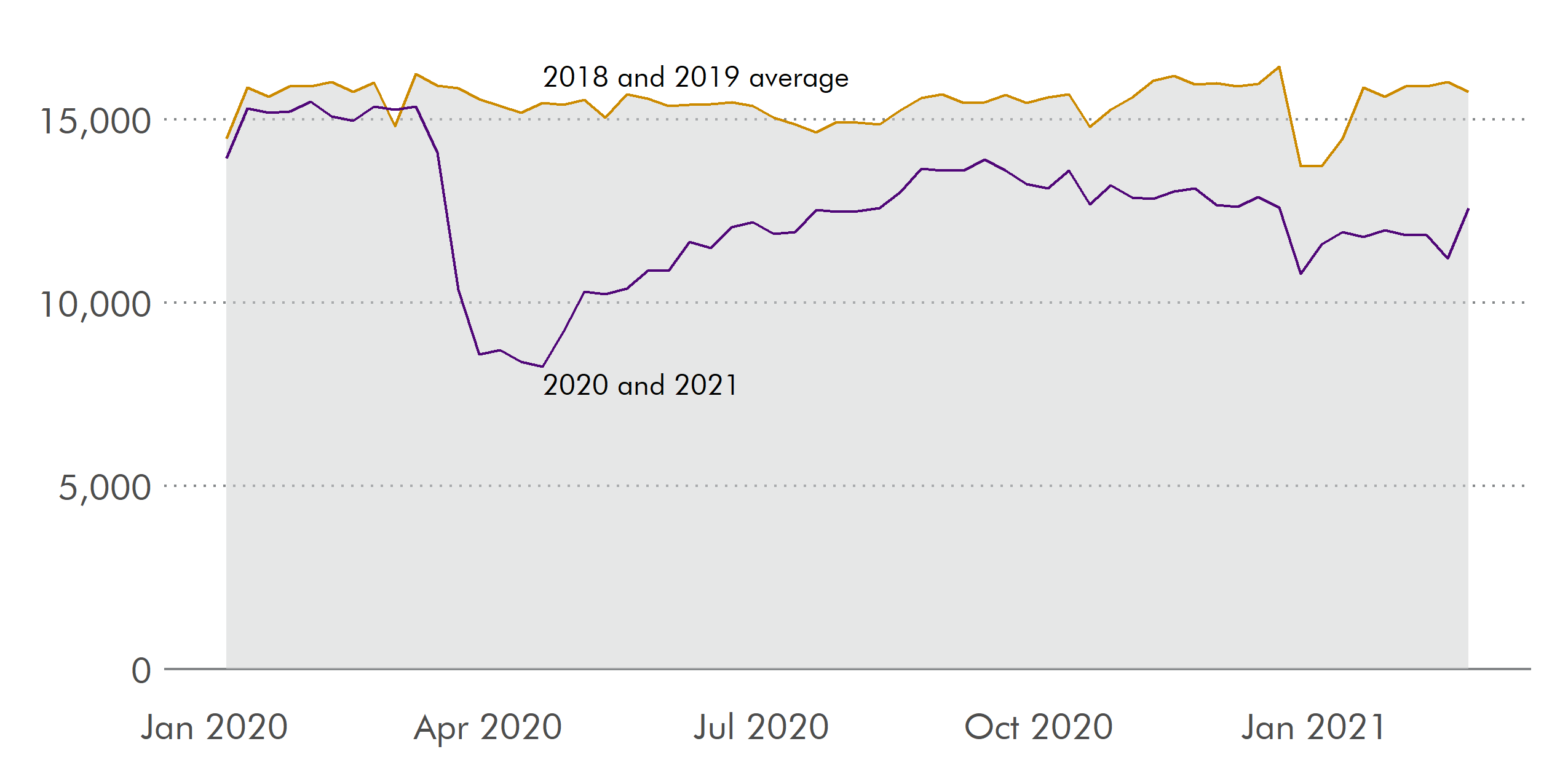
Attendance at Accident and Emergency Departments fell during March 2020 and are still below pre-pandemic levels. Public Health Scotland say this is due to reluctance for people to attend hospital from fear of 'overwhelming the NHS', worries about catching or spreading the virus, and being unaware that services are still open. Lower mobility in society from closure of services resulted in fewer accidents (for example from road accidents) and non-COVID-19 infections were less likely to spread. Greater numbers of people died at home, particularly from respiratory diseases, heart conditions and cancer. This is not a bad thing for all people, but those in the most deprived areas are more likely to live in poor quality housing with less space, poor heating and poor ventilation. The level of care and support available for these people in the home in this context may well have been worse than in hospital, and worse than the least deprived.
Impacts on general practice and dentistry
Along with other sections of the health service, GP surgeries adapted and restricted services in response to COVID-19. These changes affected all service users, but people in some groups were affected more. The large shift to online consultations will have excluded those without access to the internet or devices to access it. This particularly affects vulnerable groups such as rough sleepers and asylum seekers, and the elderly. Age UK issued a statement outlining how telephone and online consultations excluded many older people, and were likely to exacerbate inequalities in access to services.
Changes to GP services affected those in deprived areas more than affluent areas. A survey of 'deep end' GP practices (those serving the most deprived areas in Scotland) reported that while in general they had coped during the first wave of COVID-19 infections, pre-existing health inequalities were being exacerbated. People whose first language is not English struggled more with online and telephone appointments, and arranging translators became more difficult. Concerns were raised about vulnerable children who had their support services withdrawn, which included in-person appointments in GP surgeries. Mental health problems were increasing and caused constraints on capacity particularly for practices in the most deprived areas.1
Dental services were restricted in March 2020. Concerns have been raised by the General Dental Council about the uneven impact on oral health inequalities of the pandemic. Survey data indicated that because of the pandemic, people of ethnic minority backgrounds, and those with physical or mental health conditions, were less likely to access dental care. Both children and adults in the most deprived areas in Scotland are more likely to have poorer dental health, and are therefore likely to feel a greater impact of closure of services.
Impacts on cancer screening and care
Before the pandemic, inequalities existed in the incidence of cancer morbidity and mortality between people living in the most and least deprived areas in Scotland. For most cancers, people living in the most deprived areas are more likely to be diagnosed, and suffer worse outcomes.1 Cancer incidence was 32% higher and mortality rates were 74% higher in the most deprived areas compared to the least deprived.
Due to these pre-existing inequalities, any restrictions to care and screening are more likely to affect the poorest in society, exacerbating inequalities.
In March 2020, routine screenings for a range of cancers were paused. This was restarted as part of the NHS remobilisation during summer 2020. During the pause, a large number of cancer detections were missed: between March and June 2020, there were 4,000 fewer cancer diagnoses than expected. By the end of 2020, 7,000 fewer people had been diagnosed with cancer than in 2019.
Pre-existing inequalities mean that it is likely that more of these missed cancer diagnoses will be in the most deprived areas. Cancer charities have reported that they are seeing more cancer patients in later stages of the disease. Generally survival rates are lower the later the cancer is detected.
The Scottish Government has published a Cancer Recovery Plan, and has evaluated the impact on equalities of this plan.
Despite the resumption of screening, the poorest groups in society are less likely to access screening services. Due to the impact of the pandemic on income, employment and mental health, more people may be living in poverty than before COVID-19. Because of the links between poverty and likelihood of late cancer diagnosis and survival, this could exacerbate inequalities in cancer treatment and survival.
National Records of Scotland data shows that more people are dying at home from cancer now than before the pandemic. Macmillan Cancer Support said that for the more well off, this may give better care due to having more space, easier presence of family members and warmer and well-ventilated houses. However, for some people, inequalities in housing quality and fuel poverty may mean that these groups are suffering more than they would have done if they were in hospital.2
Mental health impacts
Research has shown that COVID-19, and restrictions to control it have had huge impacts on people's mental health in Scotland.
Poor mental health is strongly associated with social and economic circumstances, including living in poverty, low-quality work, unemployment and housing.1 Before the pandemic, mental health was worst in the most deprived areas. Mental health services were becoming stretched due to greater demand, which resulted in longer waiting times for treatment. Due to the clear social gradient in mental health, any restrictions on mental health services were likely to have a greater impact on those living in more deprived areas, younger people, people living with a disability and ethnic minorities.2
Effects of the pandemic response on mental health
Mental health harms can be also be caused by indirect effects of the virus such as:
isolation and loneliness due to lockdown
income and job worries
fear of catching the disease
worries about childcare and caring responsibilities
fear of eviction or home repossession
disruption to education
higher levels of stress in cramped or confined housing.
Research by the Institute for Fiscal Studies showed that mental health had on average worsened as a result of the pandemic, and that the impact had been felt most by women and young adults, groups already more likely to experience poor mental health.
The Mental Health Foundation found that in Scotland, the impacts on mental health of the pandemic were affecting certain groups more, such as those from deprived areas, women, young adults and people with low incomes. The Scottish Government is monitoring mental health impacts from the pandemic, and found that women and young people have been disproportionately affected. A survey by Public Health Scotland found that children have seen significant mental health impacts from closure of schools and nurseries, inability to see friends, problems arising from home schooling and care, and changes to activity levels.
People living with physical disabilities and long-term illness were already more likely to suffer from common mental health problems such as depression and anxiety, and are more likely to live alone, compounding feelings of isolation and loneliness.
Effects of COVID-19 infection and treatment on mental health
People who have suffered COVID-19 infection are more likely to experience mental health harms. Long COVID is associated with reductions in mental wellbeing. Those who were admitted to hospital and underwent invasive treatments are more likely to experience Post Traumatic Stress Disorder, and psychiatric disorders such as anxiety and depression.1 Given that the most deprived, disabled people and ethnic minorities are more likely to suffer serious COVID-19 illness, this means that the mental health impacts associated with infection will have greater impact on them too.
In March 2021, the Scottish Government told the Scottish Parliament Health and Sport Committee that they would be establishing a specialist network of mental health clinicians to support people hospitalised because of COVID-19. All people hospitalised will be approached for mental health screening, and the government expects to treat around 3,000 people.
Effects of COVID-19 restrictions on mental health services
Restrictions on in-person appointments and closure of support services have had a large impact on mental health services in Scotland. Given the gradients in mental health across society, those already more vulnerable are bearing the brunt of the changes to support.
Waiting times for CAMHS (Child and Adolescent Mental Health Services) have increased during the pandemic. With those from deprived areas more likely to need support, this will increase inequalities.
GP surgeries serving deprived communities have reported an increase in patients seeking help with mental health problems. There has also been an increase in people phoning 999 for help with mental health issues.
Physical health impacts
Aside from the direct physical health harms of COVID-19, the range of indirect health harms to physical health is wide ranging. These harms are not evenly distributed across society. The restrictions placed on society are the main driver of these indirect health harms. Some people have argued that the restrictions are having a worse impact than the virus itself, but this neglects to account for behaviour change which would have occurred regardless of restrictions, such as reducing social contact and working from home. Either way, indirect health harms are having a large, and uneven, impact on society.
Excess deaths are defined as deaths above the long term average. COVID-19 has resulted in a large increase in excess deaths, but not all of these were directly caused by the disease. Analysis by Public Health Scotland found that while most excess deaths were caused by COVID-19, 18% of excess deaths had other causes, and that these were not distributed equally across society. For some causes of death existing inequalities were widened, such as for Alzheimer's, dementia, and deaths from 'external and ill-defined causes'. It is thought that some of these non-COVID excess deaths can be explained by undiagnosed COVID-19 infection. However, Public Health Scotland say some of them will be caused by reduced use of health services by those who need them and unintended consequences of the restrictions. Longer term, excess deaths are likely to be caused by indirect harms from the virus. For example, unemployment has risen considerably and is associated with increases in mortality.1 Increased educational inequalities are likely to increase inequalities in life expectancy.2
Lockdown measures increased the risk of domestic and family violence through confinement, reduction in access to support services and problems with childcare or caring responsibilities. Women and girls are the most likely to experience this sort of violence. The Scottish Government found that referrals to support increased as a result of lockdown measures, and it increased support to cater for higher demand. Women from deprived areas and younger women are more likely to experience domestic abuse.
People with long term limiting physical and mental health conditions are especially impacted by restrictions on social contact and changes to support services. Service disruption has meant some disabled people have seen their existing health conditions deteriorate. Those who have become reliant on food aid may have found it does not accommodate their dietary needs.3
People's diets have been affected by COVID-19, and this will have an effect on their physical health. Research by Together Scotland found that charities were providing more help to greater numbers of people who could no longer access food. The Trussell Trust, who run food banks, said that food bank usage increased by 89% in April 2020, and the Independent Food Aid Network reported a 246% increase in food parcels given out in April 2020 compared to April 2019. The Glasgow Centre for Population Health outlined how food insecurity had been increased markedly by the pandemic. Children who normally received free school meals were unable to do so whilst schools were closed. Vouchers, cash payments and food boxes were issued by local authorities in lieu of free school meals, but these may have been missed by some people.
Exercise and its effects on physical and mental health have been affected by the pandemic. With leisure centres and swimming pools closed, exercise was mainly restricted to either in the home or garden, or nearby parks and countryside. Access to greenspace has well documented positive influence on mental health, so these inequalities in access contribute to wider mental and physical health harms. The most deprived areas have worse access to, and are less likely to access, greenspace. People in the most deprived areas, and those with ethnic minority backgrounds are less likely to have access to a private garden. Lockdown has been shown to have reduced time spent in greenspaces, and exacerbated inequalities in access to them.4
Changes to travel patterns will have an impact on physical health, and inequality. Road traffic has an adverse impact on health through air pollution, injuries and physical inactivity. These impacts are more likely to affect those in more deprived areas, those on low incomes and those with pre-existing health conditions. After a large reduction in car use in the initial lockdown, traffic increased to near pre-pandemic levels, while journeys on public transport remained very low. Public Health Scotland looked at the impacts of these changes to travel patterns and assessed their impacts on health inequalities. If these changes result in a long term increase in the use of private cars, this will increase the adverse effects on health, and increase transport poverty. Changes to the physical environment to permit social distancing have impacted disabled people, particularly in access to public transport. A poll by Disability Equality Scotland found disabled people were refused access to public transport, and were finding social distancing difficult or impossible on pavements and at crossings.
The Scottish Government's response to COVID-19
The Scottish Government used a variety of legislation to respond to the pandemic. An explanation of the emergency powers and legislation can be found in the SPICe blog 'COVID-19 emergency powers: a short explainer'.
The Scottish Government has used its four harms framework to assess the impact of COVID-19 restrictions on inequality.
There has been a large financial cost of responding to the pandemic. The Scottish Government has spent or committed to spending around £3.2 billion for health measures in response to COVID-19.1 The impact of the 2021-2022 budget on inequalities was assessed by the Scottish Government. This summary sets out how people with protected characteristics will be affected by the budget this year.
How have the impacts of COVID-19 restrictions on health inequality been assessed?
Because of the urgency of legislative requirements during the pandemic, the Scottish Government has not been able to assess the impact on inequalities as much as usual. However, some Equalities Impact Assessments were carried out.
An Equality Impact Assessment was carried out in March 2020 for the Coronavirus (Scotland) Bill. This looked at the impact of the strict early restrictions and closure of services on people from protected characteristics. Because of the urgent nature of the legislation, consultation with affected groups was very limited.
A Health Impact Assessment was carried out for the impact that physical distancing measures would have on health and inequalities.
Some consideration was given to the impact of reintroduction of some restrictions in summer 2020 as cases began to rise in some areas. These were set out in an Equality Impact Assessment.
In July 2020, the Scottish Government published a Fairer Scotland equalities impact assessment of its strategy for the first easing of restrictions. It highlighted some of the issues faced by different groups in society during the first wave of the pandemic. It described some of the impacts on equalities, and how the gradual easing of restrictions through summer 2020 would attempt to mitigate some of these impacts, such as through allowing more social interaction, re-opening schools and early-years childcare and remobilising routine parts of the NHS. In December, another equalities impact assessment was published covering the later phases of easing restrictions. However, many of the mitigations described (for example social interactions and schools re-opening) were reversed during autumn and winter 2020 as restrictions were tightened again.
The Scottish Parliament Equalities and Human Rights Committee held an inquiry into the impact of COVID-19 on equalities in Scotland, which included looking at the impacts of the restrictions as well as the disease itself. Evidence to the enquiry was provided by a wide variety of organisations including charities, third sector groups and religious organisations. Many witnesses highlighted the importance of ensuring that emergency legislation was time-limited and only used for as long as necessary, particularly to avoid impacting the most deprived and groups with protected characteristics.
In May 2020, the First Minister said that there would be a public inquiry into the Scottish Government's handling of the COVID-19 crisis. This was particularly in response to criticism of the discharge of COVID-19 patients into care homes. This practice could have exacerbated inequalities by age by exposing an already more vulnerable group to COVID-19. As of March 2021, there is no update on any inquiry.
On the 4 March 2021 the COVID-19 Committee heard evidence from The Law Society of Scotland and other stakeholders on the impact of the emergency legislation. The Law Society questioned the need for extending emergency legislation for some elements of the COVID-19 response due to its unequal impact across society.
The vaccination programme
In Scotland, the first COVID-19 vaccines were given on 8 December 2020. There are two vaccines currently being administered in Scotland, with a third due to begin being delivered in April 2021. Restrictions on the supply of the vaccine, and the logistics required to immunise large numbers of people, mean that who is given the vaccine has to be prioritised.
Rollout of the vaccination programme is progressing fast.
A preliminary study has shown a large decrease in hospital admissions in age groups who have received the vaccine. Research has also shown a reduction in transmission of the virus in health workers who were vaccinated.
Vaccine prioritisation - a tool to address inequalities?
The way that the vaccine rollout is prioritised is set out in guidance issued by the Joint Committee on Vaccination and Immunisation (JCVI), which is a group of experts that advises government and health services. They published their first set of guidance for COVID-19 vaccine prioritisation in December 2020. This guidance covered those over 50 years and those who were clinically vulnerable. Further guidance was published on 26 February 2021, for phase 2 of the programme which includes those aged 18-49 years.
The JCVI guidance prioritises vaccination by age and clinical vulnerability. It also prioritises health and social care workers. This group are not necessarily at a greater risk of serious illness or death from COVID-19, but their high levels of contact with vulnerable people means they are a high priority for vaccination. This prioritisation is based on the number of lives expected to be saved. JCVI modelling indicates that the groups in this prioritisation represent 99% of preventable COVID-19 mortality.
The JCVI did assess its prioritisation's impact on health inequalities. It said it was likely that some health inequalities would not be addressed, as some groups who are more likely to get ill from COVID-19 were not being prioritised, such as the most deprived or those of ethnic minority background. Also, with the exception of health and care workers, vaccination would not be prioritised by occupation. The reasons given for this are that age is the single biggest factor in COVID-19 risk. The logistics of delivering vaccines by occupation or ethnicity would be difficult. Not all the necessary data is kept on GP systems and it could delay the overall rollout if systems had to be developed to capture these groups first.
It is worth noting that those in the most deprived areas on average do not live as long as those in the least deprived areas, so are more likely to be younger, and therefore less likely to be eligible for vaccination.
There have been calls to prioritise ethnic minorities and key worker occupations in the vaccine rollout to address inequalities, especially in the under 50 year old group. These groups are at greater risk than the population average.
There is evidence in England that vaccine uptake so far has been lower amongst some ethnic minority groups and the most deprived. Research conducted in health and social care staff in England found that those from an ethnic minority background were less likely to have received a COVID-19 vaccine than their white colleagues.1
A survey conducted by the Royal Society of Public Health found that people from ethnic minority backgrounds were much less likely than white people to accept the vaccine. This could be due to cultural or religious reasons and suspicion of authority, and difficulties in access to healthcare. If this disparity between different groups is maintained as the vaccine programme continues, then this will exacerbate existing inequalities. Concerns have been raised that COVID-19 may become a 'disease of the poor' if vaccine uptake is not increased in marginalised groups.
Advertising campaigns and tailored communications have been planned in England to try increase vaccine uptake in communities where vaccine hesitancy has been greatest.
Currently, data on the ethnicity of those receiving vaccines is not available in Scotland. In a letter from the Chief Medical Officer for Scotland on 9 March 2021, it was noted that in the under 50 age group, some groups including men, people of ethnic minority background, and those in deprived areas were more likely to be hospitalised. To make sure uptake was as high as possible in these areas, those delivering the vaccine were advised to use an inclusive approach and make use of local expertise, and clear communication and outreach activities. The Scottish Government have worked with organisations representing seldom heard groups, such as BEMIS, to encourage confidence in the vaccine in groups who have been disproportionately affected by COVID-19.
Recovering from the pandemic
At the time of writing, the COVID-19 pandemic is still ongoing. Once it is over, its effects will be felt for a long time. It is still not known how prolonged long COVID symptoms may be, and the impacts on education, the economy, employment, businesses and mental health may affect people for decades.
Addressing health inequalities during the recovery
The recovery from COVID-19 has received some coverage in the media and from politicians, with much of this focusing on 'building back better' and ensuring a 'green recovery'. Some of this discussion has involved addressing poverty and inequality as society recovers from the pandemic, whilst addressing climate change.
The Institute of Health Equity who published 'Marmot Report - 10 years on' realised that their report, released in February 2020, was quickly going out of date due to the upheaval caused by COVID-19. In response, they published Build Back Fairer: the COVID-19 Marmot Review in December 2020. This report outlined how the recovery from COVID-19 could address health inequalities, chiefly through addressing the fundamental causes.
The Scottish Government set up a Social Renewal Advisory Board to make recommendations on how to renew Scotland in the recovery from COVID-19. It published its report in January 2021. The recommendations centred on addressing the fundamental causes of inequality, such as providing a guarantee of basic services, housing and income which is enough for people to live healthy happy lives.
The NHS Remobilisation Plan was designed to focus on supporting those most vulnerable in society, and mitigate health inequalities through ensuring services were proportionate to need. The Scottish Government's Mental Health Transition and Recovery Plan sets out how it will prioritise addressing individual and structural inequalities.
The Scottish Parliament COVID-19 Committee convened a Citizen's Panel composed of a group of people broadly representative of the Scottish population to look at the Scottish Government's response to COVID-19. One of the recommendations in the final report was to focus efforts after the pandemic on a 'Green Recovery'.
The Mental Health Foundation produced a report outlining how best to address mental health as we recover from the pandemic. Their recommendations include making a 'Wellbeing Budget' to deal with poverty, and introducing a 'Mental Health Guarantee' that would mean that people seeking help are referred to appropriate support within 6 weeks.
In 2019, the Nuffield Foundation commissioned an expert review into inequalities, which will report in 2023. In January 2021, it published an interim 'New Year's Message' outlining how the pandemic has had an uneven impact on society and has worsened existing inequalities. It outlined steps which should be taken by the Government to mitigate these impacts and help the recovery from COVID-19. These include targeted support for children and young people, better recognition of the difficulties faced by self-employed people and addressing the multiple social and economic causes of poor health.
The Scottish Government established a Citizen's Assembly in 2019 to address questions about the future of Scotland. The remit of the assembly predated the COVID-19 pandemic, but in the recommendations for Scotland's future, they said a green and fair recovery should be a priority.
Health inequalities in a future Scotland
Health inequalities were bad in Scotland before the pandemic hit, and evidence and data to date shows that COVID-19 has made them worse. There have been a wide range of impacts to people's physical and mental health through the direct health harms from COVID-19, and indirect effects of COVID-19 restrictions. Research has shown that these harms have not been distributed equally across society. Older people, disabled people, people from ethnic minority backgrounds and other vulnerable groups have seen greater impacts from both direct and indirect health harms.
Younger people have avoided many of the direct health harms, but have been significantly impacted by the restrictions and associated impacts on the economy, education and employment.
The effects of COVID-19 will continue to be felt for a long time, regardless of the success or otherwise of the vaccination programme globally. The COVID-19 recovery potentially gives an opportunity to rebuild society and the economy in a way that addresses inequality. The extent to which any recovery is "fair" and "green" will likely be a major focus for the Parliament in Session 6.