The Health and Care (Staffing)(Scotland) Bill
The Scottish Government introduced the Health and Care (Staffing)Scotland Bill in the Parliament on 23 May 2018. It proposes a basis for appropriate and safe staffing across all health and social care settings underpinned by a set of guiding principles. Its purpose is to place the use of existing staff planning methods in health settings on a statutory footing.This briefing considers the background and the main provisions of the Bill.
Executive Summary
The purpose of the Bill is to place on a statutory footing the use of an existing, but enhanced, workforce planning method (tools). The use of the 'common staffing method' will be required in certain specified health settings. The Bill also enables the development and validation of appropriate staff planning methods for other health and social care settings, initially for care homes. The aim is to ensure safe and appropriate staffing levels using clear, evidence-based methodologies. The workforce planning tools referred to in the Bill have been mandated for use by all territorial health boards by the Scottish Government since 2013.
Workforce planning is conducted at both a national and a local (health board/social care provider) level. Staffing requirements for health settings and social care settings are assessed and monitored in a variety of ways, and are the responsibility of different bodies.
The Scottish Government has overall responsibility for national health service workforce planning. The Scottish Government decide on the numbers of most health service staff entering training, but not for those entering the allied health professions. The Government also has oversight of recruitment into the health service, and an overview of where pressures are across the professions in terms of availability of qualified staff. Health boards conduct their own workforce or workload planning according to the needs of their own populations, local context and demography. They do this in the context of government-directed policy.
From 2004, a set of 12 workforce planning tools for nursing and midwifery were developed, as part of the methodology Health Boards use to decide, on an annual basis, the staff establishmenti for most nursing settings. The tools are based on an average workload for each specialty across Scotland, and are supplemented, in a triangulated approach, by considering the specifics of local context, quality measures and professional judgement. Health Boards were instructed to use the tools and methodology from 2013.
The social care sector is very disparate in terms of service delivery, governance and structures. Social care for adults, for example, covers large independent providers based outwith Scotland, running 'care at home' services and care homes, to those run by local authorities, housing associations or a single, family run care home or care at home business. There is no obvious parallel with health services or health boards.
The Bill is in four parts. Part 1 of the Bill sets out the guiding principles for health and care staffing. The first principle is that staffing is in place to provide 'safe and high quality services'. It is important to note that this part spans the health and care services landscape, and all the staff within it, and refers to all health settings and all care settings registered by the Care Inspectorate. The intention is to create a coherent legislative framework across sectors through the application of these guiding principles.
Part 2 of the Bill seeks to amend Section 12I of the National Health Service (Scotland) Act 1978 1These provisions extend and provide more detail to the duties of health boards concerning staff governance and workforce planning. Under the 1978 Act it is the duty of health boards to 'put and keep in place arrangements for the purposes of:
(a) improving the management of the officers employed by it;
(b) monitoring such management; and
(c) workforce planning.'
The amendments to the 1978 Act, contained in Part 2, Sections 12IB - 12ID provides a detailed description of the 'common staffing method'.
Part 3 of the Bill would enable the social care sector to build on the existing mechanisms contained in Regulation 15 of the Social Care and Social Work Improvement Scotland (Requirements for Care Services) Regulations 2011 2 . It also places the general 'appropriate staffing' duty on care service providers (Section 6), giving them an equivalent responsibility to Health Boards. It amends the Public Service Reform (Scotland) Act 2010, Section 82, to provide that the Care Inspectorate may lead the development and validation of methodologies and workload and workforce planning tools in collaboration with the sector to be used in 'care home for adults' settings where necessary. This would apply to care homes for adults over the age of 18, not just care homes for older people.3
It is not clear what will happen if a health board or social care provider does not meet the duties set out in the Bill. Health Boards and social care providers might not be able, because of vacancies or local or national unavailability of staff, to fulfil the establishment that the board or organisation has deemed to be appropriate and necessary to provide high quality, safe care.
The resourcing associated with the Bill only covers the direct costs - the development and implementation of tools and methodologies and training of staff. It acknowledges that there might be a consequential impact on the demand for staff, but that this will be the responsibility of health boards to manage, and the Scottish Government do not see that there will be an overall increase in costs incurred by health boards.
Introduction
In its Programme for Government 2017/18 1, the Scottish Government committed to introduce a safe staffing bill during the 2017/18 Parliamentary year to 'deliver on the commitment to enshrine in law the principles of safe staffing in the NHS, starting with the nursing and midwifery workforce planning tools'.
The Health and Care (Staffing) (Scotland) Bill 2(the Bill) seeks to provide a statutory basis for appropriate staffing in health and care settings to enable safe and high quality care.
The Policy Memorandum 3 to the Bill states that it is already 'the duty of every Health Board to workforce plan and to provide high quality care.' That care should already be appropriate for the care requirements of patients is therefore already extant. The Bill makes this an explicit duty and introduces the word 'safe' in relation to services, but does not define what this means. However, in its consultation document, the Scottish Government used the following definition for 'safe':
Safe – There will be no avoidable injury or harm to people from healthcare, and an appropriate, clean and safe environment will be provided for the delivery of healthcare services at all time.
4
This definition was taken from The Healthcare Quality Strategy for NHS Scotland, published in May 2010. 5
The Bill proposes that existing workforce tools, mandated for use by all territorial health boards by the Scottish Government since 2013 will be put on a statutory footing. However,
The mandate did not include the requirement to apply the results, evidence analysis, or risk assess the impact that the application of the tools and triangulation process has had on decisions relating to staffing levels, assurance that there is safe and effective staffing or development of workforce plans.
Scottish Government. (2017). Consultation Document. Retrieved from https://www.gov.scot/Resource/0051/00516603.pdf [accessed August 2018]
The Bill seeks to make it more explicit that the analysis resulting from the application of the tools, in addition to better staff involvement, risk-based decision making and senior clinical involvement, is used to ensure better decision-making in relation to staffing across health settings.
The Scottish Government undertook two consultations on the proposals in 2017 7and 2018. 8 The first consultation proposed only that the existing nursing and midwifery tools, which are used to establish permanent staffing requirements, be made statutory, and that their application be monitored and reported on. The consultation also proposed to extend this approach to establish staffing levels for other staff groups. An independent analysis of the consultation responses was published 9. While the consultation questions covered health and social care, the proposals were that the legislation should only apply where validated tools were available, in health care settings.
Some respondents to the first consultation considered it unnecessary to extend legislation to social care settings because statutory frameworks are currently in place to ensure safe staffing in social care. That said, respondents did think that the legislation should take full account of health and social care integration. The proposals were deemed too narrow and there was a fear that focus and resource would be directed to those groups - nurses and midwives - explicitly identified in the legislation. Additionally, the proposals did not consider safe staffing in a system-wide way; in the context of national workforce planning and training numbers, nor in the context of current workforce challenges.
The subsequent consultation 8 on proposals which took account of earlier responses and focused on how the legislative framework would cohere across health and social care ran for four weeks in February 2018. Respondents felt that any new methodologies should work across health and social care, that there should be flexibility in how new tools were developed, used and reviewed, and that there should be recognition of the challenges faced across sectors in recruiting and retaining staff. Some respondents remained unsupportive of the inclusion of social care.
More detail about the provisions of the Bill are given below, but the above provides some explanation of why the main substance of the Bill pivots on existing nursing and midwifery workforce planning methods, as set out in the Bill, that are applied mainly in acute settings to establish a number and skill mix for permanent workforce needed. There are, however, two tools that cover some community nursing provision, and the maternity tool covers both hospital and community midwifery settings.
Workforce Planning in Health and Care Settings
Workforce planning is conducted at a national and a local (health board/social care provider) level. i Staffing requirements for health settings and social care settings are assessed and monitored in a variety of ways, and are the responsibility of different bodies.
The Scottish Government has overall responsibility for national health service workforce planning. The Scottish Government decide on the numbers of most health service staff entering training, but not for those entering the allied health professions. The Government also has oversight of recruitment into the health service, and an overview of where pressures are across the professions in terms of availability of qualified staff. Health boards conduct their own workforce or workload planning according to the needs of their own populations, local context and demography. They do this in the context of government-directed policy.
Health Boards conduct their workforce and workload planning according to their duties under 12H and 12I of the National Health Service (Scotland) Act 1978 1 (the 1978 Act) and are responsible for ensuring appropriate staffing on a day to day basis. Social care staffing is arguably far more complex given the range of settings involved and the range of providers of social care. It is the Care Inspectorate that oversees the safety and quality of care services, and their oversight includes an assessment about whether staffing is appropriate in any given setting. The process of workforce planning in the social care sector is less well-developed nationally because of its very different history and structure.
In the context of the integration of health and social care services into health and social care partnerships (Integration authorities, Integration Joint Boards), it is understood that workforce planning for services will increasingly cross health board and local authority boundaries, via the integration authorities. The Scottish Government has published a National Health and Social Care Workforce Plan in three parts, covering NHS Scotland (Part 1) 2social care (Part 2) 3and primary care (Part 3) 4
Inasmuch as the Bill is concerned with workforce planning issues, it is focused primarily on local workforce planning by health boards, in almost all of the settings (community and acute care) where nurses and midwives are found.
It is hoped that, with more robust and consistent workforce planning locally, and with better availability of data, health boards will be able to assess staffing need more effectively which will, in turn, inform national workforce planning. However, there is nothing in the Bill about the collation or reporting of workforce projection data. The current tools are not designed to project need beyond the current configuration of a ward or service, so it is not clear how this aspiration to link local to national workforce planning would be achieved in relation to this legislation.
In its submission, Audit Scotland 5cited its report 'NHS Workforce Planning, the clinical workforce in secondary care, July 2017'6. One of two recommendations in the report that related directly to safe staffing levels stated that 'NHS Boards should fully cost the workforce changes needed to meet policy directives, such as a shift to community-based care, proposed elective centres, safe staffing levels and more regional working.' Further, a number of written submissions (Scotland Excel, Unison, Glasgow City Health and Social Care Partnership, Marie Curie) argue that the Bill is centred on a largely mechanistic solution to workforce planning, which will not lend itself to the flexibility required of services to meet an outcomes-focused agenda.
Some healthcare staffing statistics
According to Part 1 of the National Health and Social Care Workforce Plan 2 there are just under 100,000 staff working within the NHS in Scotland (as at 31 March 2017, and not including administrative staff): 60,000 nurses and midwives (WTEii), 12,000 hospital doctors, 11,500 allied health professionals (such as occupational therapists, radiographers, physiotherapists etc), 5,500 healthcare scientists, 5,000 GPs (headcount not WTE) and 4,000 others such as pharmacists, who are outwith the above categories.
The Bill's scope does not cover national workforce planning. Its provisions will not contribute to ensuring that the overall demand for staff of the NHS and Social care sectors will be met. As discussed above, Audit Scotland's view is that there have been no proper assessments made, by either the Government or Health Boards, about the staffing or financial resources required to fulfil the demands of recent and emerging policy directives.
Further, the 'common staffing method'iii detailed in the Bill (12IB), is related only to the required establishmentiv of staff, not the daily and real-time assessment of whether there is appropriate medical and nursing staff in place in community and acute care settings, which is connected with the daily rostering of staff.
Why was better workforce planning required?
Audit Scotland published 'Planned Ward Nursing - Legacy or Design' in 2002, which recommended an approach to workforce planning that included a consideration of quality measures. Following on from this, in 2004 The Scottish Executive's Nursing and Midwifery Workload and Workforce Planning Project produced 20 recommendations to inform the formalisation and rationalisation of nursing and midwifery roles and workload. Underpinning this was improved outcomes for patients, and this aim has remained a constant driver of policy since.
During the course of the development of the tools, and more recently, two major reports linked to patient safety and systemic health service failure were published. The Vale of Leven Inquiry into deaths due to C.Diff infection (2009 - 2014) and the Francis Report (2013) on failures in Mid Staffordshire Hospitals Trust. While these two inquiries were not directly related to the development of the workforce planning project, they contributed significantly to government and health boards' focus on areas such as:
infection control,
better communication between staff,
transparency and openness,
complaints processes,
patient focus and
better reporting structures
These are all reflected in health board practices and care quality indicators today.
Additionally, the importance of encouraging to staff to raise issues of concern about patient safety was recognised in the Freedom to Speak Up Report in 2104.
What did the Workload and Workforce Planning Project Produce?
The work of the Nursing and Midwifery Workload and Workforce Planning Programme (NMWWPP) 1from 2004 onwards, led to the development, over a number of years, of a set of 12 workforce planning tools for nursing and midwifery, and a method for health boards to decide on an annual basis what the establishmenti should be for each nursing setting. The tools are based on an average workload for each specialty across Scotland, and are supplemented, in a triangulated approach by considering the specifics of local context - for example, the age profile of staff, local recruitment challenges; quality indicators and professional judgement.
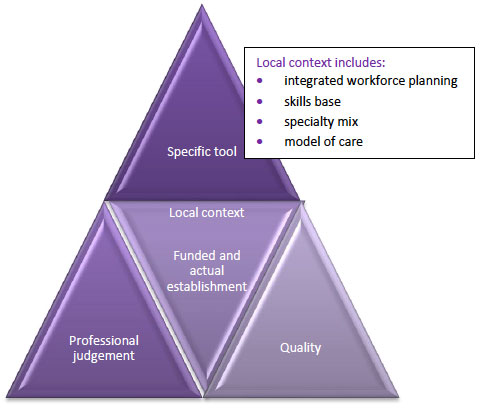
(p7 PM)2
Each tool is designed for a specific setting, as laid out in Section 12IC of the Bill, such as Adult Inpatient, Mental Health and Learning Disability and Paediatric Inpatient. The tools were developed over a number of years to support evidence-based decision making and risk management. The tools use statistical analysis to calculate the whole time equivalent (WTE) required for current workload. This evolved into a staffing method, intended for use across NHS Scotland, which seeks to use a method of triangulation to ensure appropriate staffing levels and comprises the tools themselves, professional judgement, indicators of quality care and a consideration of local context. Only the tool for emergency medicine is multi-disciplinary. This tool covers medical as well as nursing staff.
Two of the 12 tools are designed to be run on a daily basis: for Neonatal and Paediatric wards. However, the data is not examined daily, but collated at the end of the annual (or biannual) reporting period and analysed by the Board's workforce planning staff and senior nurse managers to inform their decisions on ward staffing establishments for the following year.
How do the tools work?
It is important to make the distinction between these tools, used for workforce planning, and analysed on an annual basis, and other software tools used daily by senior charge nurses and team leaders (eg. SafeCare or the Shelford Group's 'Safer Nursing Care Tool') to ensure that they have safe staffing levels on a day to day basis. The Bill does not cover the use of these daily processes except in the broadest terms in the guiding principles for health and care staffing, set out in Part 1 of the Bill. These guiding principles are 'that the main purpose of staffing for health and social care and care services is to provide safe and high-quality services', and that staffing should be arranged while:
(i) taking account of the particular needs, abilities, characteristics and circumstances of different service users,
(ii) respecting the dignity and rights of service users,
(iii) taking account of the views of staff and service users,
(iv) ensuring the wellbeing of staff,
(v) being open with staff and service users about decisions on staffing, and
(vi) allocating staff efficiently and effectively.
Scottish Parliament. (2018, May). Health and Care (Staffing)(Scotland) Bill. Retrieved from http://www.parliament.scot/parliamentarybusiness/Bills/108486.aspx [accessed August 2018]
Annual/Biannual workforce planning within Health Boards
The tools comprise a selection of questionnaire-type processes on a software platform, the Scottish Standard Time System (SSTS)i which is common to all health boards, and is also used for payroll and expenses services. Most of the tools are run on an annual (or biannual) calendar. This entails that every day for a two week period senior charge nurses and team leaders will run the tools, inputting the data as required by the software. Alongside each specialty tool, the 'professional judgement' tool is also run, and is one of the suite of 12 tools. The results are then analysed and considered alongside quality indicators, professional judgement (senior clinical advice) and certain local factors (health boards use a range of different and additional methods to supplement information derived from the tools) by senior management nursing staff. As a team these staff then decide the optimum staffing establishment for each nursing area across the health board ie each ward in each hospital or community nursing/midwifery setting. This information is shared with the wider senior management team where staffing requirements 'compete' with other board priorities for resources.
SPICe survey on use of the NMWWPP tools
The Scottish Parliament Information Centre has been informed that the tools have not been evaluated or significantly modified since they were created, and that no review has been carried out since 2015. Because no recent evaluation was available, a survey was distributed to nursing and midwifery staff at various levels who are responsible for using or completing the workforce planning tools. 195 responses were received from staff working in eight of the fourteen territorial health boards. Most of the staff c.125 were those who have responsibility for running the tools on an annual or more frequent basis, or who were involved more broadly in the Board's staff planning.
The purpose of the survey was to explore how consistently the tools are used, what training is provided, whether they are deemed fit for purpose, whether they are run at the recommended frequency, how long they take to run, what action was taken as a result of running the tools and how concerns might be raised. It also asked what other means and methods were used to ensure safe staffing levels. Further analysis can be found in separate documents. There is a Summary of the survey findings available. In addition, all of the narrative responses and most of the charts have been extracted to a word document to make all the anonymised results available. Below are some of the main observations from the survey
It was clear from some of the responses that staff were not clear about how the information was used after they had completed their tasks of inputting data and observations.
Many were unsure of how the tools contributed to ensuring that staffing was safe for patients.
around a third of respondents had not received training on how to use the tools, or had only received ad hoc training from a colleague. There was no consistency in how training was delivered.
Many respondents did not feel that their wards were staffed to provide safe and effective care and that, regardless of tools or methods, staffing was inadequate
A range of other methods (eg. SafeCare, Shelford, Risk assessment and staff 'huddles') were used by staff to try to ensure that their ward or area had adequate staff of the right skill mix on a day to day basis
Some respondents were explicit about problems with specific tools. For example, the Community Nursing Tool, the Midwifery Tool in community settings, the Mental Health and Learning Disability Tool were not helpful in community settings. The perioperative tool duplicated other methods and some tools were very time-consuming to carry out.
In response to a question about escalation of concerns, responses were mixed. There were a variety of ways that staff could raise concerns, on a day to day basis, but many felt that their concerns were not adequately addressed.
These few points do not do adequately cover the range and detail about the tools and safety in health settings provided in the responses. It is recommended that the Summary and Survey Report are also read.
Social Care Staffing
The social care sector is very disparate in terms of service delivery, governance and structures. Social care for adultsi covers large independent providers based outwith Scotland which run 'care at home' services and care homes, to those run by local authorities, housing associations, third sector organisations or individuals. There is no obvious parallel with health services or health boards. It should be noted that the Bill covers all services as listed in section 47(1) of the Public Services Reform (Scotland) Act 2010, including children's services. All such care services are covered by the duties to ensure appropriate staffing and appropriate training for staff, and must have regard to guidance from the Scottish Ministers, issued following consultation. However, only care home services for adults will be subject to Section 82A of the Bill, which covers the development of staffing methods, unless specified in regulations at a later date.
The Financial Memorandum (FM) to the Bill provides a summary of current staffing in social care. It states that, at the end of 2016, 'the social services workforce is the largest public service workforce in Scotland, with 200,650 people in paid employment....This makes up approximately 7.7% of all Scottish employment.'
The structure of employment is complex, with the workforce employed in 13,481 active services registered by the Care Inspectorateii, 42% of workers are employed in the private sector,31% in the public sector and 28% in the third sector. At the end of 2015:
2,644 employers provided care services in Scotland (excluding child-minders, but including children's care services;
1,536 were independent sector organisations;
1,070 were third sector organisations;
80% of service providers employed fewer than 50 people
The FM 1cites research carried out by Scottish Care (an independent care sector representative body) that 'found that 49% of services reported using agency care staff and 33% use agency nursing staff. Services report that they are increasingly relying on agency staff and 5% reported using agency nursing staff all the time. As a result of using agency staff, 80% of staff reported a negative impact on their finances and 56% reported a negative impact on the quality of care.'
At present, care service providers must comply with Regulation 15 of the Social care and Social Work Improvement Scotland (Requirements for Care Services) Regulations 2011 2 This makes it a requirement to ensure appropriate numbers of suitably qualified and competent staff for the health, welfare and safety of service users. This Bill does not amend this requirement, but moves it from secondary to primary legislation. The Policy Memorandum argues that this will provide parity and coherence across health and care settings. However, a number of stakeholders (eg. COSLA, SSSC and the Care Inspectorate) 3 have said that this legislative change is unnecessary, and further, that statutory requirements are already supplemented by the new health and social care standards.4
Development of National Workforce Planning
The Scottish Government has published a three-part National Health and Social Care Workforce Plan to lay the foundations for improved workforce planning across integrated health and social care services. However, it is important to reiterate that nothing in the Bill relates to national workforce planning, it only relates to duties on Health Boards, and providers of care services and service providers to ensure that appropriate staffing is in place. This should be considered while reading the following section. The Workforce Plan demonstrates the Scottish Government's aspiration for national planning and does not inform the Bill.
Part 1 5of the Workforce Plan covers NHS Scotland. Part 2 6covers social care, and was prepared in collaboration with COSLA . Part 3 7covers primary care.
Part 2 of the National Health and Social Care Workforce Plan makes seven recommendations to begin the process of thinking about workforce issues in a more integrated way. The section below lists and explains the recommendations. Most relate to the work required with the health and care sectors, in the context of integration, to start the process of a national workforce planning process.
The recent publication of the Workforce Plan, and the first four of these recommendations indicate that workforce planning in the sector is not highly developed, and that the process at the national level is in its infancy. Understanding of, and data relating to the sector is far behind the NHS in terms of its workforce, workloads and work patterns. For example, we have no way of knowing whether a person is working for one or more home care agencies, as well as/or working in a care home, and possibly also as a personal assistant, nor how the work, pay and conditions might vary from one situation to another.
Data, analysis, tools and guidance to support workforce planning
Recommendation 1: Integrated workforce data
To enable better collation of health and social care workforce data to support national and local workforce planning. This will draw on the work of the Scottish Social Services Council and the Care Inspectorate and take place in alignment with the work being led by NHS Education for Scotland on the NHS Scotland workforce in response to Part 1 of the Plan. The work will contribute to the wider, whole system approach required for health and social care in the future.
Recommendation 2: National and local labour market and workforce analysis
To develop our understanding and provide evidence of the interactions between the national and local labour market pressures, the interactions between different parts of the sector and the specific challenges presented by the configuration and location of the current social care workforce.
Recommendation 3: Workforce planning guidance for partnership working
To develop guidance for Integration Joint Boards and their commissioning partners in local authorities and NHS boards that supports partnership working for the formulation of workforce plans at regional and local level that include consideration of the third and independent sector workforce. This work will aim to:
engage with third and independent sector employers and/or their representative organisations, and trade unions;
support and facilitate alignment of local workforce plans with associated commissioning and financial plans;
make use of the work delivered under recommendation 2 above, to develop improved understanding and awareness of the impact of market mechanisms in social care; to develop approaches through which workforce planning can take these mechanisms into account in contributing to the delivery of improved outcomes for those who use services.
Recommendation 4: Workforce planning tools
To progress and co-produce social care and multi-disciplinary workforce planning tools that support the delivery of high quality care that reflects the new health and social care standards, and enable service redesign and new models of care. In developing this work, we will take account of progress with planned Scottish Government legislation that includes a focus on tools and methodology to inform and support workforce planning, starting with nursing and midwifery in the NHS.
6 Part 2 of the National Health and Social Care Workforce Plan
In 2016, the Scottish Government commissioned research into recruitment and retention in the social services workforce that showed that the social service sector use a variety of approaches to workforce planning. COSLA and other stakeholders claim that innovation and flexibility will be stifled in the sector in these areas in particular, as well as more generally. Some stakeholders believe that any measures that seek to impose methodologies on such a diverse sector will remove the capacity for flexibility in how staff are deployed and, if more staff are deemed to be necessary without further resource, then some provision could become financially unsustainable, so increasing pressure on services further. These concerns are covered in more detail below and in many of the individual submissions. (eg. Borders IJB and Council, NHS Orkney, SPDS, East Ayrshire IJB, Marie Curie, CCPS,Chief Officers Group)
At a time when commissioners and providers are looking to deliver innovative models of care for the 21st century which are tailored to changing demographic, different client needs, current financial challenges and to emerging technology, our concern is that legislation would be prescriptive and stifle innovation. Conversely, if the legislation has no impact on models of care then, as above, it is not clear what added value this Bill will have.
Innovative approaches are required to ensure we have the appropriate staff to provide high quality care. The Care Inspectorate has been working with care homes that have sought to change their staffing and skill mix, for example by upskilling senior carers in care homes to ensure stable yet flexible staff teams. Legislating for the use of a tool to provide staffing levels that is regulated by the Care Inspectorate could impede the progress completed to date.
COSLA submission 3
Governance and regulation of health and social care services
The Care Inspectoratei (CI) is the regulator for registered care services across Scotland, and the scrutiny and improvement body for social work. The CI inspects care services and social work services. It was created under Part 5 of the Public Services Reform (Scotland) Act 2010 1. It undertakes inspections of care services to ensure that they comply with relevant legislation. Services must register with the Care Inspectorate and this registration can be refused or revoked if standards fall below an acceptable level. However, the Care Inspectorate, where it can, should seek to enable and encourage improvement of a service, before issuing a more formal improvement notice. If registration is refused or revoked a service cannot legally run. The Care Inspectorate can also seek an emergency cancellation of registration through the Sheriff court.2
Inspections of care services (since July 2018) evaluate the quality of the service across key areas like people's wellbeing, staffing, leadership, the setting and care planning. 3
There is no single equivalent independent body that regulates and inspects health services in this way, although Healthcare Improvement Scotland (HIS), a non-territorial health board that was created by the same legislation as the Care Inspectorate 4, does do inspection work in NHS hospitals. Its focus is on safety and cleanliness, and, since 2016, HIS registers independent health settings such as private hospitals and clinics. One of its other key functions is to provide and embed quality assurance, with the aim of supporting Health Boards to improve quality through evidence-based research and practice. For some years, HIS and the CI have carried out joint inspections of integrated health and social care services.
Both bodies use the new Health and Social Care Standards 5in their scrutiny and improvement work. These have been in place since April 2018. The headline outcomes for the standards are that individuals:
experience high quality care and support that is right for them
am fully involved in all decisions about their care and support
have confidence in the people who support and care for them
have confidence in the organisation providing their care and support
experience a high quality environment if the organisation provides the premises
Under these headings are more detailed outcomes and expectations that everyone should have or expect from a health or care service. The Standards are intended to be wide reaching and flexible. They are focused on the individual experiences of people using services, and are underpinned by the principles of: dignity and respect; compassion; being included; responsive care and support; wellbeing.ii
A significant number of submissions to the Committee's Call for Views were received from third sector organisations (eg MS Society, Marie Curie, Chest Heart Stroke, Inclusion Scotland). Their concerns centred on the impact of the Bill on people who use services, although not exclusively so. Inclusion Scotland state that reference to co-production is missing in the Bill, and that this approach to all health and social care legislation is underpinned by the Community Empowerment (Scotland) Act 20157 and The Public Bodies (Joint Working) (Scotland) Act 2014 8. Inclusion Scotland's submission9 make reference to Audit Scotland's NHS in Scotland 2017 report which states that: 10
NHS boards have had legal duties to involve the public in designing services for a number of decades. More recently, the Public Bodies (Joint Working) (Scotland) Act 2014 also placed duties on Integration Authorities. The Community Empowerment (Scotland) Act 2015 (the Act) marked a significant shift in the Scottish Government’s expectations of how the Scottish public should be involved in decisions that affect them. NHS boards, integration authorities, and local authorities all have legal duties placed on them by the Act.
What does the Bill aim to do?
The legislative context
The primary legislative context for the Bill are sections 12H and 12I of the National Health Service (Scotland) Act 1978 1 which place a duty on NHS Boards to put and keep in place arrangements to monitor and improve the quality of health care they provide and to improve the management of the workforce and workforce planning. The National Workforce Planning Framework and the 2005 Guidance that accompanied it established how the requirement to workforce plan would be met. Revised guidance was issued in 2011, setting out high level steps for health boards to consider and follow.
As described in earlier sections, a less direct legislative context is provided by the Public Services Reform (Scotland) Act 20102 and the Social Care and Social Work Improvement Scotland (Requirements for Care Services) Regulations 2011 3
However, the Policy Memorandum 4asserts that:
the general appropriate staffing duty in the Bill sets out more specific requirements – effectively 'levelling up' requirements on Health Boards to broadly mirror existing requirements on care service providers, making more explicit the requirements around the staffing element of workforce planning.
PM4
It is not clear how or if this will happen in practice, or what it will actually mean, given the very specific duties regarding registration and regulation that the Care Inspectorate have under the Public Services Reform (Scotland) Act 2 . These duties, which state which actions and sanctions are available to the Care Inspectorate, are not reflected in the duties and role of Healthcare Improvement Scotland or any other body in relation to health boards.
Despite the formation of integration authorities to direct resources and plan health and care services for their populations, they are not employers, so workforce planning effectively remains the responsibility of health boards and local authorities, which have to ensure that appropriate staffing is in place to provide those delegated services.
The driving policy direction for the Bill is to ensure 'the right people in the right place at the right time to deliver sustainable, high quality services with improved outcomes for the people who use services, irrespective of health or care setting'4. It is the intention that the requirements on Health Boards related to workforce planning will flow through to Integration Authorities in respect of delegated functions and services. However, as the Royal College of Anaesthetists highlights, 'By not being designated as the employer, the Integration Authority may be limited in its control over staffing decisions'.iUnison also raises questions about accountability and oversight when it might not be wholly clear which party - the commissioner of services (IJB), the Care Inspectorate or the provider of services - has the responsibility for compliance8
Given the fragmentation of delivery of care services the question of who the designated person with responsibility for ensuring safe staffing levels – and how they are reported is a serious one. This is particularly the case when rather than being provided directly care provision is commissioned from a third party. Who would be responsible for measurement (of staffing levels) – the private care provider or the IJB/ Council commissioning the care? This relates to the issues outlined earlier about the possibility of the legislation being ignored. Whilst there is obviously a wide variety of standards - it has not been our experience that detailed measures enforcing contract compliance has been a great speciality of commissioning bodies in Scotland. If this Bill is to be considered under that rubric it is more than possible that its intentions will not be realised.
UNISON 9
Legal sanctions/negligence
There are no legal sanctions mentioned in the Bill, nor does it cover what happens if the statutory duties are not met. However, the PM (S.89) states that compliance will sit with organisations not individuals, and that monitoring will occur through existing local and national reporting and regulatory mechanisms.4
This means that an individual could not easily use the legislation to seek legal redress/ compensation in an instance where they felt that unsafe staffing had led to a bad outcome for them.
The law of negligence requires that, where a person or body behaves negligently, they have an obligation to pay compensation to anyone who suffers harm as a direct result. Breach of a statutory duty can form the basis of a claim for negligence, but the law in this area is not clear.
Legislation may specifically include or exclude the possibility of raising court action for negligence as a result of breach of a statutory duty. However, the Bill is silent on this matter. In this case, it is up to the courts to decide whether it was the intention of the legislature to allow individuals to take court action on the basis of the duty. This is less likely – but by no means impossible – if the duty is placed on a public body.
Committee Call for views on the Bill
Many of the concerns raised when the Scottish Government first consulted in 2017 remain. 1 However, the Committee's Call for Views provides a comprehensive range of observations, questions and concerns about the Bill. Some of the key, general issues are raised here. These and others will emerge through the Committee's scrutiny work over the coming weeks.
General Principles
Most submissions to the Committee's Call for Views were supportive of the guiding principles of the Bill. Scottish Borders Council/Integrated Joint Board stated that 'The guiding principles for staffing are laudable. No-one is likely to take issue with a main purpose aimed at providing 'safe and high quality services'1
Many submissions endorsed the intentions of the Bill to introduce a consistent approach to safety and quality across Scotland, and across health and social care. Most also expressed the view that to make staff involvement and engagement in the process a requirement was a very positive aspect of the Bill.
The intentions of the Bill are admirable and use of a standardised and robust approach across Scotland should support decision making to be more transparent and to allow comparison...there is an opportunity for staff to be more widely engaged in reviewing safe staffing levels.
NHS Ayrshire and Arran 1
This was supplemented by third sector submissions that called for a greater degree of involvement from those who used services and from their representatives. This was, as discussed above, considered to be more in the spirit of the co-production agenda (eg Inclusion Scotland, The Alliance). However, this is not a Bill about patient or service user rights.
With reference to the guiding principles (Part 1), The Law Society said:
The guiding principles are unobjectionable, but so general and multi-factorial as to leave plenty of scope for subjective judgement and the inevitable juggling of competing priorities....and it would be difficult to challenge a decision of a health or care service provider on the basis of these.
1
Some (RCN, NHS Orkney)1 believe that this section is weakened by a lack of definition in relation to terms such as 'appropriate' and 'safe':
The perception of what is safe and what has been agreed may differ and we need to ensure that this doesn't in turn become an area of tension between staff and managers'(NHS Orkney). 1
Most submissions said little about Part 1 of the Bill and instead focused on Parts 2 and 3. As the Law Society goes on to state:
The principles and duties are used to set the scene for the real point of the Bill which is the requirement that the Bill imposes on Health Boards and care service providers to follow particular staffing methods that are to be prescribed in regulations by the Scottish Ministers
Is the Bill limited in its scope?
In terms of legislative scope, it is important to note that this Bill is about staffing and workload planning, not wider workforce planning to ensure adequate supply of staff to meet the future requirements for staff in health and social care as dictated by the broader policy agenda. The Bill is chiefly concerned, the guiding principles notwithstanding, with workforce and workload planning in limited circumstances.
The majority of submissions were concerned that the Bill, while laudable in its principles, was being introduced into a workforce context that is under pressure from general recruitment and retention problems nationally. Lack of availability of staff, and short supply in many health professions, as well as in the social care sector, means that it is challenging to meet the requirements and staffing establishments currently set by Health Boards and social care providers. Health Boards and providers are concerned about what support will be available to them when factors affecting the staff available may be outside their control. (eg.Scotland Excel, Scottish Executive Nurse Directors' Group, Cancer Research UK, NHS Tayside, Royal College of Physicians of Edinburgh, Scottish Borders Council, NHS Ayrshire and Arran). The impact of Brexit in creating more pressures on recruitment and retention was also raised (eg. The Brain Tumour Charity).
Placing workforce planning tools on a statutory footing does nothing to address recruitment and resourcing issues in the health and social care service and among providers.
Scottish Borders Council and IJB 1
Another significant criticism on the scope of the Bill was that it was seeking to address two things with one approach and one set of tools: ensuring that the retrospective results delivered by current tools delivered an appropriate staffing establishment but also to ensure that staffing was safe on a day to day basis. The current tools are not designed to provide information for day to day adjustments. The SPICe staff survey highlighted a range of methods (or none) that were used on a daily basis that were sensitive to actual risk and immediate patient acuity. The Bill appears to conflate the two very different exercises that Health Boards undertake to make health settings safe in staffing terms.
The Bill is trying to do two different things using one set of tools. The common method describes a distinct process which uses the extant tools to do the finance / workforce planning for the establishment setting on an annual basis.
The day to day review of staffing requires a different approach to provide an assessment of the right number of nursing staff with the right knowledge, skills and experience, in the right place at the right time in real time and appropriate tools such as the SafeCare Tool, used by NHS Lothian, which applies a twice (or three times) daily census of patient acuity to the available staffing determine the extent to which patient needs can be met and allows senior decision makers to deploy the resources to the optimum.
Other factors to bear in mind:
Those tools used only annually are not familiar to staff
Those tools used annually do not consistently deliver outputs useful to the planning cycle (as may not be used / reported on at a time that feeds the planning or financial cycles)
Some tools (Community , Perioperative, Emergency Department) are extremely time consuming and staff are unwilling to participate
The perception of what is safe and what has been agreed may differ and we need to ensure that this doesn’t in turn become an area of tension between staff and managers.
NHS Lothian 1
Audit Scotland raised the matter of supplementary staffing; the use of agency, bank and locum staff to manage day to day staffing shortages. The PM asserts that if the tools were used consistently and properly, the need for supplementary staff would decrease. There is no funding associated with the Bill to address any rise in staffing costs that result from the Bill's requirements.
it is anticipated that as a result of application of the robust approach to planning staff resource requirements described in the Bill the need for supplementary staffing will reduce significantly
3
Audit Scotland says that there are risks associated with additional staffing costs:
The Scottish Government and NHS Boards have already been looking to reduce supplementary staffing costs, but these costs continue to rise. As we reported, in December 2015, the Scottish Government launched the Managed Agency Staff Network (MASNet). It aimed to reduce agency spending and improve the arrangements NHS boards have for managing, monitoring and reviewing agency staff needs. Nursing agency costs have risen from £4.2 million in 2011/12 to £24.5 million in 2016/17, in real terms. Since our audit, the 2017/18 figures have been published showing nursing agency costs have fallen slightly to £23.6 million. Given there is a current requirement to apply staffing tools to determine numbers, it is unclear to what extent better use of existing staff resources will reduce these agency costs, or how this will be achieved.
We highlight in our report that agency costs are putting pressure on NHS Boards' pay budgets and that workforce projections are not reflecting demand pressures. We also report NHS staff survey information which shows that around a third of staff surveyed felt there were not enough staff to do their job properly.
4
Audit Scotland goes on to raise concerns associated with the risk of increasing vacancies, and what measures Health Boards and social care providers, who also require nursing staff, should take if the rise continues. The National Health Workforce Plan acknowledges that for the next few years the numbers of student nurses and midwives entering the workforce will not be enough to meet demand. Further, Audit Scotland says that 'the Scottish Government has not fully incorporated future demand for healthcare and the impact of retirements from and ageing workforce' 5
Is the Bill necessary?
A number of submissions pointed out that the Bill will duplicate statutory requirements that already pertain across health and social care.
The proposals risk duplicating existing statutory requirements to ensure appropriate workload and workforce planning for health and social care and social work. Existing requirements (that) are enhanced by the National Health and Social Care Standards1
Scottish Borders Council and IJB 2
With a focus on process, mainly acute settings and 'mechanistic' tools, there is a fear that the outcomes based service planning that has underpinned the integration of health and social care so far, will be undermined by the Bill, not least by how it is structured.
The Bill is split between Part 2 referring to health care settings and Part 3 referring to social care settings. This separation appears to be at odds with the integrated landscapes in which the services delivered by IJBs operate within.
Aberdeenshire IJB 2
Many submissions pointed out that, while the Bill is seeking to introduce conformity and consistency across the health and social care fields, and that it is bringing inspection and support functions together by the joint working of HIS and the CI, it does not recognise the very different landscapes of health settings and social care provision. The latter is delivered by a broad range of providers (private, voluntary and local authority) in very variable settings ranging from a large care home to someone's flat.
Multi-disciplinary teams, integration of health and social care and skewing of resource
Related to the preceding concern that the Bill does not recognise how differently the health and social care sectors operate, and how differently they are governed and regulated: most submissions said that the focus in Part 2 on existing tools for nursing and midwifery would lead to a focus by Health Boards, in terms of resource and wider planning, on these professions at the expense of other health professionals, and particularly other settings and contexts.
Since the tools were developed, integration of health and social care, as well as policies and resourcing pressures requiring the redesign of many services, now means that the tools are less applicable.i Further, because for many other health professions, such as Physiotherapists, Anaesthetists and Clinical Nurse Specialists for example, the tasks they undertake are increasingly about individualised patient outcomes, it would be very challenging to develop tools based upon observational studies of workload/tasks (personal communication with Health Board staff member).
Other settings, where the tools are not used, might also be at risk of being overlooked. For example, workforce planning tools are not used in all settings even where nurses work' or might work, such as in prison healthcare, sexual health, addiction services, hospital to/at home services and hospices for example
The use of staffing tools is currently limited to those already developed, mainly within nursing models. (T)his is unrepresentative of many integrated services which utilise skills across a multi-disciplinary team. It is unclear how such an integrated environment can be viewed as safely staffed if only one part of this team is represented in that assessment
Aberdeenshire IJB 1
Workforce planning methods (staffing methods) hav(e) only a partial, or distorting impact in multi-disciplinary teams within integration authorities. This will have the paradoxical effect of undermining integration.
NHS Ayrshire and Arran1
The Bill itself - Part 1 - Guiding Principles for Staffing
The Bill is in four parts. Part 1 sets out the guiding principles for health and care staffing. The first principle is that staffing is in place to provide 'safe and high quality services'. It is important to note that this part spans the health and care services landscape, and all the staff within it, and refers to all health settings and all care settings registered by the Care Inspectorate. The intention is to create a coherent legislative framework across sectors through these guiding principles. There are then a set of six principles that health boards and care providers must have regard to when planning staffing:
(i) taking account of the particular needs, abilities, characteristics and circumstances of different service users,
(ii) respecting the dignity and rights of service users,
(iii) taking account of the views of staff and service users,
(iv) ensuring the well being of staff,
(v) being open with staff and service users about decisions on staffing, and
(vi) allocating staff efficiently and effectively.
The Scottish Government hopes that the inclusion of these principles will 'mitigate the risk highlighted by the initial consultation that resources may be diverted away from staff groups and settings not covered by existing workload and staffing tools.' p21, Policy Memorandum 1.
Sections 2 and 3 set out the duties on Health Boards, local authorities and integration authorities when they are commissioning services. Health Board commissioners must have regard to the guiding principles in ensuring that appropriate staffing is in place. Local authorities and integration authorities must have regard to the guiding principles and the duties relating to staffing imposed on those providing care services.
What about integration of health and social care?
There is a clear distinction between health and social care sectors in the Bill, the former driven by the 1978 Act and the latter by Regulation 15 of the Social Care and Social Work Improvement Scotland (Requirements for Care Services) Regulations 2011 2 and, in reality the structures of the sectors bear little comparison. However, there is an attempt in the Bill to take account of the integration of health and social care through the 'guiding principles outlined in Part 1, section 1, as listed above (as well as seeking to bring the roles of the CI and HIS closer together, and by introducing the potential for staff planning tools in the social care sector).
The guiding principles are, according to the PM, aligned with the existing 3planning principles for health and social care integration as set out in the Public Bodies (Joint Working) (Scotland) Act 2014 4. Statutory Guidance 5 has also been issued on how these principles should be applied. These guiding principles are also aligned with those underpinning the new health and social care standards 6
The new health and social care standards principles are:
Dignity and respect
Compassion
Be included
Responsive care and support
Wellbeing
Part 2 - Staffing in the NHS
Part 2 of the Bill seeks to amend Section 12I of the National Health Service (Scotland) Act 1978 1These provisions extend and provide more detail to the duties on health boards concerning staff governance and workforce planning. Under the 1978 Act, 1 it is the duty of health boards to 'put and keep in place arrangements for the purposes of—
(a) improving the management of the officers employed by it;
(b) monitoring such management; and
(c) workforce planning.'
The amendments to the 1978 Act contained in Part 2 of the Bill provide detail on the 'common staffing method'.
As explained in the 'Workforce Planning in Health Settings' section, Part 2 of the Bill has most detail on the proposed common staffing method which is based upon the existing nursing and midwifery tools. The modified staff planning method now includes additional requirements that:
staff are engaged in the process and informed of outcomes
transparent risk-based prioritisation and decision making is carried out
there is the provision of senior clinical professional advice (in addition to use of the Professional Judgement tool)
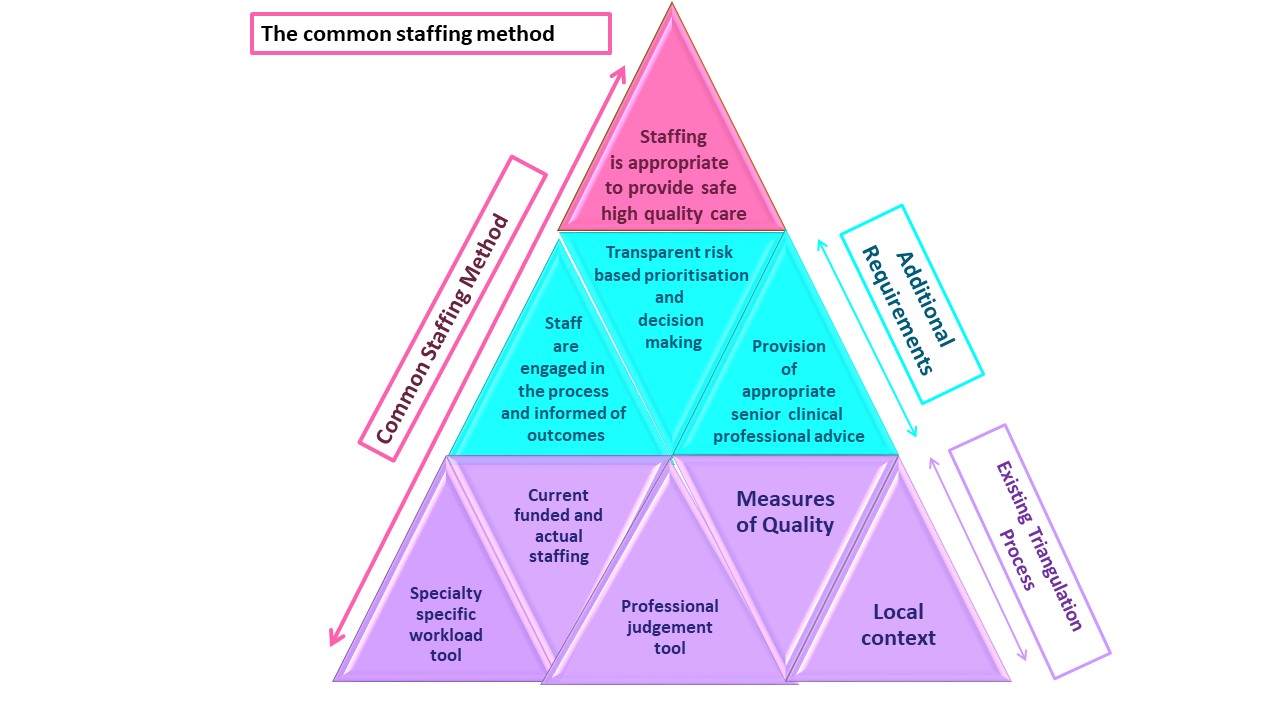
The method used, and tabulated in the Bill (see Table on page 4 of the Bill) 4, currently refers to the types of health care and employees that are already covered by existing workforce planning tools, and which are part of the existing 'triangulated approach' to workforce planning . However, the legislation will not only cover employees currently listed - registered nurses and midwives and doctors in emergency departments, but those staff members who are carrying out duties delegated by registered nurses and midwives and, in the case of Emergency Care, medical practitioners.
The Bill, if enacted, could be amended by regulations to further extend provision/s to cover other staff and other health care settings or services.
The Policy Memorandum (p19)3 states that the intention is for the general 'appropriate staffing' duty to 'level up' requirements such that there is equivalence in requirements not only across the health and care sectors but also with regard to all staff providing care, such as allied health professionals and medical practitioners. As has already been stated, it is not clear how this intention will be achieved by the Bill.
As noted earlier, concerns have been raised that the Policy Memorandum 3 appears to conflate the two aspects of workforce planning and deployment, namely how many staff should be included in the permanent establishment, as identified by following the triangulated approach, and the more reactive rostering and risk assessment that occurs daily or several times a day on most wards. These real-time assessments are essential to take account of exceptional sickness absence, higher than planned-for acuity of patients, redeployment of staff to other areas, or other immediate contingencies that arise on a daily basis. The 'common staffing method', and therefore the Bill, does not explicitly address the issue of immediate staffing pressures. These pressures and gaps in staffing can occur despite the tools having been applied rigorously.
Part 3 - Staffing in Care Services
Part 3 of the Bill aims to enable the social care sector to build on the existing mechanisms contained in Regulation 15 of the Social Care and Social Work Improvement Scotland (Requirements for Care Services) Regulations 2011 1 . It provides a function for the Care Inspectorate to lead the development and validation of methodologies and workload and workforce planning tools, in collaboration with the sector, to be used in care home for adult settings where necessary (PM para. 86 )2. It also places the general 'appropriate staffing' duty on care service providers (Section 6), giving them an equivalent responsibility to Health Boards. The PM states that:
The purpose of including care services in the legislation is to enable the sector to build on and strengthen existing mechanisms by placing Regulation 15 into primary legislation and creating a cohesive legislative framework across health and care settings.
p.262
However, the move from secondary to primary legislation of this requirement makes no difference in legal terms. The Bill places no (additional) sanctions on either sector, and it does not deal with the regulatory background. What the Bill does demonstrate however, by seeking to introduce some equivalence between the health and care sectors, is how different they are in legal and regulatory terms, in addition to their profound differences in structure, governance and organisation. Aspects of these differences were raised in most submissions that commented on Part 3.
Part 3 of The Bill seeks to provide:
A power for the Care Inspectorate to work in consultation with the care sector to develop staffing methods. Initially this will only be for care homes for adults;
A regulation-making power for the Scottish Ministers to enable the Care Inspectorate‘s power to be extended to other care settings in the future, if the need arises;
A regulation-making power for the Scottish Ministers to require the use of any staffing methods developed by the Care Inspectorate;
The ability for Scottish Ministers to issue guidance to care service providers setting out further detail around the duties contained within the Bill.
para.130 PM 2
Part 3 of the Bill does not provide any detail on how the methodologies and workforce planning practices should be developed. The Care Inspectorate will lead the work to develop the methodologies in collaboration with the sector. At this stage, the Bill only covers the development of workforce planning methods for care homes.
Part 4 - General Provisions
Part 4 of the Bill contains the General Provisions relating to modification of the Act, if passed, by regulations, which would be subject to affirmative procedures (if the text of the legislation is amended) or negative procedures otherwise.
It also covers Commencement details. Part 4, Sections 12 (ancillary provision) and 14 (Short title) commence on the day after Royal Assent is granted. The remainder of the Bill would come into force on days named by the Scottish Ministers in regulations. A number of submissions, including the Law Society, highlight that the Bill lacks clarity in a number of areas, which would need to be prescribed through regulations or clarified in guidance.
the real point of the Bill (which) is the requirement that the Bill imposes on Health Boards and care service providers to follow particular staffing methods that are to be prescribed in regulations by the Scottish Ministers. All detail on how to achieve 'appropriate staffing' will be in these regulations.
The Law Society 1
Monitoring and Enforcement
It is not clear what will happen if a health board or social care provider does not meet the duties set out in the Bill. Health Boards and social care providers might not be able, because of vacancies or local or national unavailability of staff, to fulfil the establishment that the board or organisation has deemed to be appropriate and necessary to provide high quality, safe care. Health Boards would either have to redesign the particular service or reduce the number of beds available to that service; which could mean the same thing. Almost all submissions raised the issue of scope: if the Bill does nothing to address supply and availability of trained staff, then Boards and social care providers alike would find it extremely difficult to meet the duties which would be placed upon them by the Bill. (For specific examples of effects on patients of a shortage of radiologists, see Cancer Research UK submission. 1)
Social Care providers are regulated in a different way.They already have a duty to ensure that there are enough appropriately trained staff within a service registered with the Care Inspectorate, and appropriate staffing of services is assessed by the Care Inspectorate .
It is also not clear what would happen if a health board does not adhere to the results from applying the common staffing method. In reality it appears that the requirement to provide appropriate staffing at all times and in all instances must be balanced by the Board against all other clinical, statutory or financial priorities. The lack of clarity around compliance is highlighted above and in a number of the written submissions (eg Royal College of Psychiatrists, NHS Orkney, Royal Blind, RCPE)
Healthcare Improvement Scotland
NHS Healthcare Improvement Scotland (HIS), which provides public assurance of quality and safety of healthcare through advice, guidance, support and standards has been commissioned by the Scottish Government to develop specific quality measures for nursing and midwifery as part of the Excellence in Care Programme. It is likely that HIS will develop the future staff planning tools for health care settings. Most Independent Health Clinics are required to register with Healthcare Improvement Scotland.
As has been explained under the social care staffing section, care services are rigorously and explicitly monitored by the Care Inspectorate. Certain requirements, including appropriate staffing, are already a condition of registration of a care service. The Care Inspectorate also has an improvement and support function and, in practice, will work constructively with providers to achieve the required standards of registration.
Both the Care Inspectorate and Healthcare Improvement Scotland take the new Health and Social Care Standards 2 (from April 1 2018) into account in relation to their inspections, scrutiny and registration processes.
There is a short sub-section (12IE) in Part 2 of the Bill on 'Reporting on Staffing'. This states that after the end of each financial year, boards must report on how they have carried out their duties under three preceding subsections: (12IA)'Duty to ensure appropriate staffing'; (12IB) 'Duty to follow common staffing method' and (12ID) 'Training and consultation of staff'. The PM says that in practice reporting will be done through existing annual reporting mechanisms. (para 124) and through existing local and national reporting and regulatory mechanisms and HIS and the Care Inspectorate scrutiny processes. (para 89) 3
Resources and Finance
The Financial Memorandum(FM) sets out the costs associated with the Bill. Scrutiny will be undertaken across the Health and Sport Committee's upcoming evidence sessions. This section briefly summarises what additional funding will support the implementation of the Bill.
The FM acknowledges that health boards face difficulties in filling vacancies because of the shortage of available staff, and that the Bill does not directly address those shortages. However, it is hoped that the legislative requirement to apply the existing tools will improve board projections on future staffing requirements. In both the FM and the PM, there is reference to the high costs of supplementary staffing required to meet short-term needs by health boards. It is not clear how the provisions of the Bill will address the use of supplementary staff ( or the shortage of available staff and vacancies), assuming that the tools have been used by health boards since 2013.
The resourcing associated with the Bill only covers the direct costs - the development and implementation of tools and methodologies and the training of staff in their use. It acknowledges that there might be a consequential impact on the demand for staff, but that this will be the responsibility of health boards to manage, and the Scottish Government do not see that there will be an overall increase in costs incurred by health boards. There is an assumption that health boards will have to consider the of redesign services in order to reconcile staffing, high quality care and finance issues.
The Summary of Costs (Table 1 in the FM) covers the direct costs associated with the Bill, some of which are already incurred by health boards (staff training) or the Scottish administration (Nursing and Midwifery workforce planning tools infrastructure and maintenance, IT updates etc). For up to three years there will be additional funding for boards to support staff training (£664,430 assuming that 50% of Band 7 nurses will be trained) and to fund 16 new nurse managers to apply, collate, analyse and report information from the nursing and midwifery tools (£931,469 in 2019-20, with half that amount being provided in the immediately preceding and proceeding years) However, there appears to be no new funding to review and improve the existing tools.
As for developing new workforce planning tools, the Nursing and Midwifery Workforce Planning Project estimates that to develop and implement a new tool costs £538,185. The FM allows for the development of one new tool per year for the next six years, with additional funding to cover the Planning Project's infrastructure and expansion within NHS Healthcare Improvement Scotland (11 new posts). How a new tool is developed is covered in Table 2 of the FM. The costs covered above are only to develop new tools in the health care sector.
There are no national workforce planning tools within the care sector currently. The Care Inspectorate will be given the function to lead work with stakeholders to develop a tool or methodology for care homes for adults initially, if one is deemed necessary. In order to assess the evidence of need for a tool, £50,000 has been allocated in 2019-20 for commissioned research and analysis. Funding for six staff within the Care Inspectorate is outlined in Table 7 of the FM, who will support tool and methodology development, with costs given from 2020 to 2024. Further support is outlined for provider training as well as additional inspector support for engagement and inspection training.
It is also anticipated that providers will incur costs through their involvement in tool and methodology development (£200,000 per year for three years across the care sector), as well as for staff training (£150,000 per year for two years across the care sector). These estimates have been included in the cost summary (Table 1 in FM).
The Financial Memorandum acknowledges that there is much more uncertainty in the financial implications of developing tools and methodologies in the care sector because there is no precedent, and because there are currently few, if any, parallels between the structures of the health and care sectors.