Health and Sport Committee
What should primary care look like for the next generation?
Introduction
We decided that given multiple developments in Primary Care services it was appropriate to take a broader look at services and how they will look in the future. This report covers the initial phase of our inquiry when we asked the public how much they understood about how primary care worked in Scotland. We provided them with some background information on recent policy and legislation and worked with them to plan how they wished to see primary care organised in the future, within the current policy framework and beyond.
Background
Primary care is the first point of contact with the NHS. This includes contact with community based services such as General Practitioners (GPs) or Community Nurses. It can also be with Allied Health Professionals (AHPs) such as Physiotherapists and Occupational Therapists, Midwives and Pharmacists.
The Scottish Government’s National Clinical Strategy for Scotland signals the transformation required in Primary Care. “The strategy describes the rationale for an increased diversion of resources to primary and community care. Stronger primary care across Scotland should and will be delivered by increasingly multidisciplinary teams, with stronger integration (and where possible, co-location) with local authority (social) services, as well as independent and third sector providers”.
The Scottish Government’s vision for the future of primary care services is for multi-disciplinary teams, made up of a variety of health professionals, to work together to support people in the community and free up GPs to spend more time with patients in specific need of their expertise. It seeks to reduce pressures on services and ensure improved outcomes for patients with access to the right professional, at the right time, as near to home as possible.
A new Scottish General Medical Services Contract Offer was agreed in 2018.
The contract sees GPs fulfilling roles to support a wide range of clinical professionals, working as an expert medical generalist and senior clinical decision maker within multi-disciplinary community teams.
The GP contract also sets out the role of the multidisciplinary team and the practice team, including general practice nurses, practice managers and practice receptionists.
The 2018 GP contract also notes that the "non-expert medical generalist workload needs to be redistributed to the wider primary care multi-disciplinary team". As part of the service redesign a number of services will be reconfigured by 2021.
The Scottish Government is working to transform primary care in order to develop new ways of working that will help to put in place long-term, sustainable change within primary care services that can better meet changing needs and demands:
Putting general practice and primary care at the heart of the healthcare system.
Ensuring people who need care are more informed and empowered than ever, with access to the right person at the right time, and remaining at or near home wherever possible.
Developing multi-disciplinary teams in every locality, both in and out of hours, involved in the strategic planning and delivery of services.
Views of service users
In 2015 the Scottish Government undertook an initiative to seek views from the public on what a healthier Scotland would look like. The findings from that are at annexe D of our report.
In July 2018 the King’s Fund as part of a wider piece of work provided a review of “What do patients want from general practice?”. It reported that:
“A systematic review of 19 international research studies looked at which characteristics were ranked most commonly by patients as priorities for general practice care (Wensing et al 1998). The five most important were:
humaneness
competence/accuracy
patients’ involvement in decisions
time for care
accessibility.”
We obtained views from service users through three approaches:
An on-line survey
A survey of younger people aged between 12 and 25; and
The creation of three randomly selected public panels meeting in the East, West and North of Scotland.
The On-Line Survey
Our aim for the first phase of our inquiry was to hear directly from service users about their future priorities for primary care involving them in the discussion about the need for change in the way primary care is configured. We were aiming to:
To explore what primary care GP/family health services should look like for the next generation; and
To identify the big questions about the future of primary care so that these can be put to the right people as a challenge in phase 2 of our inquiry.
Our on-line survey was designed primarily to promote and highlight the Inquiry itself, as well as to provide a base-line as explained above. There has been a wide range of work already done to capture public views on primary care in Scotland, so this survey would complement and supplement that extant research.
The survey questions comprised a range of mainly ‘closed’ questions on a range of topics relating to primary care. These topics included:
A set of general demographic questions – age, gender, education etc
A general view of the government vision for primary care
Understanding of the range of professionals included in the primary care team, and whether people would want to access them without going through their GP
Priorities for people in their experience of primary care – access to appointments and services, length of appointment etc
The role of digital technology • Data sharing among health professionals
The relationship of GPs to the NHS – the business model
Satisfaction with services
Use of out of hours (NHS 24) services
Primary care funding within the context of the new GP contract • Willingness to pay for any services
Public involvement in how primary care services are run or changed • What should primary care look like in the future
A question relating to further involvement in the inquiry
The survey was launched at the beginning of March and remained open until the end of April. In total we received 2,549 responses, mainly completed on-line although hard copy responses were received and are included in the above total. The survey was promoted through web and social media channels, with targeted work undertaken to try and ensure a wide demographic spread.
SPICe have analysed responses and produced a summary report which is attached at Annexe A of this report. A copy of the survey is, for information, at annexe E.
Scottish Youth Parliament Survey
The Scottish Youth Parliament (SYP) worked with us to ensure we were able to access the views of younger people between 12 and 25. They distributed two of the questions from the survey (views on technology and which health professionals would they like to see), as part of a more comprehensive piece of work they were undertaking.
Their survey received 1,136 responses and a summary report prepared by the SYP containing a series of recommendations is attached at Annexe B. Recommendations mainly cover the use of technology with one urging easier access to specialist support in particular for mental health through their GP.
The Public Panels
We established three public panels of 10-14 people, sampled from a randomly recruited pool to meet to certain criteria (eg age, gender, socio-economic background). The panels were invited to discuss issues similar to those included in the survey in a more in-depth and informed way and to share their views with us. Panels were located broadly in the East (Dunfermline), West (Cambuslang) and North (Inverurie) (to mirror the NHS regions), one in each of the three health regions, with one a more rural location.
The panels, representing only themselves and not any particular interest group, were supported by Parliament staff including researchers from SPICe and facilitation from the Committee Engagement Unit to deliver both education on the issues and opportunities for the panels to deliberate on what they heard. Additional input was provided by a health economist who provided details about other models of delivering care available across the world. Each panel met on two Saturdays.
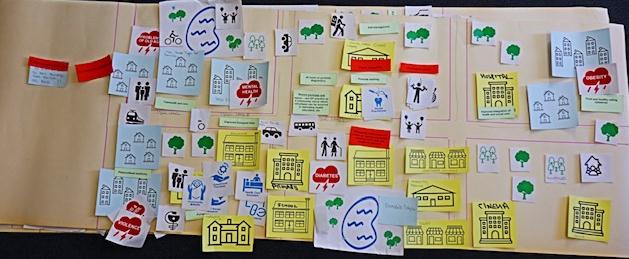
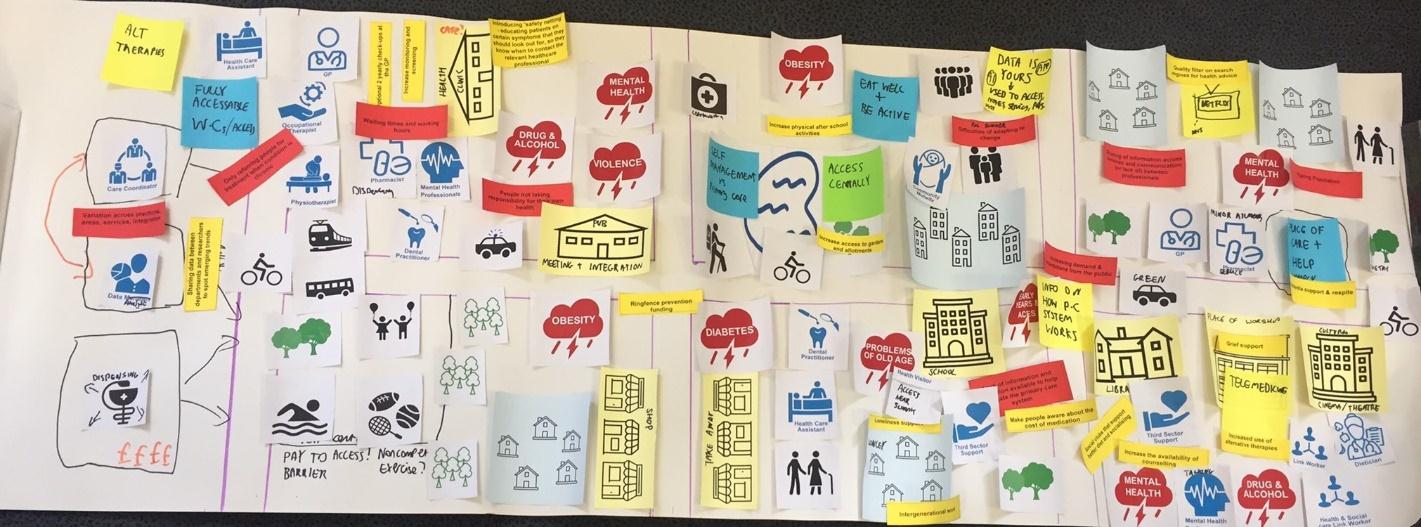
We joined the second meetings to observe and hear the views of the panels directly. Each panel completed a creative mapping exercise to think about how they would like future services to be designed to address the health and social needs in their communities.
We were impressed by the quality and depth of material debated by the panels and we intend to invite representative members to give oral feedback and evidence as the conclusion to our second phase of the inquiry.
A full report from each of the panels detailing in detail the processes they followed and including copies of the output from each panel has been prepared for us and is contained at Annexe C of this report.
Thank you
Our thanks and gratitude are due to the thousands of people who took the time to provide us with their views and tell us their wishes for the future of primary care. We are particularly grateful to the SYP for their assistance and support which is reflected in the large number of young people they consulted, and the detail contained in their report to us.
We are indebted to the public panel participants who gave up two Saturdays to deliberate, debate and conclude on our behalf. It is testament to their commitment that every person who attended week 1 of the discussions returned for week 2, all were keen to be involved and to ensure that the public voice is heard.
What the public has told us
In total we have survey responses from 3685 individuals and reports from three public panels. We use the broad themes coming from the public panels to summarise their main priorities and have included in this detail from the survey and the recommendations of the SYP as appropriate to the questions asked of them.
Use of technology
The priorities from the panels are:
Electronic patient record, shared with all relevant professionals – a single set of records integrated across all care services – consistent platform, used for electronic test results, correspondence, etc.
Ability to contact health professionals by email and schedule appointments online, hold consultations via video.
Using technology/wearables to monitor health e.g. blood pressure, diabetes and sharing information with relevant professionals.
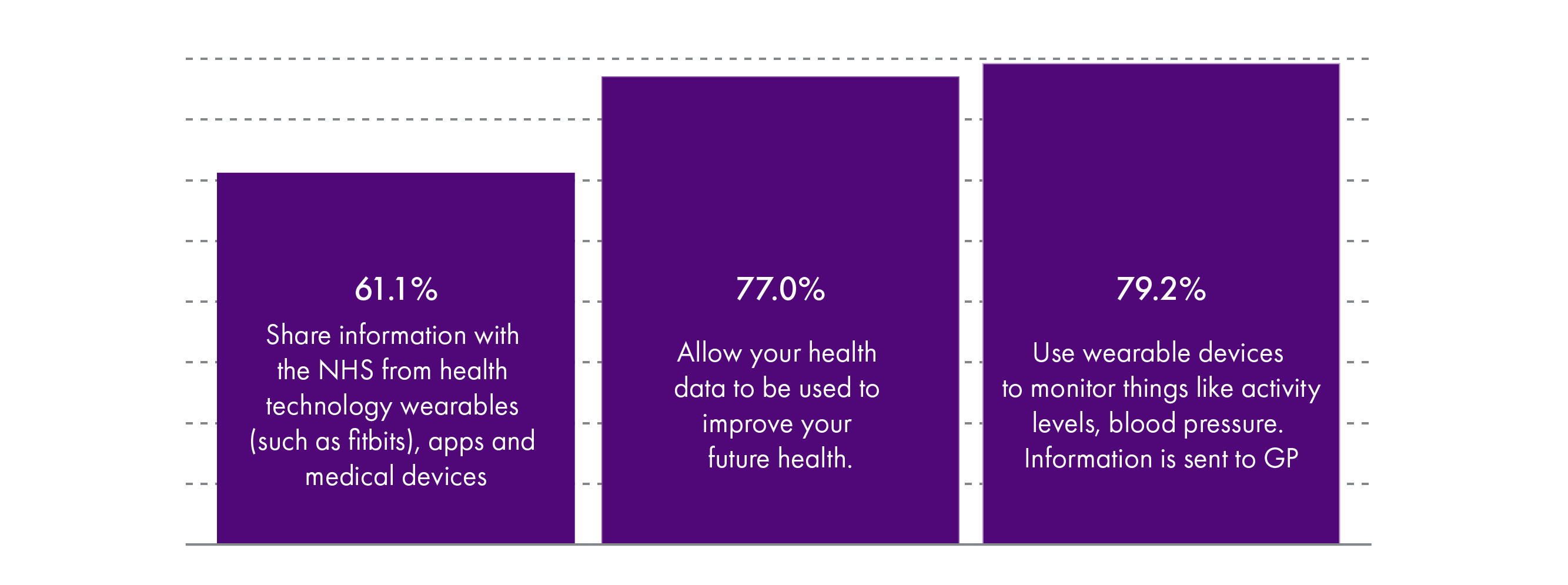
77% of survey responses were happy to allow their data to be shared, slightly more (79.2%) would use wearable devices to monitor activity levels and blood pressures and allow information to be transmitted direct to GPs with 86.2% were happy for their notes to be shared across the primary care team. Although the number willing to share such information with the NHS as an organisation was less at 61% .
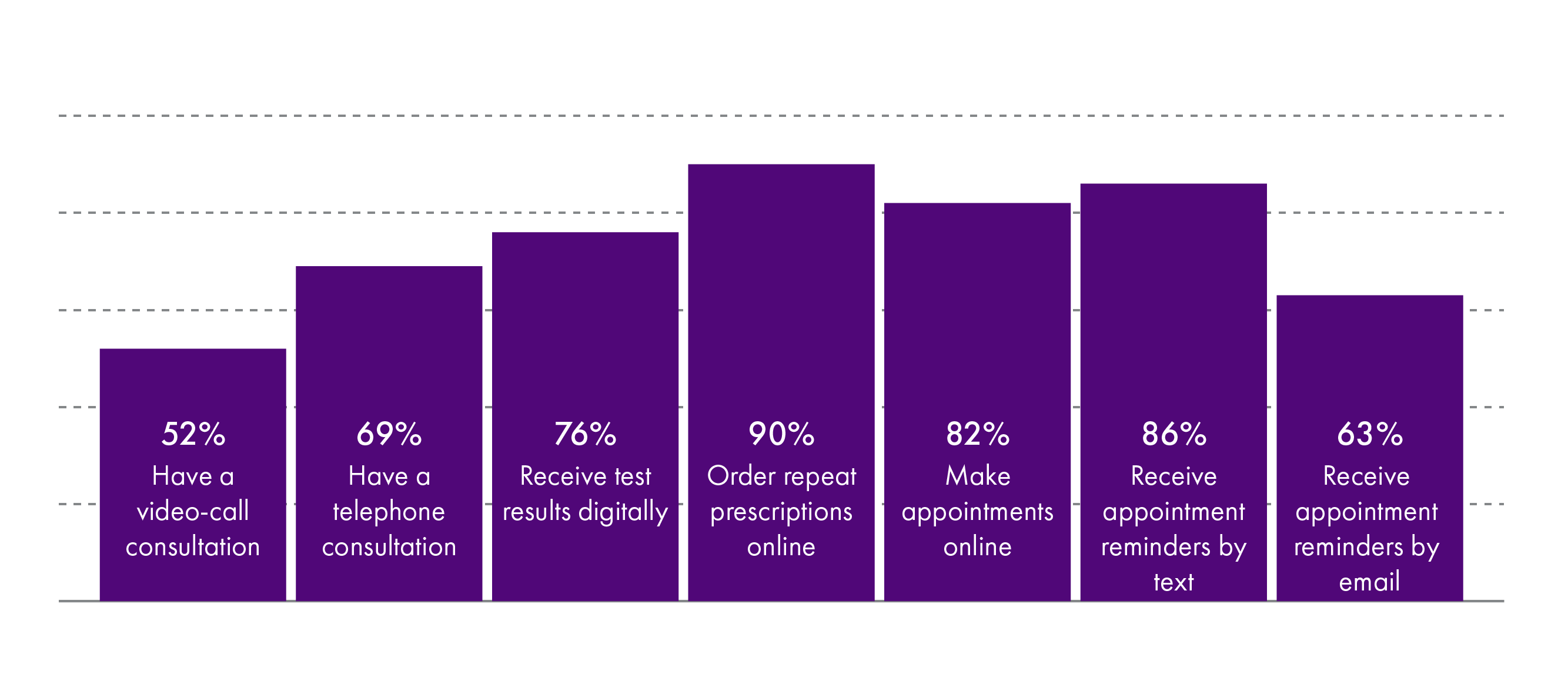
Up to 90% of survey respondents were happy to use technology to order repeat prescriptions with slightly less (82%) willing to make appointments on line, 86% would receive reminders by text and 63% by e-mail. 76% were happy to receive test results digitally, 69% to have a telephone conversation and just over half (52%) to have a video call consultation.
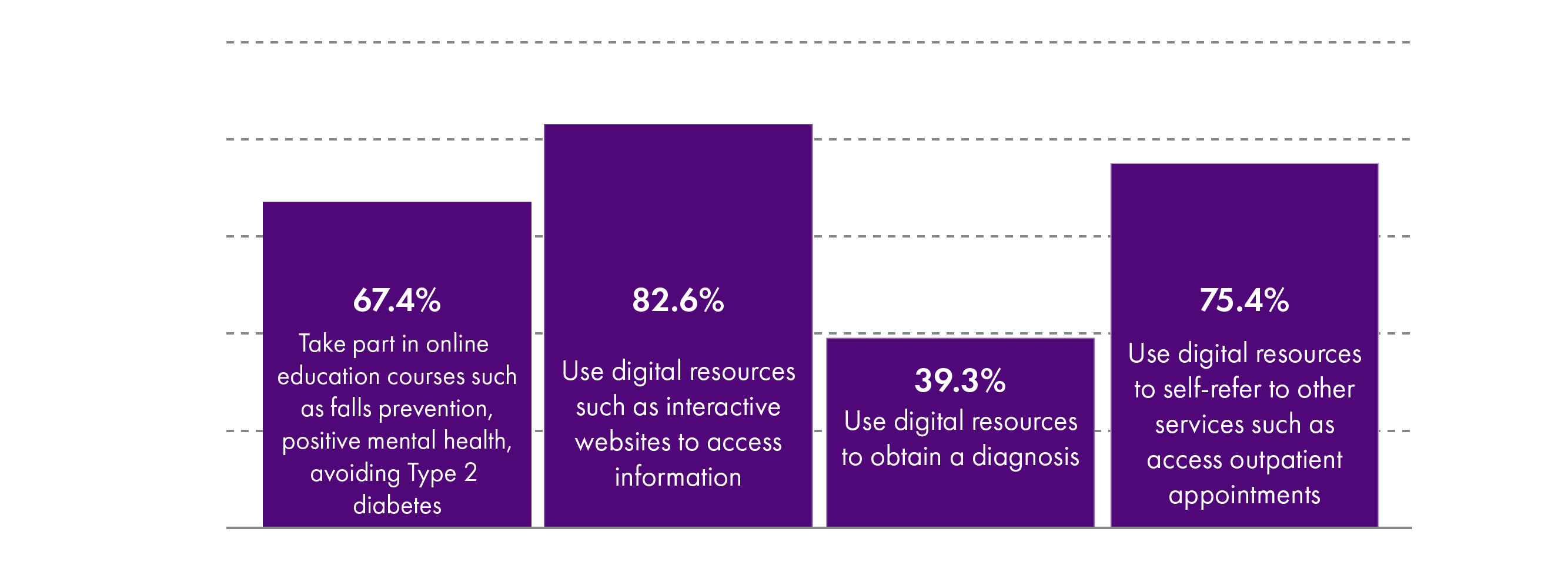
Over two thirds of survey respondents would be willing to take part in on-line health education, use digital resources to self-refer to other services such as outpatient appointments with over 82% content to use digital resources to access information. However fewer than 40% wished to use digital resources to obtain diagnosis.
Responses from the SYP recommended the use of e-mail, text and social media for appointments and prescriptions. They also recommended the use of Skype or FaceTime appointments with GPs in particular for those in rural/remote areas and with disabilities. They welcomed a greater use of opt-in healthcare App’s including one for mental health but also expressed reservations about App’s for medical diagnosis being mandatory.
Community wide approach to well-being
The priorities from the panel are;
Social prescribing – support for physical activity & addressing loneliness e.g. promoting walking groups, active social groups, activities making better use of greenspace
Don’t assume loneliness only affects older people. Use of neighbour networks.
Co-location of facilities – multi-use community facilities. Making use of community locations eg places of worship & social clubs, community hubs providing nutrition & cooking classes.
Teaching basic
life skills in schools, & how to access/use health services.
School nurses integrated into community services
Keeping people at home – using voluntary support for home care – or collective care in homely settings (so that staff can care for more people)
Survey responses while not looking at the above areas exactly expressed a desire for services in primary care to be expanded, especially testing and diagnostics as well as pain and weight management clinics.
Patient-centred approaches to accessing services
The priorities from the panel are;
Sustained relationships with health staff who know individuals
Greater engagement and consultation with patients about services
More effective triage for primary care services
Easily accessible information about and referral/signposting to services e.g. pop-up community opportunities for information/referral
Flexible appointment systems – routine access to evening/weekend appointments to fit lifestyle/working hours – designed to serve public not professionals.
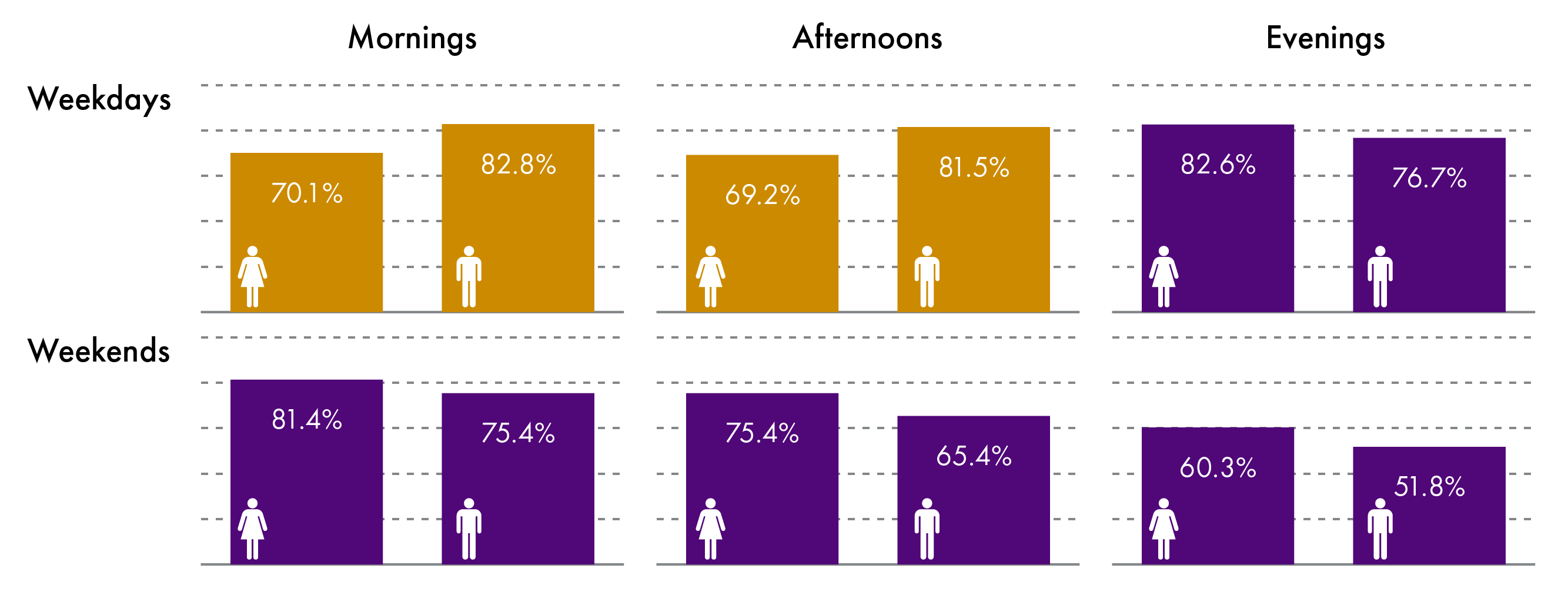
Survey responses showed high levels of satisfaction with existing week day primary care appointment times but over three quarters wanted evening appointments. Equally many wanted weekend appointments ranging from 51% in the evenings to 81% in the morning.
Survey responses wished for improvements in processes and responsiveness of Primary Care services and to see the most appropriate health professional. They also wanted better communications between primary and secondary care and greater opportunities to self-refer.
Service/workforce planning
The priorities from the panel are;
GP at heart of hub but with shared responsibility with other professionals for care and sign-posting – connection between the different professionals
More local and joined-up decision making
Better forward planning for workforce supply & demand, career development for NHS staff
Improved information sharing across all services
Greater use of patient records to plan future services.
Taking into account staff stress in planning staff-patient ratios, support for emotional needs of staff & listening to staff concerns before change happens.
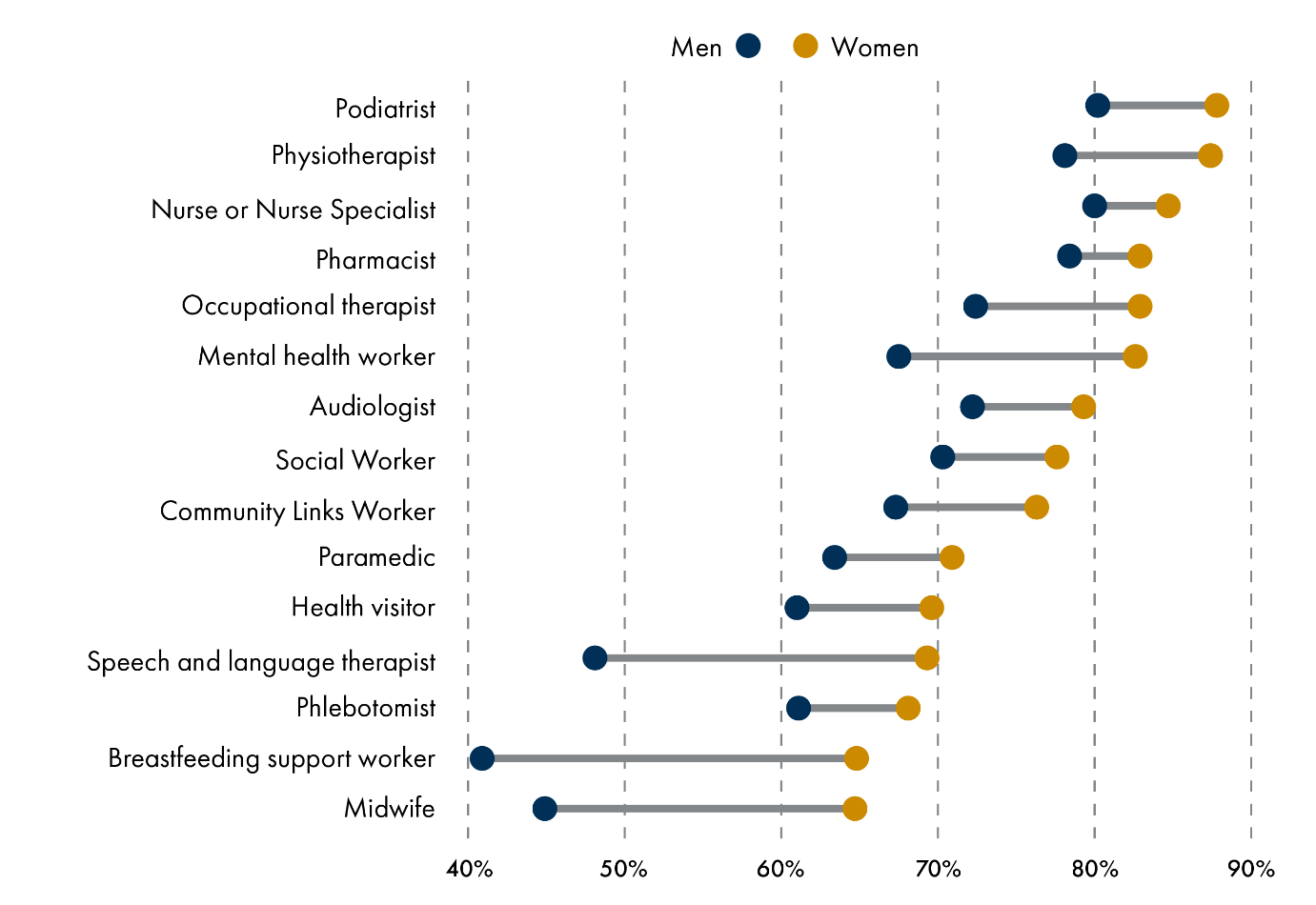
Those surveyed were asked if they would like to be able to see other health professionals without going through their GP and while results varied by sex with more women than men agreeing those who commented seemed content to be seen by other health professionals and to self-refer.
Survey responses also commented on the role of the receptionist as the “gatekeeper” to services and a need to improve triage services at surgeries. Other comments referred to stress levels of health staff and the need for more time to be dedicated to appointments.
Survey responses also highlighted differences between rural and urban services and concerns around centralisation of specialist services increasing barriers to access.
Comments from those surveyed expressed frustration about failings to share information although there was a split about who owned the data and the giving of consent to share.
Health & social care
The priorities from the panel are;
NHS to take over responsibility for social care from local authority
Improved planning across health & social care, shared IT systems.
Finance
The priorities from the panel are;
Use resources effectively – reduce waste, fewer managers, right resources in right places
Longer term funding for third sector services.
Survey questions were asked about the current model of funding GPs as independent contractors running their practices as small businesses. 79% indicated awareness of the model with 68% indicating it worked well or extremely well for them and 51% indicating it worked well or extremely well for the NHS. Panel members showed no interest in this aspect during their considerations.
Prevention focus
The priorities from the panel are;
Encouragement, education & incentives for health behaviour eg healthy eating, physical activity – with particular emphasis on deprived communities, addressing financial barriers
Universal health MOT for prevention/early intervention
DN profiling – using technology for prevention.
Focus money & promotion on early years (0-3) to reduce ACEs
Subsidised healthy food & healthy school meals
Mental health support/well being spaces in schools – NHS working with schools & employers to catch mental health situations quickly, mental health as part of teacher training
Prevention/early detection for dementia
Holding industry to account for health impact of products/services
Greater emphasis & new methods for public health promotion/education – using eg social media, heath TV channel.
Survey Panel responses included a desire for greater focus on prevention than treatment with regular health checks and advice provided. Many referred to mental health with a number seeing it as the main priority for primary care services.
The SYP had a recommendation that young people should be able to access specialist health support more easily through their GP especially a mental health worker.
Other comments
Two areas covered by the survey but not explicitly by the panels were the Scottish Government vision with which 77% agreed and out of hours services for which 78% who had used them (just under a third had) were satisfied or very satisfied.
Conclusion
From the surveys and the deliberations of the public panels there is clear public support for change in the way Primary Care is accessed and delivered. The public have indicated they want change and to experience the benefits of technology.
The public have universally indicated they want solutions and do not regard the status quo as an option.
In the second phase of our inquiry we look forward to hearing from the professions and those responsible for delivering services how they can react to what we have been told.
Annexe A - Analysis of Results
Methodology and rationale for the Inquiry
The launch of the survey in March 2019 coincided with the Committee’s announcement that it was embarking on an inquiry to look at primary care for the next generation. This inquiry is set in the context of health and social care integration, a new GP contract, Realistic Medicine and national primary care workforce planning and transformation.
It was agreed the inquiry would have a first phase devoted to gathering information, primarily centred on information from the public predominantly service users. The purpose of the initial phase being to find out from users what they wanted their primary care to look like. It was agreed this should attempt to move the debate on from the ideal local scenario for each individual to one which also reflects the reality of cost, impact and accessibility for all.
The inquiry is planned in two phases, the survey being part of the first phase, along with engagement with three public panels, which intends to consider public views, attitudes, and understanding before the second phase of the inquiry, which will start in the autumn. During the second phase, the Committee will hear from professional bodies, representing a wide range of stakeholders including professionals, the third sector and the Scottish Government.
Public Panels
The substantive aspect of the first phase has been the establishment of three randomly selected public panels in the East, West and North of Scotland. These have comprised deliberative workshops, which have included Members, to establish issues and concerns to inform the second phase. A separate report has been written about the work and outputs from the panels.
This unique approach has provided panels with information on how primary care is organised in Scotland, what is changing and has changed the NHS and social care landscape over recent years, and has delivered an informed, lay perspective on the future of primary care.
The intent was to acknowledge and illustrate that no government, local authority or health board starts with a ‘clean slate’ and has to plan in the context of existing policy, legislation, and societal circumstances.
The Panels, as groups of unconnected individuals, demonstrated the wealth of experience, the depth of engagement and understanding that is possible when taken through a process of being informed through a workshop model. Some of the members will be invited to a Committee meeting in the Parliament to consider the evidence heard during the second phase of the inquiry.
The Survey
The survey was launched at the beginning of March 2019 and was open till 30 April. There were 2,549 responses, mainly completed via the online link that was promoted through web and social media channels as well as through the Committee Outreach team, targeting third sector partners.
Hard copies of the survey were also made available to any person or group that requested them. The responses were then collated and included in the analysis.
What the survey is and is not
It is important to note that an online survey of this nature is not a scientifically rigorous study, with weighted samples from the Scottish population. It represents a self-selecting sample of people choosing to respond, and is intended to provide some views and opinions, from mainly ‘closed’ questions, about the experience and understanding of primary care in Scotland. The survey was anonymous, and we did not ask if the respondent worked in primary care or the NHS. The survey questions are annexed to this summary.
What did the survey tell us?
The following contains graphics created from the mostly quantitative data recorded and then a summary of a sample of the narrative responses to the final question on the survey: ‘In a sentence, please describe your wishes for the future of primary care’. This question produced the richest responses and later in this report these are summarised under the following themes that arose from the answers:
Access
Improved processes across primary and secondary care
Prevention, health promotion and early intervention
Resources, Privatisation, paying for services and means testing – the current model
Technology
The multi-disciplinary team and self-referral
Localisation of services and rurality
Communication across the NHS and primary care
Information sharing
Expansion of services
The Results
The Demographics
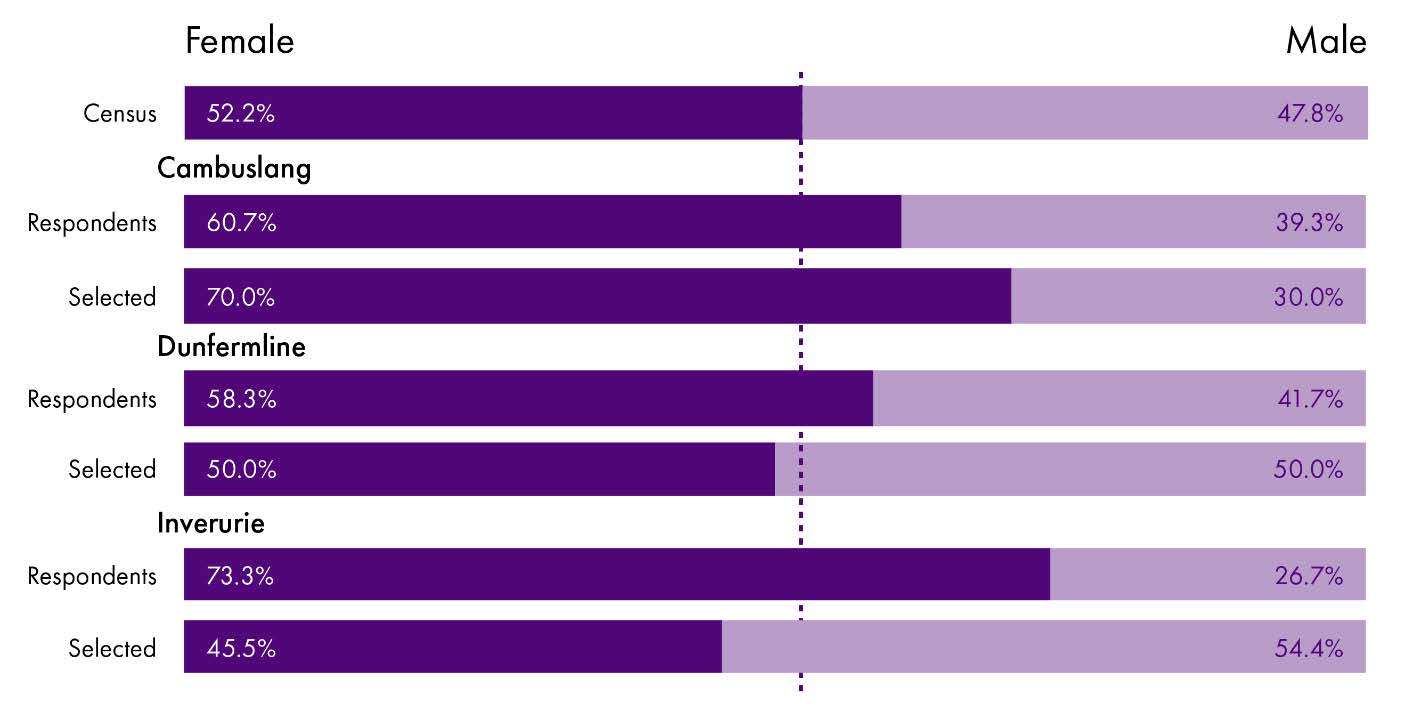
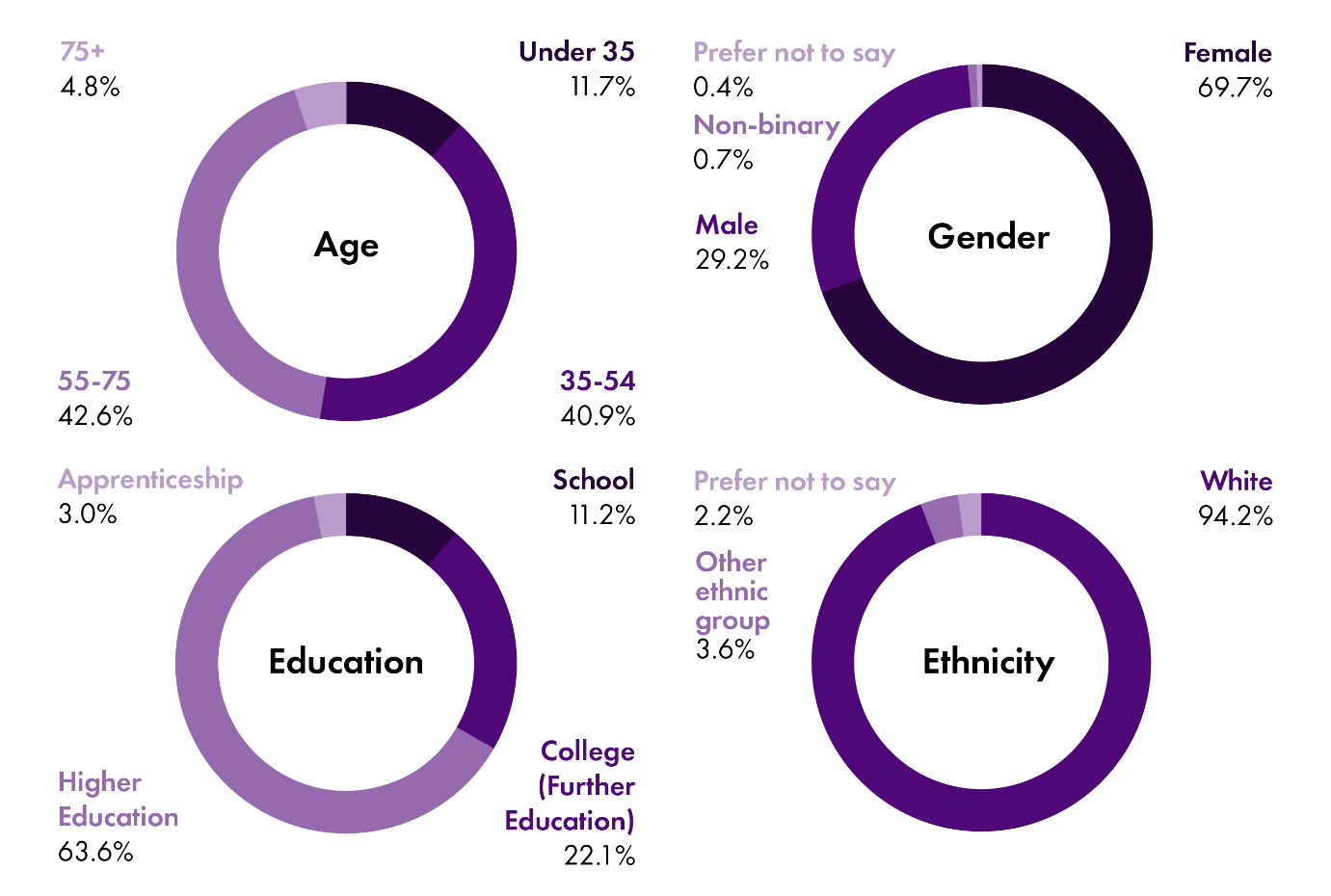
The highest proportion of respondents were women aged between 35 and 75. Most were white and had been educated to degree level
 The Scottish Parliament
The Scottish Parliament
The Primary Care vision
Respondents were asked:
‘To what extent do you agree with the Scottish Government’s Vision for primary care?’
‘The Scottish Government's vision is that “general practice and primary care at the heart of the healthcare system. People who need care will be more informed and empowered, will access the right professional at the right time and will remain at or near home wherever possible. Multidisciplinary teams will deliver care in communities and be involved in the strategic planning of our services”.
Respondents were provided with a link to the following National Performance Framework Outcome (Figure 1) ‘We are healthy and active’ which underpins the Primary Care Vision.
National Performance Framework Outcome  The Scottish Parliament
The Scottish Parliament
As can be seen below, 77% of respondents agreed with the Scottish Government’s Vision for primary care.
Scottish Government’s Vision for primary care 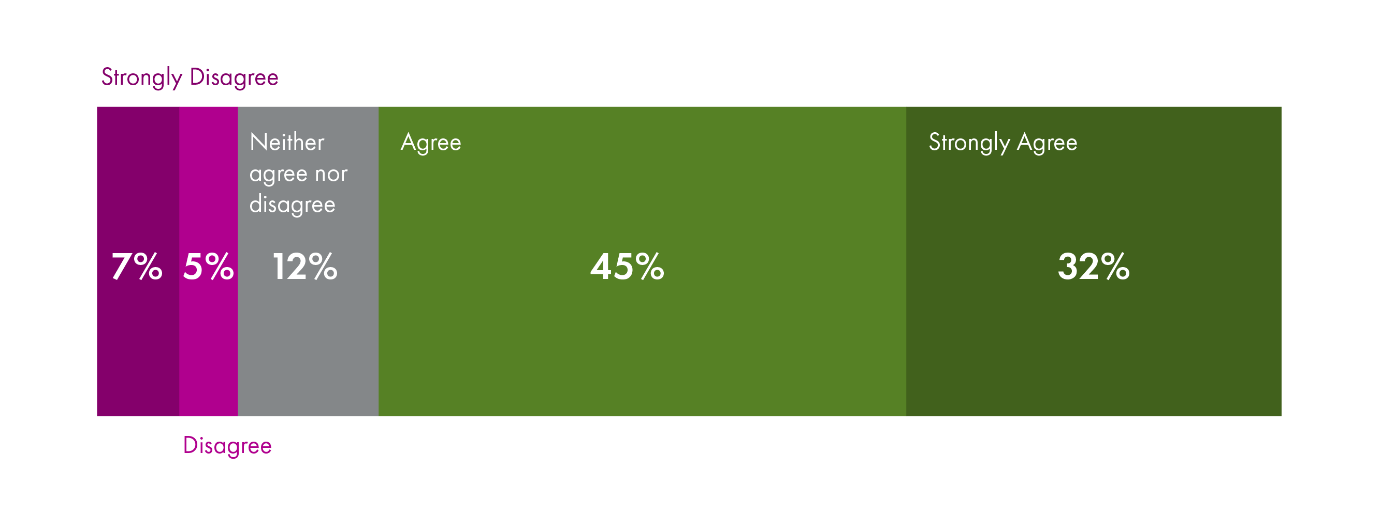 The Scottish Parliament
The Scottish Parliament
The Multidisciplinary Team
Respondents were asked:
‘Would you like to be able to see other health professionals in the primary care team without going through your GP?’
From Figure 3 below, it can be seen that more women than men answered yes to the question. It also appears that many are content to self-refer to the professional they deem most appropriate for their concern or condition.
 The Scottish Parliament
The Scottish Parliament
Respondents were also asked to suggest other professionals they would like to see based in primary care services. This resulted in 476 responses in free text. Suggestions included, not in any particular order:
Dietician or nutritionist
Paediatrician/paediatric nurse/paediatric mental health
Complementary therapies and a more holistic approach to health
Mental health staff – counsellors as distinct from health professional/psychologist
Dentist/orthodontist
Optometrist
Access to specialists such as dermatology, gynaecology/menopause
Benefits/debt adviser
Sexual health workers
Fitness adviser/weight management
Diagnostic testing – x-rays,
Advocacy
Pain management
Post-soft tissue trauma massage therapy
Drug and alcohol support
Continence and stoma care
Palliative care support
Third sector wellbeing initiatives – health promotion
Access to services
Respondents were asked:
‘When would you most like to be able to access primary care services?’
From Figure 4 below it can be seen that there is a high degree of support for the status quo, with daytime appointments. However, there was also a high level of support for weekday evening and weekend morning access, with men favouring weekday morning and afternoon appointments and women favouring weekday evenings and weekend day time appointments.
 The Scottish Parliament
The Scottish Parliament
Technology
Respondents were asked:
‘The Committee is interested in the role that technology can play in primary care. Would you be happy to:’
Figure 5 below shows that respondents were very much in favour of increasing the use of electronic communications in primary care, particularly to receive appointment reminders by text and ordering repeat prescriptions online. They were less keen to replace face to face with a video call consultation.
 The Scottish Parliament
The Scottish Parliament
Information sharing
Are you happy for your health information to be shared to help improve the health of people across Scotland?’
This question was seeking to ascertain the extent to which people were happy to share their personal medical and health data of people about the use of their health data in helping to plan, prioritise and organise public health services across Scotland. Most respondents were content with this, although fewer wanted their information shared with the NHS than with their GP or to support their own future health. Fewer, though still 61.1%, were happy to share information and data from health ‘apps’ and technology wearables.
 The Scottish Parliament
The Scottish Parliament
Accessing information
Respondents were asked: ‘In relation to digital information and advice, would you be happy to:
Figure 7 below suggests that respondents happy to use digital resources for communication and for accessing information for self-help. It is clear that fewer are comfortable with receiving a diagnosis using digital resources.
 The Scottish Parliament
The Scottish Parliament
Information sharing between professionals
Respondents were asked:
‘Do you think that your medical notes and relevant health information are always shared between relevant members of the primary care team to help co-ordinate the best care for you? (For example, between GP and Pharmacist or between GP and Dentist)’
Just over 50% of respondents thought that their notes were not shared. 26.5% thought that they were.
The next question asked if respondents were happy for their information to be shared in this way.
As can be seen from figure 8 below, a large majority were happy for relevant information to be shared across the primary care team.
Respondents were asked:
‘Are you happy for your relevant health information/notes to be shared across the primary care team to help co-ordinate the best care for you?’
 The Scottish Parliament
The Scottish Parliament
The following set of three questions asked about the current model of funding GPs: that most are independent contractors that run their practice as a small business, employing staff and are not directly employed by the NHS.
Respondents were then asked:
‘Since the start of the NHS, general practice has developed as an independent contractor model whereby many GPs are self-employed, employ practice staff and deliver services on behalf of the NHS rather than being direct employees of the NHS. Are you aware that the most GPs are self-employed and run their own practices?’
79% of respondents were aware that this is how the model works. The charts below show the extent to which respondents thought that it worked well as a model for the NHS and them and their families. More thought that it works well or very well for them and their families than it does for the NHS
How well does the model work for you and your family?’ 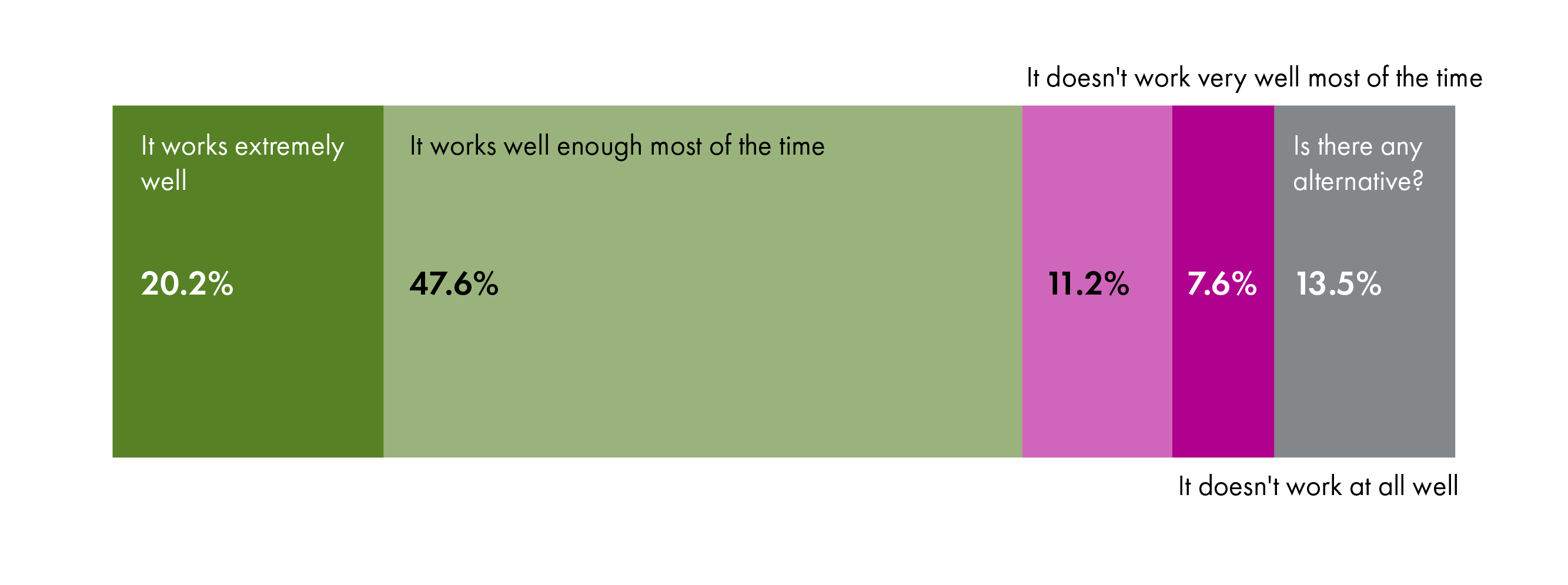 The Scottish Parliament
The Scottish Parliament
How well does the model work for the NHS’ 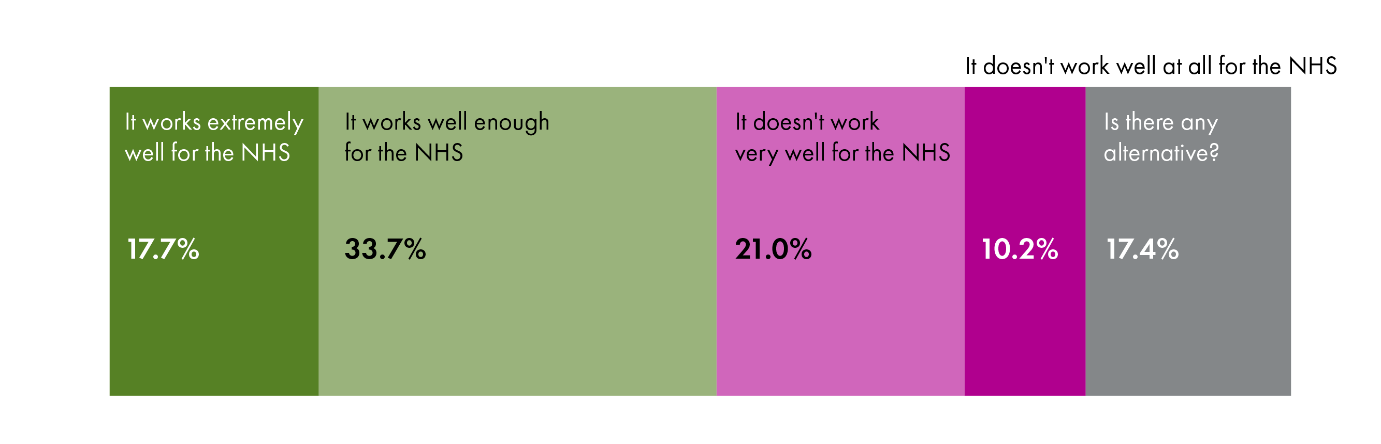 The Scottish Parliament
The Scottish Parliament
Out of hours
Respondents were asked:
‘Have you used out-of-hours (OOH) GP services in the last year?’
The responses to this question were broken down according to age to see if there was any marked difference in the age of those who use OOH services. Only 31% of respondents had used OOH services in the last year. The graphic below shows the age breakdown of those who had attended. When asked how satisfied people were with the service if they had used it, most were satisfied or very satisfied with the service.
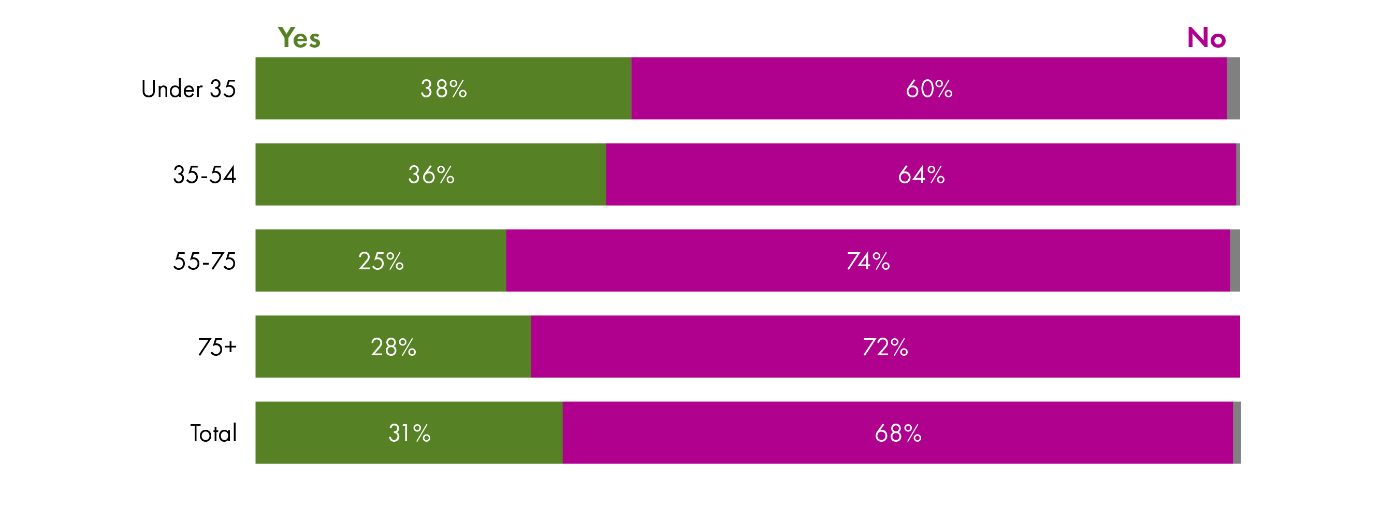 The Scottish Parliament
The Scottish Parliament
Planning Primary Care
Respondents were asked:
‘Do you want to be involved in planning how primary care is run or developed in your area?’
Most respondents expressed an interest in being involved in planning primary care in their area, but some did not feel in a position to do so currently. Because respondents were self-selecting, it is possible that respondents already had an interest in how primary care services are organised.
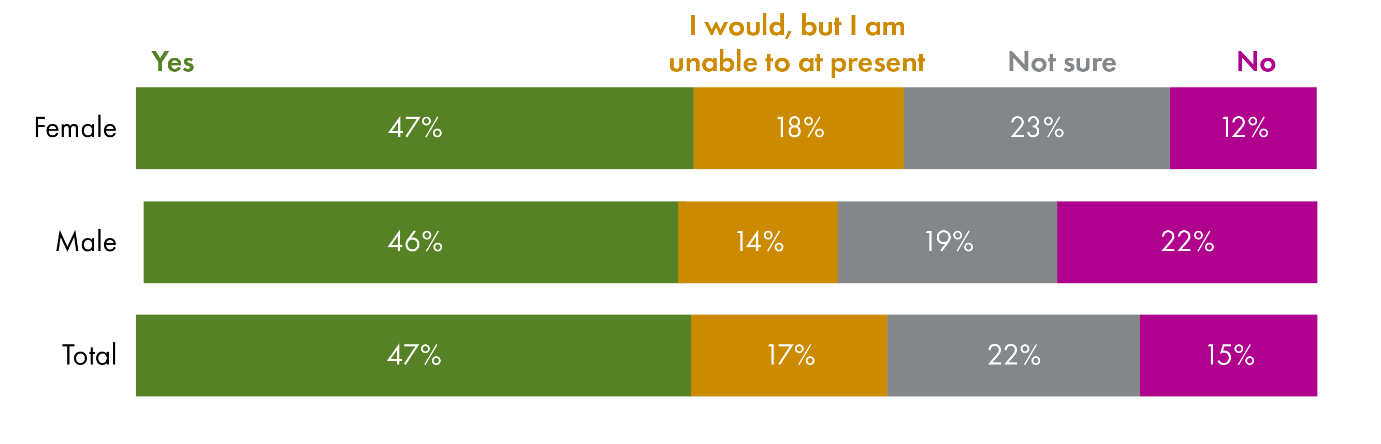
If people answered ‘yes’, ‘I would but’… or ‘not sure’ to Question 20 they were next asked:
‘How would you prefer to be involved? (People were invited to mark all that applied)
 The Scottish Parliament
The Scottish Parliament
Respondents were then asked:
‘How involved do you feel in how primary care services are run in your area?
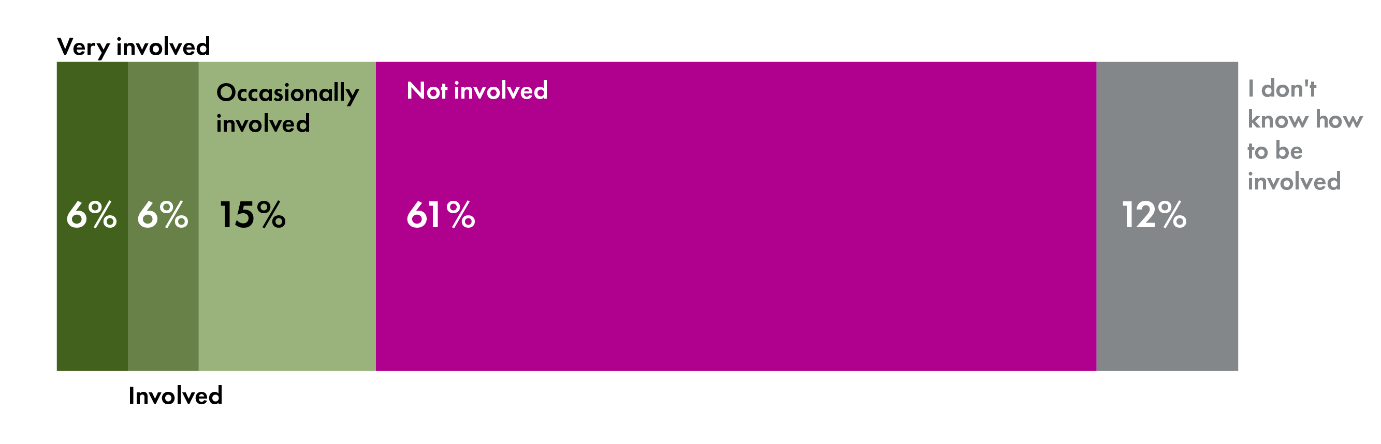
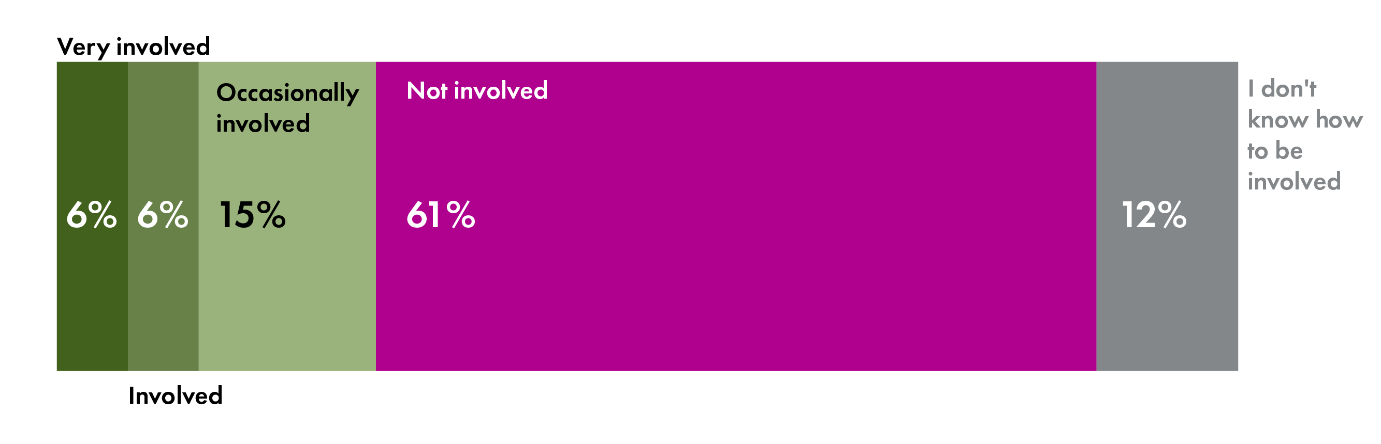
73% felt that they were not involved or did not how to be involved (61% and 12% respectively) and 27% felt involved.
Qualitative analysis of the final question
The final question of the survey was answered by 1793 people. The responses were sampled and key themes identified. Responses were coded into around 45 themes, and tallied for recurrences, that arose through the analysis. These themes have been grouped under broader headings below. Keyword searches of all the submissions were then carried out according to the identified themes in order to illustrate the range of views.
Respondents were asked:
‘In a sentence, please describe your wishes for the future of primary care’
I think we have a very good NHS in Scotland and most local GP practices run well. I do think though that dialogues at community level where communities that actively care offers an opportunity to beyond medicalised and treatment focus of health provision.
The Scottish Youth Parliament Survey
The Scottish Youth Parliament (SYP) also distributed two of the questions from the survey, as part of a more extensive survey, to young people aged between 12 and 25. 1,136 responses were received.
The SYP produced a comprehensive report, analysing the survey results, for the Health and Sport Committee which is annexed with this report. They conclude the report with the following recommendations.
Summary recommendations from SYP
The Scottish Youth Parliament recommends:
Young people should be able to access a specialist health support more easily through their GP, especially a Mental Health Worker.
In the future, healthcare appointments should be sent by email / text / social media and prescription notifications sent to your smartphone or tablet to benefit young people with busy lives.
Optional video services such as Skype or FaceTime (or similar video service) for a GP appointment should be considered for the future to support young carers, young people living in rural or remote areas as well as young people with disabilities or mental health problems, making it easier to attend a GP appointment.
Medical diagnosis App’s should not form a mandatory part of primary health care in the future due to concerns over mis-diagnoses due to the lack of physical assessment, miscommunication, accessibility and a lack of human interaction.
Opt-in healthcare App’s should be developed to help make young carer’s lives easier and a mental health App should be developed to empower young people with mental health difficulties.
Healthcare App’s should be developed through consultation with health professionals and patients; that these could be very useful for improving mental health outcomes; that security and privacy is ensured; that healthcare professionals and medicine keeps up with new technological developments; and that since healthcare Apps may not suitable for everyone, a flexible approach to their introduction should be adopted.
Annexe B - Submission from the Scottish Youth Parliament April 2019
Introduction
The Scottish Youth Parliament (SYP) represents Scotland’s young people. Our vision for Scotland is of a nation that actively listens to and values the meaningful participation of its children and young people. Our goal is to make this vision a reality, in order to ensure Scotland is the best place in the world to grow up.
Our democratically elected members listen to and recognise the issues that are most important to young people, ensuring that their voices are heard by decision-makers. We exist to provide a national platform for young people to discuss the issues that are important to them, and campaign to effect the change they wish to see.
SYP’s Values are:
Democracy – We are youth-led and accountable to young people aged 12 to 25. Our democratic structure, and the scale of our engagement across Scotland, gives us a mandate that sets us apart from other organisations.
Rights – We are a fundamentally rights-based organisation. We are passionate about making young people aware of their rights, and ensuring that local and national government deliver policies that allow those rights to be upheld.
Inclusion – We are committed to being truly inclusive and work tirelessly to ensure the voices of every young person from every community and background in Scotland are heard.
Political Impartiality – We are independent from all political parties. By working with all stakeholders, groups, and individuals who share our values, we can deliver the policies that are most important to young people.
Our Approach
SYP welcomes the opportunity to respond to the ‘What does primary care look like for the next generation’ inquiry by the Health and Sport Committee (hereinafter referred to as ‘the Committee’) at the Scottish Parliament. This response is based on the findings of co-designed questions in the #WhatsYourTake survey prior to SYP’s 68th National Sitting in Dalkeith, Midlothian, and the consultation workshop which took place on Sunday 17th March 2019.
The workshop was attended by thirteen young people, called ‘Health Care for the Next Generation’ and co-produced by SYP including SYP’s Health and Wellbeing Committee Convener Alice Ferguson MSYP, the Health and Sport Committee, the Scottish Parliament’s Community Outreach Team and Committee Engagement Unit.
Through a series of interactive activities, MSYPs gave their views on the future of primary health care which are summarised below. By way of icebreaker, they each identified two types of professionals they think should work in a GP office if it had only two spare rooms. They moved on to a ‘walking debate’ on the pros and cons of technologies for the future of health care (video services and medical diagnosis apps) and then took part in a ‘Dragon’s Den’ activity where in sub- groups they discussed ways in which technology could help provide primary health care in the future and pitched ideas to the plenary, voting with sticky notes on their favourite idea.
 The Scottish Youth Parliament
The Scottish Youth Parliament
The #WhatsYourTake online survey was open from 15th February until 20th March, gathering 1136 responses from young people aged 12-25 across Scotland, from all 32 local authorities and our 11 national voluntary organisations and various others representing a diverse range of communities of interest and lived experience (including different faiths, disabilities, care and carer experience, LGBTQI+, young farmers and young offenders).
It asked respondents (with both questions including a series of options as outlined below).
Which of the following technologies would you be happy to use to access health care in the future?
Using Skype or FaceTime (or similar video service) for a General Practitioner (GP) appointment.
Having appointments sent by email / text / social media.
Using medical diagnosis Apps – with results sent directly to GP or hospital.
Receiving medical diagnostic test results by email / text / social media.
Having prescription notifications sent to your smartphone or tablet.
Using online forums to ask generalhealth questions of your GP, dentist or other health professional.
Share information from health technology wearables, such as 'fitbits', with the NHS.
Other (please specify):
Which health professionals would you like to be able to see more of without having to go through your GP? (The survey included brief descriptions of these roles).
Pharmacist.
Physiotherapist.
Practice Nurse.
Health Visitor.
Midwife.
Community Link Worker.
Occupational Therapist.
Speech and Language Therapist.
Mental Health Worker.
Paramedic.
Breastfeeding Support Worker.
Social Worker.
Other (Sexual Health Specialist Nurse, Alcohol and Drug Worker).
Background information of survey respondents
The majority of respondents are at school (87%) and aged 12-14 (49%) and 15-17 (42%). 55% of respondents are female, 45% were male, 2% identified as non-binary and 1% prefer to use their own term. 13% of respondents belong to black, Asian and minority ethnic groups.
Which health professionals would you like to be able to see more of without having to go through your GP? (see above for options in full).
Most survey respondents would like to be able to access a Mental Health Worker through their GP. Including thirty-three collective classroom responses, support for this option was at 59%. Pharmacist (40%) and Physiotherapist (42%) were the next popular options.
I feel mental health support NEEDS to be made easier to access for everyone, especially young people. If someone wants to talk about their mental health they should be able to access a specialist in a quick and easy manner without having to go through multiple channels and waitlists beforehand.
Other options specified / suggested in the onlinesurvey included ‘SexualHealth Nurse / Specialist’, ‘Alcohol and Drugs Worker’, ‘Optician’, ‘Podiatrist’, ‘Chiropractor’ and ‘Gender Identity Clinics.
Some respondents detailed their answers expressing that ‘GPs perhaps shouldn't be dealing with cases of mental health’; they ‘should retain their role as gatekeeper to other services’; attending the Doctor’s is a long process; and peer-support for mental health is preferable to seeing a GP.
The workshop participants in their icebreaker identified Mental Health Worker and Practice Nurse as their preferred medical professionals to be at their GP’s office if it had only two spare rooms, even though support for the ‘Practice Nurse’ was low (17%) on the online survey.
Other options which received at least one vote were:
Paramedic (this option was preferredby a young carer who has neededparamedics close by in the past).
Midwife (for rural areas, withouteasy access to the maternity unit at a hospital, this could increase safety – ‘they are specialists’)
Occupational Therapist - (increased accessibility could help get people who have had difficulties get back into work. One young person commented that services are too spread out).
Community Link Worker – (‘they have more of an all-round insight into your health’ and could link up with social work which would be really beneficial to the community.)
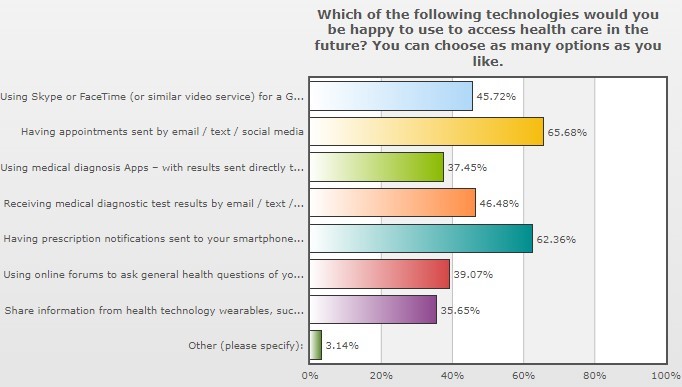
Which of the following technologies would you be happy to use to access health care in the future?
 The Scottish Youth Parliament
The Scottish Youth Parliament
As can be seen above, having appointments sent by email / text / social media and prescription notifications sent to your smartphone or tablet were the preferred responses from the #WhatsYourTake survey. "Having appointments and prescriptions sent through texts/notifications would be a huge help to young people with busy lives".
In the ‘other please specify’ comments box (chosen by 3.14% of respondents), respondents suggested postal communication in cases where access to internet is lacking, online or App appointment booking facilities and official NHS forums.
Other comments included views that young people would prefer to have a face-to-face Doctor’s appointment or personal / human interaction, concerns over access to WiFi in rural communities and by older people, and lack of access to ‘fitbits’, for example:
"Using technology takes away the human aspect of health."
"Though ‘fitbits’and the like could be beneficial, not everyonehas access to them, so carewould have to be taken to ensure the system doesn’t rely on them."
Views were provided that ‘Apps have been shown to be inaccurate and cannot replace assessment by a qualified healthcare professional’ and ‘people may need support when they find out certain results.’ Someone suggested an opt-out/opt-in function for receiving prescription notifications sent to their smartphone or tablet. Security concerns were also raised as regards hacking and prescriptions being modified which could seriously risk the recipient’s health. Many young people related their answer to their lived experience or that of their families’
E.g. I have type 1 diabetes it would be great if the data gathered from my smart device for example from my mobile phone or from my Apple Watch could instantly be shared on Diasend so my diabetes team at Ninewells Hospital know instantly know what is going on with my diabetes.
I think that the influence of technology would greatly benefit many people, perhaps those who are elderly and who are not as mobile as others. I also think that these services would enable people (eg. receptionists, ect.) who work for the NHS more time to be spent on more important issues and would benefit the running of the NHS in general.
Those endorsing online forums liked the anonymity of being able to inquire about an embarrassing health issue online first, in order to get the advice and confidence to see their Doctor
During the walking debate at the workshop, MSYPs supported video services such as Skype or FaceTime (or similar video service) for a General Practitioner (GP) appointment with six MSYPs voting ‘for’ this option, with three MSYPs ‘neutral’ and ‘against’ respectively. MSYPs felt video services favoured young people living in rural or remote areas as well as young people with disabilities or mental health problems, making it easier to attend a GP appointment.
Those who chose to be ‘neutral’ felt that this already happens in some areas, and were not sure if this option would viable in terms of affordability. Those ‘against’ video services felt that they would miss the personal 1:1 interaction; that physical interaction would be difficult and could affect diagnoses resulting in more second opinions being sought; it could result in greater waiting times due to connectivity problems; there could be issues in areas with a lack of internet; and people with anxiety may not want to access video services.
MSYPs were also predominately against having medical diagnosis Apps with nine voting ‘against’, one ‘neutral and two ‘for’. They expressed concerns over misdiagnoses through miscommunication and that information given objectively through an app could ‘make symptoms seem so much more serious than they actually are. There was discussion over how seriously a diagnosis provided in this way would be taken, with one young person saying, ‘as long as you don’t take it as gospel’. There were concerns over whether the NHS would be permitted to share data in this way, however, others pointed to ‘Patient Access’ for booking appointments used in some practices which has a unique log-in, and suggested that this could be part of any App.
Arguments for Apps highlighted the benefit particularly for young carers, as they are not always able to speak to a professional when they need to, especially when they are caring for themselves and sometimes multiple family members. Some MSYPs felt like an app would give reassurance to those not comfortable with speaking to health professionals or want to find out information they would not require a full appointment for. MSYPs thought it could cut down waiting times.
On healthcare Apps more generally, MSYPs recommended that Apps be developed through consultation with health professionals and patients; that these could be very useful for improving mental health outcomes; that security and privacy is ensured; that healthcare professionals and medicine keeps up with new technological developments; and that since healthcare Apps may not suitable for everyone, a flexible approach to their introduction should be adopted.
Two ideas in the dragon’s den activity received the most votes. These were the following, in order of preference of the participants who voted for their preferred option after the presentations using sticky dots:
1. A Mental health app (Received 8 votes)
An App could be developed that you input quantitative data about how your mental health is. This would track if your wellness is increasing or decreasing using a daily log and daily mood scores. It would offer immediate support, for example, if you’re having a panic attack, it would offer tools to help with that. It would contain music / playlists to help you when you are feeling distressed. Your GP / Mental Health Nurse would have access to it to check in on you without an appointment. This would ultimately be a prescribed safe space to take with you wherever you go. It will allow young people to physically see themselves improving, which is empowering
2. ‘multifunctional health App’ (Received four votes)
This App would contain a sleep, period, mood, blood pressure tracker, and a medication list and notifications to take medication as required. You would be taking control of your own health using data, which you would be happy to share with health professionals. By using the App, you knowingly agree to consent to your data being shared with health professionals. You would be empowered, accountable to yourself and in control – this could improve self-help so you visit the Doctor’s less, but also provide them with more information about your health.
The Scottish Youth Parliament recommends:
Young people should be able to access a specialist health support more easily through their GP, especially a Mental Health Worker.
In the future, healthcare appointments should be sent by email / text / social media and prescription notifications sent to your smartphone or tablet to benefit young people with busy lives.
Optional video services such as Skype or FaceTime (or similar video service) for a GP appointment should be considered for the future to support young carers, young people living in rural or remote areas as well as young people with disabilities or mental health problems, making it easier to attend a GP appointment.
Medical diagnosis App’s should not form a mandatory part of primary health care in the future due to concerns over mis-diagnoses due to the lack of physical assessment, miscommunication, accessibility and a lack of human interaction.
Opt-in healthcare App’s should be developed to help make young carer’s lives easier and a mental health App should be developed to empower young people with mental health difficulties.
Healthcare App’s should be developed through consultation with health professionals and patients; that these couldbe very useful for improvingmental health outcomes; that security and privacy is ensured; that healthcare professionals and medicine keeps up with new technological developments; and that since healthcare Apps may not suitable for everyone, a flexible approach to their introduction should be adopted.
Annexe C - Primary Care Public Panels
In March 2019, the Health & Sport Committee of the Scottish Parliament began an inquiry into the question: What should primary care look like for the next generation?
Primary Care is generally the first point of contact with the NHS (except for Accident and Emergency) for most people in Scotland when they need to access healthcare. This includes contact with many community-based services and healthcare professionals as well as a number of non-clinical roles such as practice receptionists and managers and community link workers.
The first part of the inquiry focused on gathering views and experiences from the public and especially people who use primary care services across Scotland. To help inform the first stage of the inquiry, the Committee agreed to establish three public panels in the west, east and north of Scotland to consider the question and offer ideas. The panels were designed to give a diverse group of the public the chance to learn about the subject and to work together to come up with ideas to share with the committee on how primary care could meet their needs in the future.
Panel 1 with 10 participants in Cambuslang, South Lanarkshire  The Scottish Parliament
The Scottish ParliamentPanel 2 with 14 participants in Dunfermline, Fife  The Scottish Parliament
The Scottish ParliamentPanel 3 with 11 participants in Inverurie, Aberdeenshire  The Scottish Parliament
The Scottish Parliament
Who took part?
Parliament staff worked with a not-for-profit organisation, the Sortition Foundation, to recruit a randomly selected and stratified sample for each panel, based on 2011 Scottish Census data.
 The Scottish Government
The Scottish Government
Invitation letters from the Committee Convener, Lewis MacDonald MSP, were sent to 2500 residential households in each area, selected at random from the Royal Mail‟s address database. Recipients were invited to register their interest in participating and the final groups were selected to be broadly representative based on gender, age and educational attainment level.
Panel members received travel expenses and a participation fee of £100 in recognition of the time and commitment they gave. The payment of expenses and the participation fee are key ways of removing barriers to participation and ensuring that seldom-heard voices are included in the process.
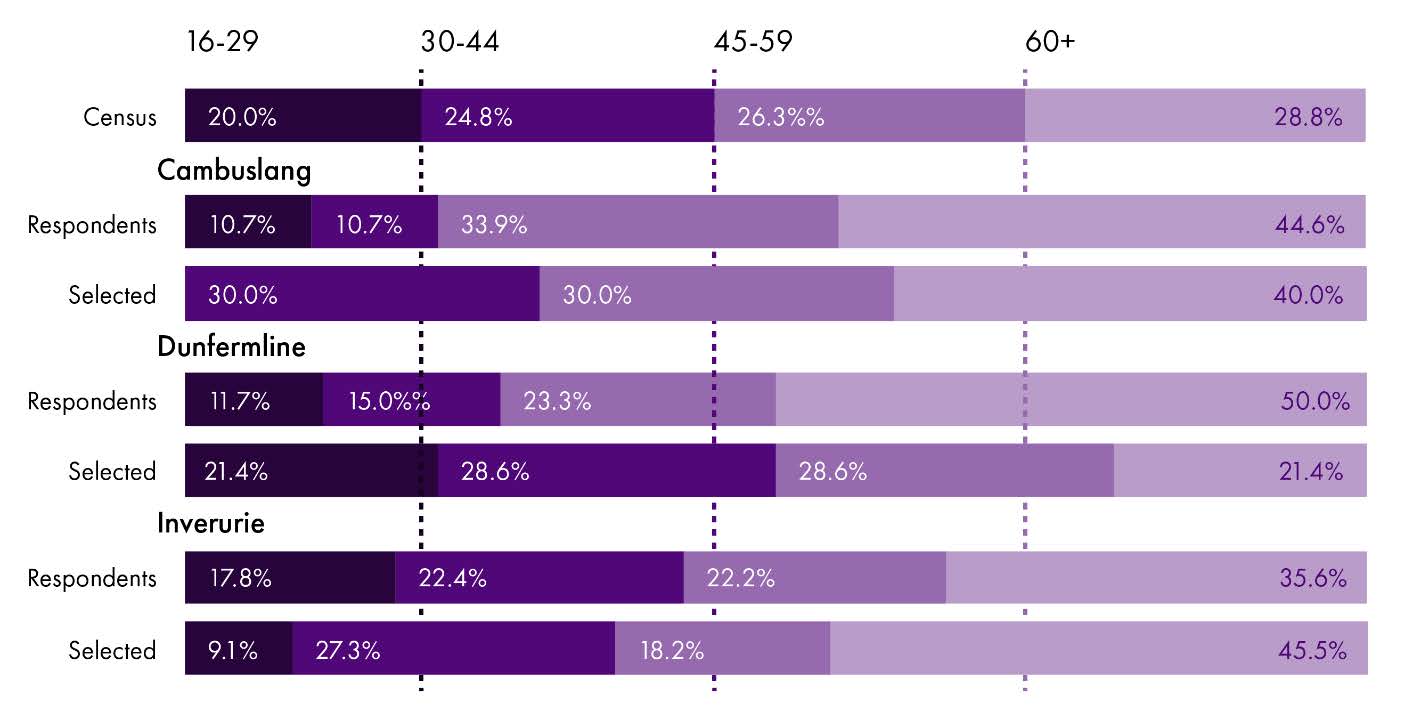
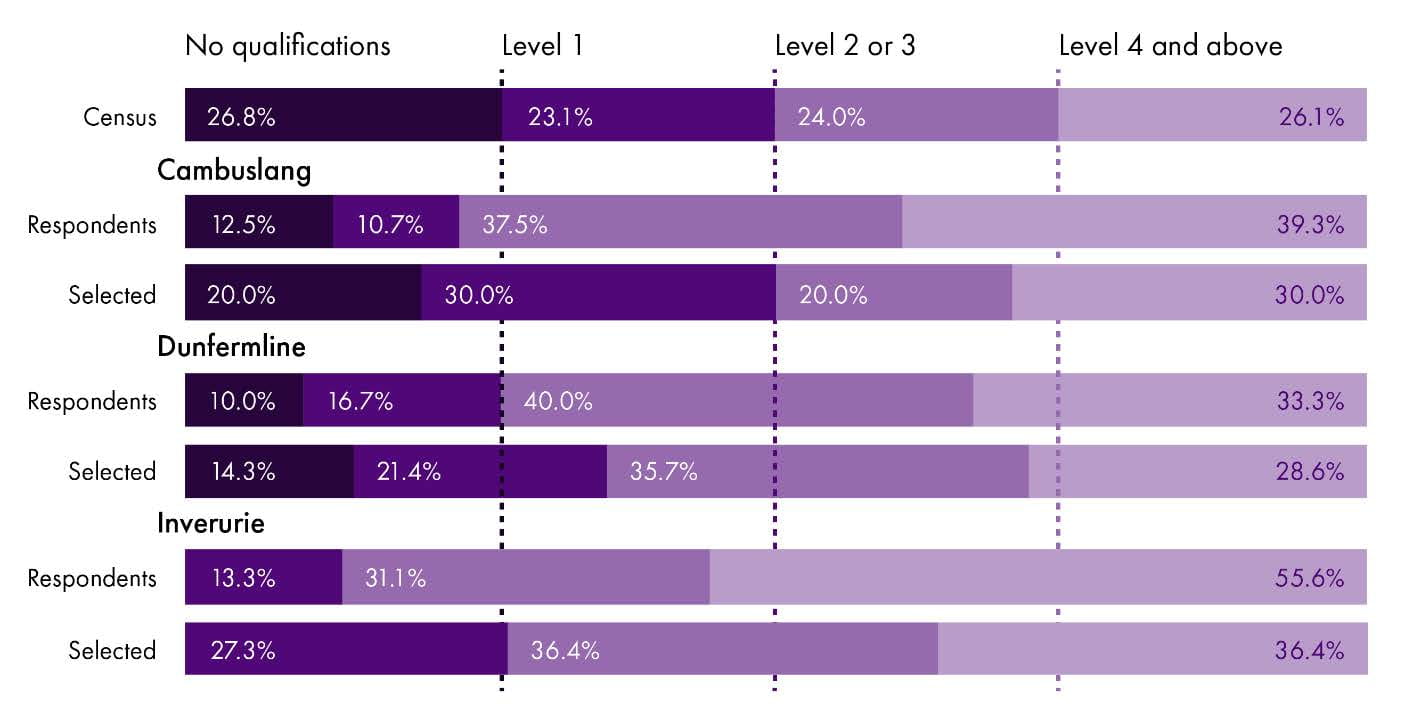
Response rates were relatively low (from 1.8% for Inverurie to 2.4% for Dunfermline) which made it difficult to match the sample as closely as we would have liked to Scottish census data. For example, in Inverurie there were no respondents from the “no educational qualifications” category, while in Cambuslang no one was able to attend in the 16-29 category. Even so, the approach taken meant that we were able to include more young people, and people from a wider range of educational backgrounds.
Composite demographic data of all three areas based on age, education and gender
The Scottish ParliamentThe Scottish ParliamentThe Scottish Parliament
Day 1
At the start of day 1, we asked participants what one word came to mind when they thought of the Scottish Parliament. Responses ranged widely, both positive and negative, demonstrating that the groups came together with diverse attitudes to the Parliament. Each group then agreed their own conversation guidelines to ensure that discussions were positive and respectful.
 The Scottish Parliament
The Scottish Parliament
Day 1 was primarily for learning about primary care and current policies. Expert input was provided by a researcher from the Scottish Parliament Information Centre (SPICe) and by Jill Mitchell, Chief Executive of CBC Health Ltd in Gateshead, who brought experience of service re-design and innovation in general practice.
Panel members learned about the range of services included within primary care, funding, Health and Social Care integration and the Scottish Government‟s vision for the future of primary care. They also heard a little about alternative models from elsewhere. The panels considered together why this issue is important for them and their families and what might get in the way of delivering the vision.
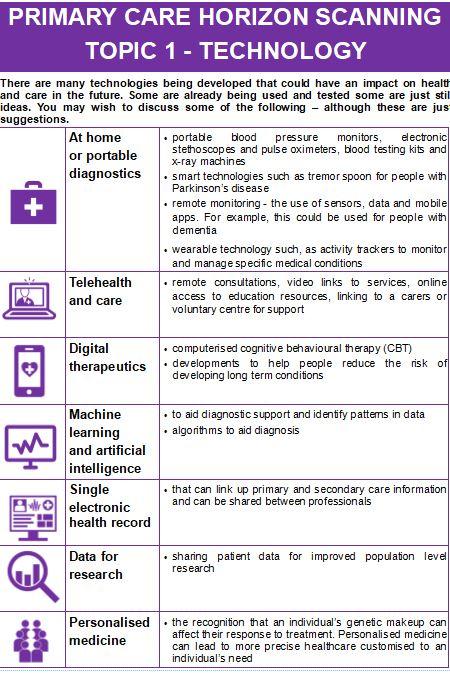
Day 1 ended with a horizon scanning activity thinking about future possibilities in areas such as technology, self-care and volunteering.
 The Scottish Parliament
The Scottish Parliament The Scottish Parliament
The Scottish Parliament
Day 2
On day 2, the panels were joined by MSPs from the Committee. The main activity was a creative mapping exercise to think about how the groups would like future services to be designed to address the health and social needs in their communities.
Cambuslang The Scottish ParliamentDunfermline  The Scottish Parliament
The Scottish ParliamentDunfermline  The Scottish Parliament
The Scottish ParliamentInverurie  The Scottish Parliament
The Scottish Parliament
Cambuslang
 The Scottish Parliament
The Scottish Parliament The Scottish Parliament
The Scottish Parliament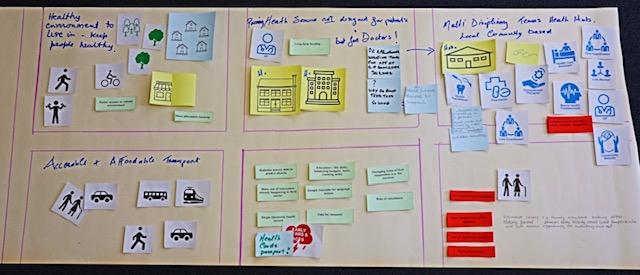
Dunfermline
 The Scottish Parliament
The Scottish Parliament The Scottish Parliament
The Scottish Parliament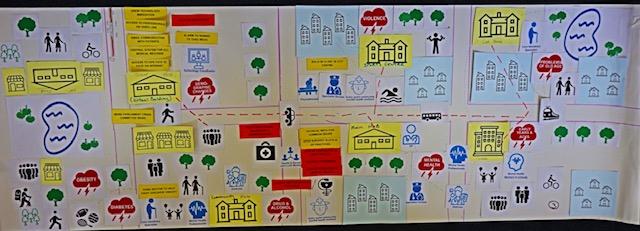 The Scottish Parliament
The Scottish Parliament
Inverurie
 The Scottish Parliament
The Scottish Parliament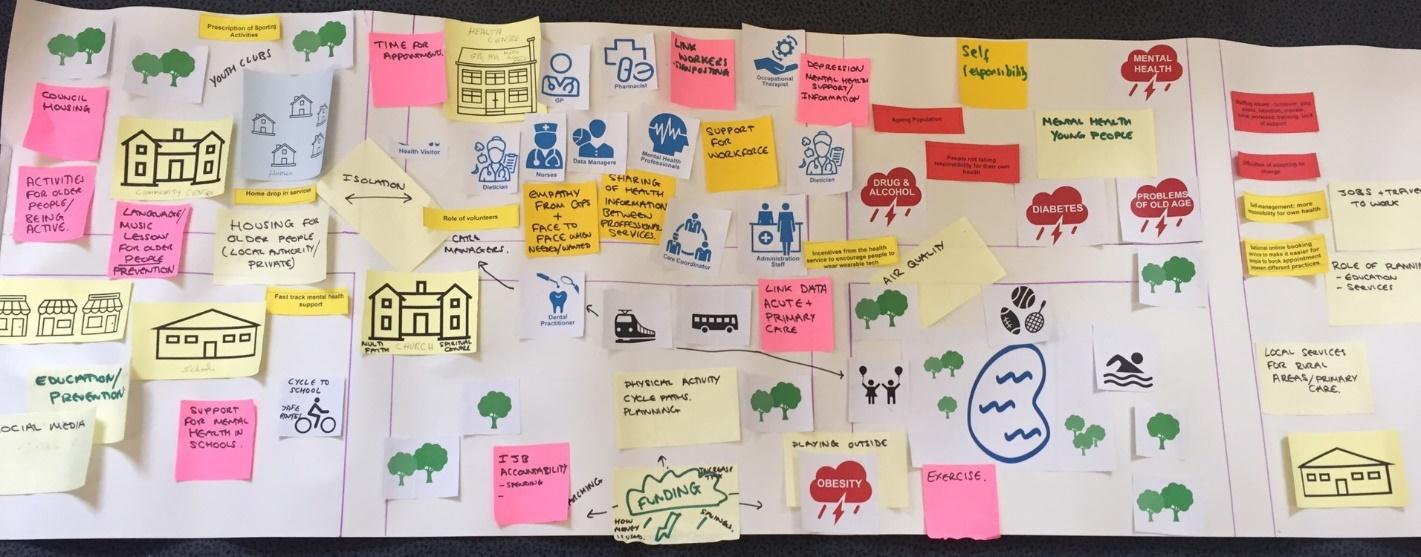 The Scottish Parliament
The Scottish Parliament
The groups then worked together to agree the priority themes and questions that they would like to feed into the next phase of the committee's inquiry.
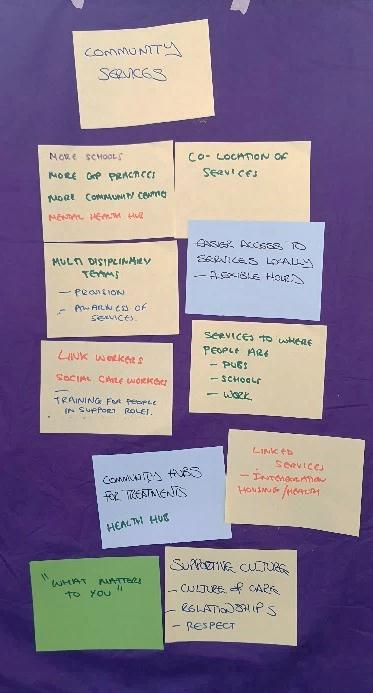 The Scottish Parliament
The Scottish Parliament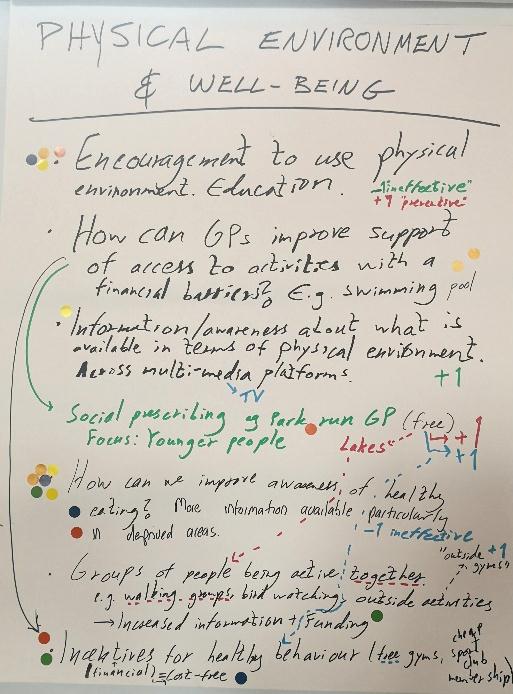 The Scottish Parliament
The Scottish Parliament
Evaluation
The panels are being evaluated by Dr Stephen Elstub from the University of Newcastle, a research specialist in deliberative engagement. Participants were asked to complete a survey at the beginning of the first day and the end of the second one. A researcher from Dr Elstub‟s team observed both Dunfermline panels. The evaluation report will be available after the summer and will allow us to understand in more detail the background and diversity of the group and their experience of taking part in the panels.
What did the panels conclude?
Full conclusions from each panel are in Appendix 1. Although each panel came up with its own unique set of themes & priorities, it is possible to identify a number of areas which were consistently identified and/or strongly prioritised.
Theme Priorities Use of technology Electronic patient record, shared with all relevant professionals – single set of records integrated across all care services – consistent platform used for electronic test results, correspondence, etc.
Ability to contact health professionals by email, schedule appointments online and hold consultations via video link
Using technology/wearables to monitor health e.g. blood pressure, diabetes and sharing information with relevant professionals
Community wide approaches to wellbeing Social prescribing – support for physical activity & addressing loneliness, e.g. promoting walking groups, active social groups, activities making better use of green space
Need to not assume loneliness only affects older people. Use of neighbour networks
Co-location of facilities – multi-use community facilities. Making use of community locations, e.g. places of worship, social clubs, community hubs providing nutrition and cooking classes
Teaching basic life skills in schools and how to access/use health services
School nurses integrated into community services
Keeping people at home: using voluntary support for home care – or collective care in homely settings (so that staff can care for more people)
Patient-centred approaches to accessing services Sustained relationships with health staff who know individuals
Greater engagement and consultation with patients about services
More effective triage for primary care services
Easily accessible information about and referral/signposting to services, e.g. pop-up community opportunities for information and referral •
Flexible appointment systems – routine access to evening and weekend appointments to fit lifestyle/working hours – designed to serve public not professionals
Service & workforce planning GP at heart of hub but with shared responsibility with other professionals for care and sign-posting – connection between the different professionals
More local and joined-up decision making
Better forward planning for workforce supply and demand, career development for NHS staff
Improved information sharing across all services
Greater use of patient records to plan future services
Taking into account staff stress in planning staff-patient ratios, support for emotional needs of staff and listening to staff concerns before change happens
Health & social care Improved planning across health & social care, shared IT systems
NHS to take over responsibility for social care from local authority
Finance Use resources effectively – reduce waste, fewer managers, right resources in right places
Longer term funding for third sector services
Prevention Focus Encouragement, education and incentives for healthy behaviour, e.g. healthy eating, physical activity – with particular emphasis on deprived communities, addressing financial barriers
Universal health MOT for prevention/early intervention
DNA profiling – using technology for prevention
Focus money and promotion on early years (0-3) to reduce ACEs
Subsidised healthy food and healthy school meals
Mental health support/wellbeing spaces in schools – NHS working with schools and employers to catch mental health situations quickly, mental health as part of teacher training
Prevention/early detection for dementia
Holding industry to account for health impact of products/services
Greater emphasis & new methods for public health promotion/education – e.g. using social media, heath “Netflix” channel
Appendix 1
Cambuslang
NB: Dots represent how the participants rated the ideas at the end of the day. Each had 10 sticky dots to place next to their top priorities across the themes.
PREVENTION PRIORITIES Other issues raised Organisations to work together and share best practice
Wellbeing spaces within schools supporting vulnerable students
Big link to education
Homeless people living on streets – more premises where they can find accommodation
In schools – teach basic life skills, i.e. nutrition, family budget, basic cooking skills
Less short-term fire-fighting to long term fundamental change
NHS work with employers, schools, etc to catch mental health situations quickly
Importance of involving third sector in service planning
Community / health hubs promoting prevention messages
Promotion of self-management of long-term conditions
Need for early intervention and prevent duplication
Mental health – quicker access to primary health care
Access for all to activities – sport, physical activity, art, drama, music
Support BME communities – equality language
Safe consumption (of opiates) facilities aren‟t just about taking drugs – it‟s about connecting – Hep C/HIV testing, mental health support, access to services and caring for humans
USE OF TECHNOLOGY AND INFORMATION SHARING PRIORITIES Other issues raised Technology to assist translation services
Portable defibrillators in communities – and training in using them
Diabetes alarms that can predict shocks
Integrated IT software across all care services – single set of records with single point of access
Get health records off GPs
Widen use of „attend anywhere‟ – saves 150 miles round trip for 5- 10-minute appointment
Health and social care IT systems need to merge – all professionals need access
Motion and bed sensors at home
Diagnosis through technology instead of attending GP
Better adoption of tech – single point entry (once only for data)
Wider use of community alarms to prevent move to long term care or hospital admissions
Wristband tech reduces falls! Reducing falls reduces costs of repairing hip fractures which can often lead to end of life
Danger of assuming access to tech, i.e. online mental health services, only on PC not mobile
GREENSPACE - RECREATION AND SOCIAL PRESCRIBING PRIORITIES Other issues raised Walking groups, etc… promoted by all healthcare professionals – tackles both health and loneliness
Don‟t assume it‟s only older people that need support
Better use of green spaces and organisation of activities for all
GPs to social prescribe – using tech, i.e. ALISS, to find appropriate services
Long-term funding for third sector voluntary services
Work with the third sector
Health professionals to take social prescribing seriously
Make greater use of innovation already in practice, e.g. helping hand service, good morning service
Greater use of volunteers in signposting service
Accessible cycles – trikes, pedal power
MULTI-DISCIPLINARY HUBS PRIORITIES Other issues raised Designed to serve public and not professionals – flexible opening hours
Easily accessible information and rapid access to relevant support/treatment
GP should be at the heart of the hub, but with shared responsibility for care & sign-posting
Include welfare experts – reduces stigma to have experts in the hub
Available at all stages / for all age groups
Secondary care psychologists assess persons in health hubs at primary visit
Sign-posting for health and social care for life‟s journey
SOCIAL ISOLATION PRIORITIES Other issues raised Link workers create links between client and community
Use all available resources – community, third sector, library, online
Don‟t assume it only affects older people – many groups suffer from social isolation
More interaction between locals to ensure neighbours are included in social activities
Good digital connectivity is essential
Inter-generational projects / befriending projects
GPs/healthcare signposting to relevant organisations
Rural areas – not to be secluded and more investment in all aspects of daily living and transport
Third sector great for preventing isolation
Appropriate housing
Ensure access to activities for all (local)
Tea dances, bingo! Intergenerational football memories, farming memories
HEALTH AND SOCIAL CARE INTEGRATION PRIORITIES Other issues raised Improve information sharing across all services
Include third sector in service planning
Care coordinators/health care assistants mean single point of contact
Everyone involved needs to grow up! Stop the turf wars and adapt to change
Social care should be removed from local authority and placed into NHS control
Third sector extremely important
Communities‟ engagement – windfarm money, use wisely to support integration
Cultural integration
Issues around differing boundaries of NHS boards and Councils (locality wise)
Dunfermline
NB: Dots represent how the participants rated the ideas at the end of the day. Each had 10 sticky dots to place next to their top priorities across the themes.
PHYSICAL ENVIRONMENT AND WELLBEING Encouragement and education to use physical environment
How can GPs improve support of access to activities with a financial barrier (e.g. swimming pool)?
Incentives for healthy behaviour (free gyms, cheap sports club membership)
Social prescribing (e.g. park run, lakes providing free activities)
Increased information and funding for groups of people being active together, e.g. walking groups, bird watching, outside gyms and other outside activities
Social prescribing by GPs should have a focus on young people
Information and awareness raising of what is available in terms of physical environment across multi-media platforms, including TV
How can we improve awareness of healthy eating? More information is needed especially in deprived areas
COMMUNITY SERVICES More local decision making
Better joined up decision making
Local issues informing national priorities
More co-location of facilities
Multi-use community facilities (including new-build schools)
Integrate schools and other statutory services into healthcare
More engagement and consulting with patients. *Listening*, find out what people want
Sustained relationships with health staff who know individual people
Better informed communities (not just online)
More pop-up health opportunities, to include access to records and referral to appropriate services
Mental health should be core / integrated
Future of school nurses? – Integrated into community care (school pupils, elderly, new mum, etc…)
Cradle to grave support
Support for carers
PREVENTION How does the Health and Sport Committee work across portfolios (transport, planning, education committees) on cross-cutting issues?
What is the role of public health/education (vaccination, access, food)?
How can money shift to primary care? It should move from acute sector
How does the Scottish hold industry to account on:
-Food, air pollution, consumables
-Health warnings
-Culture?
Mental health and schools - what role should primary care play?
- Links into third sector
- Links into secondary care
- Mental health professionals in schools
Focus on early years (0 to 3 years old) to reduces ACEs. Money and promotion for :
-Health history
-Breastfeeding
-Health visitors
- Midwives
-Link workers
-Training for parents
Universal health MOT
Screening - what ages?
Cost effective
Gender specific
Subsidised healthy food - targeted, free fruit
More healthy school meals and more activity in schools
Community hubs that are easily accessed
-Nutrition
-Cooking classes (parents and children)
Regulation
-Advertising (e.g. McDonalds)
-Cost of healthy food
How to encourage healthy work places?
-Mental and physical health
-Role of companies
-Role of NHS
Access to sport for everyone - linking with third sector
Drug procurement
How can we stop the influence of private companies (e.g. baby milk)?
Inequality and poverty require targeted interventions
Personal responsibility - how people can make good choices
How can we reduce burden?
Everyone should do prevention
ACCESS Why do waiting lists for CAMHS not improve (recurring issue)?
Why do all waiting lists not improve? Workforce related?
How can we keep newly qualified doctors in Scotland? Can the Board of GPs send a doctor anywhere in Scotland or can they just leave and go abroad?
Effective triage for primary care services
- Finding appropriate treatment for ailments
- Technology
- Is everyone on the right waiting list?
How can we improve access and reduce costs? (use of technology)
Development and improvement of online access (standardisation)
-Bookings
- Prescriptions
-Blood test results
Consistency of access for demographics:
- same approach of access regardless of area or GP surgery
- standardisation
How can we break generational prejudices to move forward? (Trusting technology/online information)
Flexibility of appointment systems, out of hours and weekends (non emergency) to fit with flexible lifestyles and working hours
TECHNOLOGY AND INNOVATION Centralise the database of health records
Shared electronic patient record (with a login and password) available for everyone but not mandatory
Need for a consistent platform across health services (e.g. test results, correspondence) and primary care linking in with secondary healthcare
Overhaul of IT systems - join information together
DNA profiling of patients/blood tests: prevention through technology
Research into genome testing: how could this be possible?
Can I email my GP? We can already do so much online already. We should have the option of technology
How is the Scottish Government helping people email healthcare professionals? Only mean of contact at the moment is phone calls
What about letters, skype/video prescriptions?
Can apps be used? Smart workshare with GP, health related apps
If people don‟t have online access for appointments, we need to improve the types of access
Inverurie
NB: Dots represent how the participants rated the ideas at the end of the day.Each had 10 sticky dots to place next to their top priorities across the themes.
MULTI-DISCIPLINARY HEALTH Located in communities and existing health clinics
How do different professionals work together?
Seeing the right people who know about your condition
Pointing people in the right direction
Is there adequate connection between professionals and if not, how do we create it?
Removing or upskilling the receptionist so they have the knowledge to triage an individual
What is the right mix of professionals or disciplines in a location?
Able to deal with local demand
MENTAL HEALTH Increase availability and signposting
Effective engagement
Fast track support in schools
“Emergency” service
Post traumatic support
Involvement of places of worship and social clubs
More mental health nurses
Loneliness support
Prevention for dementia
Test for dementia – M.O.T – early detection
Signposting to appropriate and empathetic approach
Support in school – mental health stronger part of teacher training
Prevent overuse of drug prescriptions in mental health
Communities
Straight forward awareness building about mental health suppor
INFORMATION & EXPECTATION MANAGEMENT Do the primary and secondary school curricula provide basic health care system information, i.e. not Active Kids‟ information but actual routes to care and when to use what services?
Information delivery - how to inform the public about primary care services?
Social Media for information dissemination
NHS consulting with communities
Public health campaigns should have more focus
Industries should have more responsibility – TV/Radio messages displayed
Advertising
Maps for services so you can navigate the primary care system
Parental responsibility
HEALTH STAFF WELLBEING & WORKFORCE PLANNING Staff ratios impact on stress – the higher number of patients per health professional, the greater level of stress staff will feel
Management which understands the emotional needs of staff
Accessibility to HR support
Adequacy of breaks and presumption against regular overtime
Good work/life balance
Creche for children of Primary Care staff
Peer to peer support
Recruitment
Encouraging Young people to get into the health sector
Career development for health professionals
Staff forward planning (supply and demand)
Being listened to. Staff being asked about their opinions and concerns before change occurs
SELF-CARE, HEALTHY LIFESTYLES & ENVIRONMENT Alternative therapies to stop over reliance on pharmaceutical drugs
Personal counselling to assist a diagnosis
Greater awareness to one‟s own health and impact on society (reducing the burden)
How to create change and educate society to take more responsibility for their health?
Education messages on social media – substance abuse, healthy eating, etc…
Incentives to make healthy choices
Encouraging self-monitoring (blood pressure, cholesterol etc…)
How do we turn bad habits into good ones?
Healthy food in food banks/ subsidies for healthy food
HEALTH IN THE COMMUNITY How do we implement social prescribing?
Increase social activities
Local access to health care
Increasing home care
Development of barrier free housing
Safe cycling and walking routes
NHS Netflix: Health Education TV programmes
Allotments to encourage growing of healthy food and inter-generational cooperation
USING INFORMATION & RESOURCES TO MANAGE PRIMARY CARE Monitoring effective provision and use of prescription drugs
Create universal electronic records system
Greater use of patient records to plan future services
Use of genetic testing for preventative care
Putting right resources in the right places
MOT Health Checks – don‟t wait until it is too late!
USING TECHNOLOGY Wearable technology for older people to encourage exercise and remember to take medication
Video conferencing for appointments
Greater use of patient records to plan future services
Social media for communication
Health information shared with relevant professionals
Educational adverts on social media
Greater use of technology to monitor conditions like high blood pressure and diabetes
Use of technology in elderly homes – see Fit Homes Project in the Highlands
Consider the digital divide and support people to use technology
Digital appointment booking
Go Anywhere Technology – support people when they are on holiday or living and working in different regions and authorities
HOME SUPPORT Keep people at home with care where possible
How many residential care spaces can we afford?
Can volunteering help?
Parental leave to care for older parents – the reverse of maternity and paternity leave
Collective Care – reverse of having care in home and having 4 carer visits a day and family support to being in a homely support environment where 1 person cares for 4 people
Local provision of residential care
FUNDING Accountability – hold trusts to account
Wastage – ring-fence money and resources accordingly
Use resources effectively
Too many managers band 7 plus
Ring-fenced taxation to go specifically to NHS funding: aim to have spending profile similar to that of Europe
Introduce shared responsibility levy based on excess profits following the introduction of minimum unit pricing
Know how funding is spent: where are the cuts and the shortages
Prioritisation
Cut out duplication
Unnecessary repeat prescriptions: not just drugs but equipment too: monthly orders rather than reduce/reuse
Top up care - pay a little extra for care, e.g. dentist
Publicise costs of primary care
Active life style rebate
Annexe D- Scottish Government Public Consultation 2015; Healthier Scotland
In 2015 the Scottish Government undertook an initiative to seek views from the public on what a healthier Scotland would look like. The Healthier Scotland Conversation asked three questions:
What support do we need in Scotland to live healthier lives?
What areas of health and social care matter most to you?
Thinking about the future of health and social care services, where should our focus be?
The aim was to engage and speak to as many people as possible, particularly those whose voices aren't heard as often. Over 9,000 people took at 240 events across the country. The Conversation reached over 360,000 people through social media channels.
The findings were grouped into five themes:
Leading Healthier Lives
Wellbeing and Connected Communities
Person-Centred Care
Social Care and Caring
A Responsive and Seamless Journey of Care
Under a responsive and seamless journey of care the summary report Creating a healthier Scotland - What matters to you noted:
Many of you were unhappy with the length of time it took to get an appointment, particularly if you wanted to see a specific doctor. Long waiting lists to see specialists was another issue, with many comments about delays in accessing mental health support.
While there was usually recognition of increasing demand for services and the impact that has on waiting lists, you also reported a lack of communication about how long you would need to wait and what other support was available in the meantime.
You told us you want more flexible services, with appointments that fit in with your lives, including work and caring commitments. Extended opening hours, including evening and weekends, would prevent you having to take time off work for your own appointments or for the people you look after.
Other suggestions included booking appointments or ordering repeat prescriptions online, emailing staff, drop-in sessions allowing you to see a health professional other than your doctors, using computers or smart phones for online services such as Skype consultations. These were highlighted as ways to take the pressure off primary care, reduce physical access issues and support self-management.While there was general support for eHealth development, some were worried that this could exacerbate inequalities, as not everyone has access to technology or the internet, or the skills to use them. We also heard that some people have a preference for face to face contact.
There was interest in a move towards more multi-disciplinary care. Although your first point of contact with health services is normally your GP, you told us that it didn't need to be, and that you had received really good care from other professionals including nurses, pharmacists, community link workers and Allied Health Professionals (AHPs).
We heard from AHPs including physiotherapists and occupational therapists who talked about how they could take the pressure off GPs and prevent people from losing their independence or developing long-term conditions. Accessing support for multiple issues in one place, was suggested as a way to reduce the need for multiple appointments in different locations.
The Survey
Introduction
The Scottish Parliament's Health and Sport Committee is interested in hearing your views on primary care in Scotland. Please note that the questions may not reflect Scottish Government direction or policy. So what is primary care? Primary care is often centred around your local health centre. It includes your visits to your GP, but also to your dentist, the optician, podiatrist or physio, for example. Community nurses, midwives and pharmacists also work in primary care, as do community links workers. GP practice receptionists and practice managers are also members of the team, but are usually employed directly by the GP practice rather than the NHS. By completing this short survey you will be providing the Parliament's Health and Sport Committee with some insights into public understanding of primary care, as well as what you think is important regarding you and your family's healthcare - outside of hospital care - into the future. You can skip any question, but please click the 'submit' button at the end of the survey, as even partial responses will be helpful.
 The Scottish Parliament
The Scottish Parliament The Scottish Parliament
The Scottish Parliament The Scottish Parliament
The Scottish Parliament The Scottish Parliament
The Scottish Parliament The Scottish Parliament
The Scottish Parliament The Scottish Parliament
The Scottish Parliament The Scottish Parliament
The Scottish Parliament The Scottsh Parliament
The Scottsh Parliament The Scottish Parliament
The Scottish Parliament